The entire length of the gastrointestinal tract is lined with mucous membrane, which plays a role in the digestion and absorption of various substances. This structure is very vulnerable and requires certain protection to maintain its integrity and normal functioning.
For this purpose, the gastric mucosa is endowed with accessory and mucosal cells, and goblet cells work similarly in the intestine. These cells secrete mucus, which envelops the mucous membrane, protecting it from acids, alkalis, and mechanical injuries from coarse food particles.
general information
Normally, the presence of mucus in the digestive system in moderate quantities is a physiological process. The secretion is necessary to protect the intestinal mucosa from toxins and mechanical injuries from dense fecal matter or dietary fiber, and to facilitate bowel movements.
Mucus is constantly secreted in the digestive system, since the adult body forms a bolus of food in real time and removes it through the anus to the outside. These are dead epithelial cells. Inflammation or intoxication changes the consistency of the secretion, its quantity, composition, and the result is:
- violation of the integrity of the mucous membrane, cracks;
- bleeding;
- hemorrhoids are formed;
- mucus plugs form;
- impurities of various types appear.
Depending on the pathology, the secretion of the intestinal glands may differ in color and shape:
- white mucus in the stool or its transparent version in large quantities indicates pathological changes in the distal parts of the intestine;
- yellow – the result of taking antibiotics, the formation of hemorrhoidal cones, polyps;
- gray – problems of the descending department;
- green – bacterial infection;
- pink – suppuration;
- black – tumor process;
- small flakes of undifferentiated color – pathology in the small intestine;
- admixture of blood - erosive and ulcerative processes of the mucous membrane, cracks, hemorrhages.
What is mucus in stool
The wisely designed human body constantly secretes mucus to protect tissues and organs. An oily, jelly-like substance of white or transparent color is formed by the secretion produced by the intestinal glands. Part of it consists of epithelial cells, leukocytes on the surface of the mucous membrane. This secret plays an important role:
- protects against the influence of toxic components of feces;
- protects the intestinal lining from the mechanical effects of coarse food fibers;
- prevents chronic constipation due to difficult passage of stool.
The adult body constantly produces and eliminates viscous contents - this is normal. Thanks to mucus, stool can easily move through the intestinal tract and exit through the anus. With inflammatory changes in the intestines, serious problems arise with the release of lubrication. As a result:
- in the absence of cracks, damage to the mucous membrane, bleeding, and development of hemorrhoids;
- Serious pathologies are possible with excessive secretion production;
- A change in the color of the discharge indicates the presence of problems that require treatment.
Causes of pathology
The trigger for hypersecretion of mucus in men and women can be for different reasons: lifestyle, eating habits, diseases. The most common causes of secretion are:
- drinking water with impurities dangerous to the mucous membrane of the food tube;
- rough, poorly digestible food;
- fasting or dieting;
- hypothermia;
- constant use of medications;
- swimming in cold water;
- alcohol;
- stress;
- smoking;
- unwashed vegetables, fruits;
- unbalanced diet.
Stool and mucus cause diseases:
- irritable bowel syndrome with vomiting, dyspepsia, constipation;
- imbalance of intestinal microflora;
- tumors of the gastrointestinal tract;
- Crohn's syndrome;
- sensitization of the body;
- infections;
- inflammatory processes.
Discharge in stool may be the result of:
- helminthiasis;
- viral pathologies;
- exacerbations of respiratory diseases;
- hemorrhoidal disease with complications;
- peptic ulcer of the stomach and duodenum;
- intestinal polyposis;
- inflammation of the pancreas, large intestine;
- colitis of spastic origin;
- diverticulosis;
- proctitis and paraproctitis;
- cystic fibrosis.
Possible complications and diseases
Dysentery . This disease may be accompanied by symptoms:
- hyperthermia;
- temperature increase;
- nausea;
- feeling of weakness;
- vomit;
- severe abdominal pain.
If green stool in an adult persists for several days for no apparent reason, and the above symptoms appear, you need to consult an infectious disease specialist. If the phenomenon is accompanied by a putrid odor, sudden weight loss, and diarrhea, this state of affairs already indicates the presence of E. coli and other pathological microorganisms.
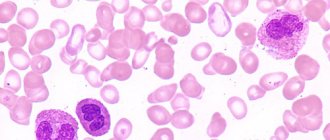
Dysbacteriosis . It occurs not only in children, but also in adults. Accompanied by belching, bloating, and upset bowel movements. Increased gas formation and green stools in adults are also present. All these symptoms are caused by a violation of the microflora. As a result, beneficial microorganisms gradually die and are replaced by pathogenic microflora. During the exacerbation of the disease, a high number of leukocytes is observed. As a result of such changes, the intestines cannot digest food normally. This provokes its fermentation and rotting. Components are released that cause green poop to appear.
Clinical manifestations
Symptoms of pathological secretion of the glands of the mucous membrane of the digestive system are varied, since they are caused by many reasons. But the main clinical, visually distinguishable manifestation is still the color and consistency of the mucus.
White mucus in stool
Viscous white discharge, reminiscent of jelly, in the stool of an adult indicates inflammation of the rectum, dysbiosis, mycosis of the rectum, irritation of the mucous membrane by microorganisms or poorly digested foods. Rough food or infection can provoke cracks, an allergic reaction, and exacerbation of chronic gastrointestinal diseases.
Mucus instead of feces
If instead of formed feces during defecation, mucus plugs that imitate snot come out of the anus, this means the inability of the digestive system to correctly form a bolus of food and pass it along the entire length of the intestine. Excessive irritation of the mucous membrane causes hypersecretion in a volume that the anal sphincter is unable to hold. The flow of mucus is accompanied by abdominal pain and hyperthermia.
The cause may be: multi-day constipation, intestinal obstruction, obstruction of the intestinal lumen by parasites, microorganisms, tumors, polyps, volvulus, rectum ulcer, foreign object in the rectum.
Mucus with blood
The most serious situation is bloody discharge from the anus, which indicates a violation of the integrity of the intestinal mucosa as a result of erosive and ulcerative processes or tumors. Blood in the stool may be a sign of hemorrhoids. The danger lies in the development of uncontrolled bleeding, anemia, and cancer metastasis.
Yellow slime
The yellow color of the discharge indicates the presence of pus in the stool, the development of inflammation, the addition of secondary flora against the background of polyps, hemorrhoidal disease, dysbacteriosis, and intestinal infections.
Transparent slime
This is the safest option for hypersecretion of the glands of the mucous membrane of the digestive system. The reasons may be smoking, taking medications, coffee, hunger. The most dangerous is the development of spastic or membranous colitis. An examination by a specialist is required.
Pink slime
Pink secretion is a dangerous situation that most often occurs due to liver cirrhosis, peptic ulcer, Crohn's syndrome, allergic colitis, intestinal varicose veins of various locations, and diverticulosis.
Black slime
The most common cause of black secretion is taking vitamins or medications containing iron. But in the worst case scenario, this is a sign of a malignant neoplasm, therefore an urgent comprehensive examination is necessary in this case. A change in the color of mucus in the stool is associated with severe bleeding.
Brown slime
Most often, a brown secretion indicates insufficient pancreatic function or dysbacteriosis. However, sometimes this coloration of mucus can be caused by direct entry of mucus from the nose into the intestines during acute respiratory infections or acute respiratory viral infections, accompanied by a runny nose. In addition, a brown tint may indicate a secondary infection. Pus in the stool can also turn brown.
What foods and habits contribute to stool coloration?
If green feces were noticed in an adult once, this does not mean that it is necessary to sound the alarm. Often the color changes due to the foods consumed. For example, with excessive consumption of certain grains, which are difficult for the body to digest, the stool may turn green, and this phenomenon persists for several days.
To digest grains that have a dense shell, the body needs to produce bile in large quantities so that the process of breaking down food is more productive. The enzyme promotes this and produces greenish-colored stool.
Some products contain special pigments that can change the color of excrement. This factor is associated with an excess of iron in food. Therefore, this phenomenon should not be regarded as a disease.
Color may be affected by:
- Frequent consumption of spinach, cucumbers, sorrel, lettuce, dill, and other foods that have a pronounced green color.
- Eating caramels, marmalade and other foods that contain a high level of food coloring. They can even cause stool that is dark green in color.
- If foods contain chlorophyll, the color of the stool will also change. After eating seaweed, this phenomenon can persist for up to 3 days.
- Red meat, fish, and red beans in some cases also contribute to the coloration of stool.
Pigments tend to persist in the human body for up to 5 days. That is, it is possible that even after a person stops eating all of the above foods, the color of the stool will still remain unchanged.
Important: If an adult notices that he has green poop, and the phenomenon is accompanied by mucus discharge, then this becomes a reason to think about his health. This symptom may already indicate that there are problems in the functioning of the gastrointestinal tract.
The reasons for the appearance of green stool are usually divided into two classifications:
Let's look at them more specifically.
Diagnostics
A change in the color of the secretion of the glands of the mucous membrane of the digestive tube requires consultation with a qualified specialist: a therapist, gastroenterologist, proctologist, infectious disease specialist.
It is necessary to donate blood for a detailed analysis and conduct a bacteriological examination of stool. Sometimes a consultation with a surgeon or oncologist may be necessary. In any case, the clinical and laboratory examination of the patient includes:
- OAC, OAM – screening of the patient’s general condition;
- biochemical tests: blood for sugar, cholesterol, tumor markers, antibodies to hepatitis viruses, and so on;
- coprogram;
- endoscopic instrumental research methods: FGDS, anoscopy and others as recommended by a doctor;
- Ultrasound of the abdominal cavity and pelvis;
- CT.
If this minimum is not prescribed:
- sigmoidoscopy, colonoscopy, irrigoscopy;
- MRI;
- blood electrolyte balance.
What diagnostic measures are prescribed?
If greenish-colored stool appears in an adult, the doctor will definitely prescribe examinations and studies.
- Coprogram. Thanks to this technique, a specialist can identify what is in the microscopic composition of stool. The method also allows you to study the chemical composition. Basically, these factors are enough to understand why the stool is green.
- Other laboratory methods include blood and urine analysis, bacterial culture and microscopic examination. The latter is carried out if parasites are suspected. During the procedure, specialists use a polymerase chain reaction, during which DNA of the life cycle is isolated. If a person's stool is green, the cause may well be parasite infection.
- Sowing tank Allows you to identify the causative agent of intestinal infection, the presence of bacteria, and the state of the microflora. The biomaterial is placed in a special environment, where the causative agent of the disease is determined.
Features of treatment
Therapy for pathologically altered secretion of the mucous membrane of the digestive system is subject to correction by general and special methods. General ones include the nutritional system, lifestyle changes, the use of systemic medications, and background traditional medicine. The most common pathologies are treated with separate complex regimens.
Balanced diet
The diet should be based on fractional meals with meals every three hours. A serving should not exceed 200 g in volume. Food products are selected on an individual basis, taking into account intolerance to individual components and susceptibility to allergies. The drinking ration is calculated per kilogram of weight, at least 1.5 l/day. Steaming, baking, boiling. Fatty and salty foods should be avoided.
| Allowed | Forbidden |
| Tomatoes, cucumbers | Carrots, cabbage (all options) |
| Pasta | Potato |
| Whole wheat bread | Pumpkin |
| Fermented milk products: kefir, fermented baked milk, yogurt, matsoni | Corn |
| Milk | Beet |
| Various grains: oatmeal, buckwheat, millet | Bananas |
| Dietary meat, fish, seafood | Coffee |
| Soybeans, legumes | Kiseli |
| Fruits, preferably with vitamin C: citrus fruits, green apples, kiwi | Sweet soda |
Medicines
Systemic therapy to relieve hypersecretion of digestive mucus aims to stabilize and maintain the function of the digestive system. For this purpose, pre-, pro-, dysbiotics, lacto- and bifidobacteria are used. This helps restore the natural intestinal microflora. In addition, they use:
- laxatives if the cause of hypersecretion is constipation;
- diarrhea is treated with lactulose derivatives;
- pain is relieved with antispasmodics;
- immunity is supported by immunostimulants and immunomodulators;
- intoxication is removed with sorbents or activated carbon, drugs based on it.
Diseases that lead to green stool
The most common causes of green stool are poisoning, dysbiosis and fermentative dyspepsia.
Poisoning is an acute digestive disorder, which is manifested by fever, diarrhea with green feces, vomiting and nausea. The causes of poisoning may be:
- low-quality products, which lead to the proliferation of pathogenic microflora;
- poisonous mushrooms;
- intoxication of the body with toxic substances found in alcohol, medications, plants, etc.
In case of poisoning, the stomach should be emptied of contents by lavage, general intoxication of the body should be eliminated with the help of medications and water balance should be restored.
Fermentative dyspepsia is a digestive disorder caused by a large amount of carbohydrates with coarse fiber in the diet, as well as a decrease in the amount of gastric juice.
The appearance of dyspepsia is also accompanied by poor chewing of food, eating at a fast pace, and drinking carbonated drinks. Symptoms of the disease appear as follows:
- bloating;
- feeling of transfusion and rumbling in the stomach;
- constipation and diarrhea;
- light green stool.
To eliminate discomfort in the gastrointestinal tract, it is necessary to adhere to a protein diet for 7-10 days with the exception of vegetables and fruits, since foods with a large amount of fiber (white cabbage, apples, etc.) provoke increased gas formation.
Dysbacteriosis is a violation of the digestion of food in the intestines due to a lack of lactobacilli and an excess of putrefactive bacteria.
The development of dysbiosis is accompanied by abdominal disorders, bloating, and abdominal pain. In addition to the change in the color of the feces to yellow and green, you can see many undigested pieces of food in the stool.
To eliminate symptoms, pre- and probiotics are used to replenish beneficial lactobacilli, and you should also follow a special diet to maintain normal microflora.
Folk recipes
There are no special herbs or plants to normalize mucus production in the digestive system. However, herbal remedies that are used to treat any pathological changes in the digestive system are effective. They are loyal to stomach acidity and bile production. Here are some of them:
- ginger drink: the root of the plant (1 cm) is crushed and brewed with a glass of boiling water, cool, add a spoonful of honey, lemon juice, drink 50 ml three times a day before meals;
- herbal tea from chamomile, calendula, yarrow in equal parts (teaspoon) per glass of boiling water - drink throughout the day;
- kefir with honey: a tablespoon of buckwheat flour per glass of kefir, half a teaspoon of ginger, a spoonful of honey - the mixture is infused for 8 hours in the refrigerator, stirred, and drunk instead of breakfast.
All prescriptions are agreed in advance with the doctor.
Treatment regimens for common pathologies
Treatment of hypersecretion of digestive mucus depends on the type of pathology on an individual basis. It is not recommended to change the schemes.
Inflammatory diseases
Altered mucus is most common in irritable bowel syndrome. They use antispasmodics (Trimedat, No-Shpu, Duspatalin), antidiarrheals (Loperamide, Imodium, Smecta), laxatives (Duphalac, Buscopan), antidepressants (Fluoxetine, Imipramine, Citalopram), probiotics (Enterozermina, Linex), prebiotics (Fervital, Lactulose , Lactofiltrum).
In second place is hemorrhoids. A combination of anti-inflammatory suppositories and liniments (Natalsid, Relief, Proctosan), hemostatics (Ditsinon, Vikasol), laxatives (Mukofalk, Bisacodyl), analgesics (Anestezol, Analgin), venotonics (Detralex, Troxevasin), anticoagulants (Heparin, Prednisolone) are used. Read more: how else to treat hemorrhoids at home
For the treatment of diverticulum, antibiotics (Flemoxin, Cefoxitin), analgesics (Mesacol), antihistamines (Suprastin, Tavegil), laxatives (Normaze, Mucofalk), antispasmodics (No-Shpa, Meteospasmil) are used.
Worm infestations
Intestinal obstruction by helminths and parasites is treated with the use of anthelmintic drugs (Nemozol, Dekaris, Fenasal, etc.), choleretic agents (Allochol, Holosas), hepatoprotectors (Karsil, Ovesol), sorbents (activated carbon, Enterosgel), vitamins (Supradin), enzymes (Creon, Pancreatin).
Dysbacteriosis
Imbalance of intestinal microflora is corrected with antibiotics (Amoxicillin, Oxamp), antifungals (Fluconazole, Flucostat), bacteriophages (Sextaphage, Intesti), sorbents (Polysorb), probiotics (Bifilakt) and prebiotics (Lactofiltrum, Fervital), enzymes (Creon), immunomodulators (Immunal, Echinacea).