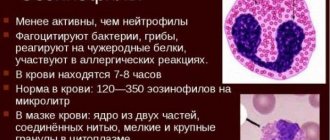
Eosinophils represent one of the groups of leukocytes (white blood cells). Their production is activated when a foreign protein structure enters the body. The number of cells is determined during a routine general blood test, and not only the absolute value (the number of pieces in a unit of blood) matters, but also the ratio to the total number of leukocytes (it is expressed as a percentage). When our immunity starts working intensively and independently tries to defeat the disease, eosinophils in the blood test are increased. However, you should know that not every increase or decrease in the level of these blood cells indicates a pathological process. However, first things first.
Role and functions of cells
Eosinophils get their name because of their ability to stain with the acidic dye eosin, with which the bodies are isolated in a smear for further counting. They are produced by the bone marrow and mature in about 9 days. Later, eosinophils enter the bloodstream and circulate in the body in case of penetration of foreign proteins. Cells are capable of:
- extravasation - penetration through the walls of blood vessels;
- chemotaxis - movement towards pathological foci (can change position chaotically);
- phagocytosis - act as microphages (they absorb relatively small cells, toxins, particles).
After 12–24 hours, the bodies move into peripheral tissues. The highest concentrations are observed on the mucous membranes, submucosal layer of the stomach wall, and small intestine. Here the bodies continue to perform their protective functions, waiting for a collision with foreign genetic material. The proportion of circulating cells is miniscule. For each eosinophil there are up to 300 precursor cells that mature in the bone marrow and from 100 to 300 tissue bodies. Differing from neutrophils, which react against any infections, as well as from actively phagocytic monocytes, eosinophils are weakly involved in standard protective reactions. Their main functions are recognized:
- cytotoxic qualities (can produce substances that have a detrimental effect on some parasites and on the body’s own cells);
- stimulate the sensitivity of IgE-specific receptors (which causes severe allergic reactions, including the immediate type);
- can absorb and release allergy mediators (activate or suppress manifestations of hypersensitivity);
- involved in eliminating the consequences of allergies;
- participate in antitumor immunity.
In peripheral tissues, protective bodies live up to 12 days. Then they are replaced by new mature cells.
Normal levels of eosinophils in the blood
The cell level is determined during a general blood test with a leukogram. In a conventional study, the results indicate only the total number of leukocytes, without distribution into groups. The leukocyte formula norms are almost identical for adults and children, representatives of both sexes.
Table - Leukogram norms for adults
| Group of cells | Share, % | Absolute indicator, 10⁹/l |
| Band neutrophils | 1‒6 | 0,04‒0,3 |
| Segmented | 48‒75 | 2,0‒5,5 |
| Eosinophils | 0,5‒5 | 0,02‒0,3 |
| Basophils | 0‒1 | 0,0‒0,065 |
| Lymphocytes | 19‒37 | 1,2‒3,0 |
| Monocytes | 3‒11 | 0,09‒0,6 |
The eosinophil count in an adult is considered normal from 0.02 to 0.3*10⁹/l. For children, the upper threshold is slightly higher (0.7*10⁹/l). The percentage of cells among white blood cells varies depending on the age of the patient.
Table - Normal percentage of eosinophils in children
| Age | Share, % |
| Up to 2 weeks | 1‒6% |
| Up to a year | 1‒5% |
| Up to 2 | 1‒7% |
| Up to 5 | 1‒6% |
| Until 6 | 1‒5% |
To assess the blood picture in children, only a percentage indicator is often considered. The absolute value (MON abs.) in young patients significantly exceeds the norm for adults, which is only rarely associated with diseases.
It is typical that the number of peripheral blood cells changes throughout the day. Minimum concentrations are observed in the morning. The values increase after physical activity and eating food. The maximum is reached when a person falls asleep (before midnight), and then gradually decreases.
Eosinophils below normal
If the absolute number of eosinophils per milliliter of blood falls below 200, the condition is interpreted as eosinopenia.
Eosinophil counts become low in the following cases:
- In severe purulent infections, including sepsis, when the population of leukocytes shifts towards young forms (band and segmented), and then the leukocyte response is depleted.
- At the beginning of inflammatory processes, with surgical pathologies (appendicitis, pancreatitis, exacerbation of cholelithiasis).
- On the first day of myocardial infarction.
- In case of infectious, painful shock, when the formed elements of the blood stick together into mud-like formations inside the vessels.
- For poisoning with heavy metals (lead, copper, mercury, arsenic, bismuth, cadmium, thallium).
- For chronic stress.
- Against the background of pathologies of the thyroid gland and adrenal glands.
- In the advanced stage of leukemia, eosinophils drop to zero.
What does the eosinophil count indicate?
An increase in the number of cells above normal is called eosinophilia. This is a laboratory term that is considered a marker of certain diseases. It is impossible to make a diagnosis based on the results of the CBC. A full examination will help determine the nature of the disease. Based on the percentage of eosinophils, three degrees of severity of the condition are distinguished.
Table - Types of eosinophilia
| What will the doctor say | Compliance in numbers | What does it mean |
| Slightly elevated | To 10% | Mild degree of eosinophilia (physiological processes, disturbances in preparation for analysis, initial stages of pathology development) |
| Promoted | Up to 15% | Moderate degree (allergies, infections, early stages of cancer progression) |
| High | More than 15% | Severe (serious allergic reactions, extensive infections, autopathologies, cancer) |
The circulation of a large number of eosinophils in the peripheral blood almost always means stimulation of their production in the bone marrow, since in a short time the cells pass into the tissue bed. Active synthesis of bodies can be provoked by:
- pathogenic microflora;
- encounter with allergens;
- parasitic infestation;
- the presence of atypical own cells;
- tissue breakdown;
- changes in bone marrow function.
Doctors refer to the most common causes that are relevant for children and adults with the abbreviation POKAA. This means that eosinophilia is most often caused by:
- parasites;
- tumors;
- collagenoses;
- allergies;
- asthma.
It has been proven that the severity of deviations in OAC results directly depends on the intensity of development of the underlying pathological process. The more complex the disease, the higher the level of eosinophils will be found in the patient. Based on cell indicators, you can monitor the effectiveness of eliminating causes. Analysis deviations can cause some physiological changes in the body, which you need to know when planning a laboratory visit:
- evening readings may exceed the norm by 30% (which is taken into account if the analysis is carried out urgently);
- consumption of large amounts of sweets, alcohol, protein foods of animal origin (it is better to exclude them when preparing for the study);
- the amount is slightly increased in the first days of menstruation, sharply decreases after ovulation (but does not go significantly beyond the normal limits);
- the analysis is influenced by medications (hormonal drugs, antituberculosis, anticonvulsants, antihistamines, diphenhydramine, papaverine, aminophylline, B vitamins, etc.).
Does eosinophilia have symptoms?
Deviations in blood tests always show signs of a causative disease. By themselves, they do not have specific symptoms or change the patient’s well-being slightly (it cannot be said that it was a violation of the blood composition that became the main prerequisite).
Table - Possible symptoms of eosinophilia
| Nature of the disease | Manifestations |
| Parasitic infestations | Weakness, digestive and stool disorders, loss of appetite, body pain, nausea |
| Tissue destruction | Symptoms of systemic inflammation (lethargy, fatigue, fever), local pain |
| Allergic reactions | Local swelling, rash, itching, cough, runny nose |
| Malignant processes | Lack of appetite, weight loss, pain, apathy, weakness, low-grade fever in the evenings |
What symptoms does it present?
Elevated eosinophils are not a disease, but one of the signs of a developing pathology. Symptoms depend on the nature of the disease that caused increased production of eosinophilic leukocytes:
- with parasitic infestations, nausea, vomiting, muscle pain and general weakness appear;
- allergic manifestations are accompanied by rashes, cough or runny nose, local or local swelling;
- malignant neoplasms are accompanied by loss of appetite, weight loss, weakness, and pain at the site of the tumor;
- inflammation and necrosis cause pain and fever to high levels.
Sometimes an adult develops short-term symptoms of deterioration associated with minor exposure to an allergen or mild poisoning. But more often, the symptoms of the disease increase gradually, worsening the quality of life and forcing one to seek medical help.
Cause for alarm is when the percentage of eosinophils in the blood is increased and the patient has significant signs of deteriorating health.
If eosinophilia does not cause deterioration in health, this does not mean that additional examination will not be required. Elevated eosinophils may be a temporary physiological abnormality or indicate the onset of disease. Additional tests will help identify developing pathology or confirm that the deviation arose under the influence of physiological processes.
Eosinophils in the blood are often elevated during allergies
Causes of eosinophilia
The main and most common prerequisite for an increase in the number of eosinophils is considered to be parasites. The combination of parasitic infestations and abnormalities in clinical blood tests occurs so often that doctors primarily consider the possibility of infection with worms. High levels of eosinophils may be due to the following diseases:
- ascariasis;
- filariasis;
- toxocariasis;
- schistostomiasis;
- amoebiasis;
- paragonimiasis;
- trichinosis;
- echinococcosis;
- malaria;
- opisthorchiasis;
- strongyloidiasis;
- enterobiasis.
Such reasons are relevant for adults and children. However, eosinophils are not always elevated in the presence of parasites in the body. The cell count does not change when infected with Ciardia Lamblia, but this development is considered more of an exception.
Eosinophilia, provoked by allergies, is accompanied by an increase in cell counts of more than 0.6 * 10⁹/l. In this case, the values do not exceed 1*10⁹/l. When the level is higher, other causes must be considered, since sensitivity reactions cannot provoke such significant changes. Eosinophilia accompanies:
- hay fever (hay fever) - allergic manifestations to flowering plants;
- bronchial asthma;
- allergic fasciitis and myositis - inflammation of the muscles and surrounding fascia;
- serum sickness - allergy to vaccines;
- rhinitis (runny nose);
- drug reactions;
- Quincke's edema;
- hives
A significant increase in the level of eosinophils in the blood requires a comprehensive examination for malignant diseases. Neoplasms may contain protective cells; such tumors have a more favorable prognosis. Eosinophilia accompanies the following types of cancer:
- nasopharynx;
- lungs;
- large intestine;
- stomach;
- uterus;
- thyroid gland;
- lymphatic system;
- bone marrow.
Specific tumor markers help determine the location of the malignant focus. Diseases of the hematopoietic system are diagnosed by bone marrow biopsy. Eosinophilia accompanies acute eosinophilic, lympho- and myeloblastic leukemia. The combination of abnormal blood flow with hepatosplenomegaly and lymphadenopathy may indicate Hodgkin's disease.
In case of serious tumors accompanied by tissue destruction, basophil levels also increase. The level of eosinophils is taken into account to monitor the effectiveness of therapy. Its increase may signal a relapse of the disease or the appearance of metastases.
Cell values rarely change with a cold. Their indicator should remain unchanged during pregnancy and menstruation, while the indicators of lymphocytes, monocytes and platelets may change.
Useful information: Cholesterol is elevated in the blood: 12 reasons, what it means, normal, treatment, how to reduce it in women and men (diet, foods, medications)
Autoimmune eosinophilia
An excessive concentration of immune cells in the blood can be caused by immune attacks on the body's own tissues. The autoimmune nature of the abnormalities is observed in eosinophilic syndrome. This disease is more common in young men and women and has a poor prognosis. The diagnosis is made if:
- the indicator exceeds 1.5*10⁹/l for longer than six months;
- there are no objective signs of allergies or the presence of parasites in the body;
- multiple lesions of internal organs develop.
Eosinophilic syndrome is manifested by increased body temperature, chills, decreased appetite, and weight loss. During the examination, an enlargement of the spleen and liver, damage to the heart valves, heart failure, and disturbances in the functioning of the central nervous system may be detected.
Eosinophilic myositis can be part of the syndrome described above or be an independent disease. It is characterized by a pronounced increase in the level of eosinophils in the peripheral blood. It differs from other types of myositis by the presence of rashes in the projection area of the affected muscle. Eosinophilic fasciitis is similar in manifestations to scleroderma, but it begins acutely, appears for the first time after unusual types of stress, and is corrected with the help of glucocorticoids.
Drug-induced eosinophilia
Many medications have side effects, including changes in your blood patterns. These include drugs used to treat infectious diseases:
- Penicillins;
- Cephalosporins;
- Doxycycline;
- Gentamicin;
- Streptomycin;
- Rifampicin.
Eosinophilia can be provoked by Allopurinol, Spironolactone, Ranitidine, Enalapril, Warfarin, Carbamazepine. Changes in indicators are observed after hemodialysis, radiation exposure, and administration of the hepatitis A vaccine.
Hereditary pathologies
Violations of indicators can be detected in newborns with genetically determined diseases. These include benign eosinophilia, familial histiocytosis, and congenital immunodeficiencies. As a rule, these disorders are detected soon after the birth of a child or in infants during the first year of life. Some chromosomal abnormalities may predispose to the formation of malignant tumors.
Idiopathic forms
Sometimes the reasons for changes in the blood picture cannot be determined. An example is constitutional eosinophilia, which is more often detected in premature infants. It goes away on its own as the baby’s weight normalizes.
With Loeffler's syndrome, the formation of single or multiple infiltrates in the lungs is observed. They form suddenly, resolve on their own, and the course of the pathology is considered benign. During an exacerbation, the level of leukocytes may increase, and the percentage of eosinophils increases to 70%. Loeffler's disease is also called endomyocardial fibrosis. The condition is accompanied by changes in the endocardium, valve damage, stenosis, a decrease in the volume of both ventricles, and the development of heart failure. The prognosis for patients is unfavorable.
Common causes in children
Eosinophilia occurs in newborns after Rh conflict with the mother, during intrauterine infection, infection with staphylococcus and fungi shortly after birth.
In children over 1 year of age, changes in test results may be due to an allergic reaction, atopic dermatitis, or allergies to medications. In school-aged children and adolescents, viral diseases (chickenpox, for example) and infection with worms are considered common causes. Deviations in the analysis can be observed for some time after the illness; they disappear after the body has fully recovered.
Despite the list of the most common causes, autoimmune diseases or malignant tumors cannot be excluded. To accurately establish the nature of the deviations, an examination will be required.
Interpretation of results
The interpretation of the results should be carried out by the attending physician who referred your child for a blood test. If the parents independently asked for a blood test, then deciphering the answer should be entrusted to a specialist. It may be located in the same place where the blood was donated, or you can contact your place of residence with a ready-made test result.
When eosinophils are elevated in a child and in an adult, this condition is called eosinophilia. Next we will look at situations where this is possible and why it occurs.
What to do in case of a “bad” analysis?
The doctor who ordered the study should read the results of the OAC. If a person passes the test on his own, violations should be addressed to a pediatrician (if this is a child) or a therapist. It is important not only to study indicators that are outside the normal range, but also to correlate them with the values of other blood cells.
Eosinophilia and elevated ESR may indicate a disease accompanied by an inflammatory process. High levels of eosinophils and low platelets accompany viral infections and bone marrow pathologies. Diseases of the hematopoietic system are indicated by an increase in the level of eosinophils and a change in hematocrit. Cells can be detected in biopsies and various biological fluids. This helps in identifying the place where toxins enter the body or the location of malignant tumors.
If there is a significant increase in eosinophil levels, you should take the CBC again. This will eliminate errors during the study or disruption of preparation for it. If violations are detected again, an examination should be started. If eosinophils are elevated, you need to take the following tests:
- blood biochemistry;
- general urine examination;
- feces for helminth eggs or blood for worm antigens;
- immunogram;
- liver tests;
- allergy tests;
- antinuclear antibody test;
- rheumatoid factor.
To clarify the analysis information, ultrasound of internal organs, CT or MRI, and fluorography of the lungs are performed. To exclude malignant diseases, tumor markers and a bone marrow or lymph node biopsy are prescribed.
Diagnosis of the disease
To get a complete picture of a person’s health status, it is first necessary to take a biochemical blood test; such a study can indicate the reason why eosinophils are elevated. Further, based on the results, it is necessary to conduct a number of further studies:
- Ultrasound examination of internal organs;
- Analysis of stool for the presence of parasites and their eggs;
- Analysis of urine;
- Tests to determine the functioning of internal organs (kidneys, liver, etc.);
- Fluorography of the lungs.
- Allergological studies (study of mucus, provocative tests, spirometry, puncture of interarticular fluid and other manipulations).
Is it possible to treat yourself
Any disease that causes deviations of eosinophils from the norm should be treated under the supervision of a physician. Even the obvious presence of worms in the body may not be the only problem. In addition, some parasites produce toxins with carcinogenic properties, and allergic reactions lead to autoimmune pathologies. If the risk is detected in a timely manner, it is possible to carry out the most effective and safe therapy and diagnose complications in the early stages. Self-medication and the use of folk remedies are fraught with delay in treating truly dangerous diseases that can threaten the patient’s life.
Is treatment required?
Eosinophilia is not a disease, but a sign of a developing pathology or temporary physiological deviation from the norm. What this means in an adult, doctors can only determine after additional examination:
- If the increase is a sign of illness, then the underlying pathology should be treated. After recovery or remission, the indicator will decrease.
- When eosinophilic granulocytes have increased due to medication or bad eating habits, after eliminating the provoking factor, the level will decrease on its own.
If eosinophils in an adult have increased due to physiological reasons, then the blood test should be retaken after 2 weeks. During this period, the excess amount of blood elements will be destroyed, and the number of eosinophilic cells will decrease to normal. If this does not happen, then a hidden course of the disease should be suspected.
FAQ
Question: What is eosinophil cationic protein? How and why is it defined?
Answer: A cationic protein is a specific substance that acts as a mediator for eosinophils and is released from their granules when immunoglobulin E comes into contact with allergens. The indicator is measured in blood serum. The value is important for diagnosing most types of allergies (food, contact, bronchial asthma, atopic dermatitis, allergic rhinitis), as well as for monitoring the effectiveness of therapy.
Question: Is it possible to get vaccinated if you have elevated eosinophils?
Answer: The issue of vaccination should be resolved with the pediatrician who is monitoring the baby. It all depends on age, the presence of anxiety symptoms, and individual characteristics. In children under one year of age, the blood picture is unstable. If at this time there are no signs of allergies, viral or parasitic infections, slight deviations in eosinophils are not considered a contraindication. During periods of active sensitivity reactions, accompanied by rashes and general poor health, it is better to refrain from vaccinations.
Question: What does a rhinocytogram result in which eosinophils are highly elevated mean?
Answer: A rhinocytogram is the study of a smear from the nasal mucosa under a microscope. It helps to assess the functioning of local immunity, detect infectious diseases and other causes of inflammation of the membranes. Exceeding the norm of eosinophils always indicates an allergic origin of rhinitis. However, even if the cell level is within normal limits, an allergy cannot be ruled out. The analysis is needed for a comprehensive diagnosis of seasonal allergic reactions; its results are studied together with other information obtained during the examination.
Question: Have you heard that the level of corpuscles is checked in the urine, nose, and sputum? Why do they do this and how do blood cells end up in other fluids?
Answer: Eosinophils are everywhere. These bodies are released into the blood and eventually migrate to peripheral tissues. Large concentrations are concentrated on the mucous membranes. Here the cells are involved in local immunity. The level of eosinophils in a nasal swab, as well as in sputum, is indeed determined. This is necessary for diagnosing allergic diseases. The total number of leukocytes in the urine is counted (without defining groups). Exceeding the norm accompanies inflammatory lesions of the kidneys and urinary tract.
Question: What is better to take if the levels are only slightly elevated - an anthelmintic or an antiallergic?
Answer: Drugs from these groups cannot be taken independently in order to correct the blood picture. You need to focus on the symptoms. If the cause of the deviation is obvious, it is permissible to begin treatment, but you need to understand its nature - determine the type of parasites, detect the allergen and the method of its penetration into the body. One-time use of drugs instead of full-fledged therapy cannot lead to recovery or a decrease in the levels of protective cells in the blood.
Combined elevations of eosinophils
People with allergies will experience an increase in eosinophils and lymphocytes when infected with viral infections. This condition is typical for allergy sufferers with helminthiasis and dermatoses. A similar picture is observed in patients receiving treatment with antibacterial drugs and sulfonamides. A jump in eosinophils and lymphocytes in children occurs with infectious mononucleosis and scarlet fever. Therefore, it is necessary to carry out additional laboratory diagnostics: examine the feces for worms, determine the level of immunoglobulin E and the presence of antibodies to the Epstein-Barr virus in the blood.
If, against the background of eosinophilia, there is an increase in the level of monocytes, then an infectious process is occurring in the person’s body. Most often it is mononucleosis. The same blood picture is possible with sarcoidosis, mycotic lesions, viral infections, tuberculosis, gonorrhea and rickettsiosis.
Author of the article:
Alekseeva Maria Yurievna |
Therapist Education: From 2010 to 2021 practicing physician at the therapeutic hospital of the central medical unit No. 21, the city of Elektrostal. Since 2021 he has been working at diagnostic center No. 3. Our authors
conclusions
Eosinophils are protective blood cells from the group of leukocytes that resist allergens, parasites, and atypical cells. The proportion among all leukocytes is considered to be up to 5% and the absolute value is up to 0.3*10⁹/l. An increase may indicate:
- allergies;
- autopathology;
- malignant diseases;
- infection with worms or other parasites.
A decrease in the level of eosinophils is detected much less frequently, but may be associated with the development of oncology, chronic infectious diseases, and occurs while taking certain medications. Some conditions can threaten human life and therefore require timely diagnosis and treatment. Read more about this in the article: “Eosinophils are low - what do these blood counts indicate and what to do.”
Eosinophilia is a laboratory term, a symptom of disorders in the body. To eliminate deviations, it is necessary to determine the nature of the pathology and begin pathogenetic treatment.
How to take the test correctly?
In order for the analysis result to be accurate and truly reflect what is happening in our body, we need to be properly prepared. Moreover, there is nothing complicated in preparing for this analysis.
First of all, both parents and the child need to prepare mentally. It is best for the child not to cry, not to panic, and to behave calmly. To do this, parents should explain to the baby what will happen in the hospital, that there is nothing wrong with it. Maybe you can even promise your child something in return if he behaves well.
It is also important to prevent your child from running around the hospital corridors while waiting for their turn in the blood collection room. Physical activity may affect study results.
Also, one of the most important rules for preparing for a blood test is that it must be taken on an empty stomach. If the child is already big (over 4 years old), then you can be patient and donate blood after an overnight fast. It is allowed to give the child water to drink.
It is recommended not to feed infants for 1 - 1.5 days before donating blood.
Blood is most often taken from the finger; in very small children, from the heel.
When preparing to donate blood, it is important to take prescribed medications. A number of medications can affect test results. Therefore, it is advisable to talk to your doctor about this. Don't do anything on your own!
Some medications can affect the level of the determined indicator. For example, Prednisolone can lead to a decrease in the level of eosinophils and monocytes in the blood.
If parents properly prepare for donating blood, they will not have to take the test again, plunging their child into a stressful situation.