The mobile Internet audience is growing rapidly
66 million Russian users use it along with desktop, and 20 million already access the Internet only from mobile devices - this is 15% more than a year ago.
Pages on smartphones may load slowly
There are several reasons: an unstable network connection, low Internet speed, or the site is not adapted for mobile devices. If you have to wait too long, users will move to other sites.
We offer users Turbo technology
It significantly speeds up the loading of text, images and videos on smartphones and helps save time and megabytes of mobile Internet.
General information
The most common skin diseases include pyoderma (pustular skin lesions), which arise as a result of infectious skin lesions by pyogenic microbes. One of the types of pyoderma is streptococcal pyoderma ( streptoderma ), that is, it is an infectious skin disease caused by streptococci.
Streptoderma is characterized by predominant damage to smooth skin and folds with a pronounced tendency of the lesions to grow peripherally. At the same time, skin appendages (sweat glands/pilosebaceous apparatus) are not affected. Streptoderma code according to ICD-10: L08.0. Streptoderma in adults accounts for about 40% of all pustular skin lesions. In this case, streptoderma can occur both as a separate nosological form and as a mixed streptostaphylococcal skin lesion. In adults, relatively young women with thin skin are more often affected. Streptoderma often (in 30% of cases) is the cause of temporary disability. Streptococcal pyoderma is considered an occupational disease in a number of industries (metallurgical, mining, construction, etc.). Also, streptoderma on visible parts of the body (face, neck, hands, head), especially in women, causes psychological discomfort.
Streptoderma occurs more often in children than in adults and its share in the overall structure of pustular skin diseases reaches 60%. Streptoderma is most common in children 2-7 years old. In addition to the general reasons, there are additional reasons for the occurrence of streptoderma in children, due to the natural vulnerability of the child’s delicate skin, the low effectiveness of the skin as a protective barrier, the lack of stable personal hygiene skills and the presence of close contact between children. Frequent minor injuries to the skin in the form of minor wounds, scratches, and maceration contribute to a high risk of developing the disease. Therefore, outbreaks of streptococcal infection are very typical for children's groups (kindergartens, primary schools).
The term “streptoderma” is a collective concept that unites several skin diseases - streptococcal impetigo , bullous impetigo , crevice impetigo (seizures), paronychia (superficial panaritium ), papulo-erosive streptoderma , intertriginous streptoderma , erysipelas , streptococcal toxic shock syndrome , acute streptoderma , chronic diffuse streptoderma , ecthyma .
Foci of streptoderma are found on various parts of the body - streptoderma on the head in the hair (skin on the head), on the skin of the hands and legs (including on the hands/feet), streptoderma on the face, in the groin area, in the nose, on the torso , in the intergluteal folds, on the behind-the-ear folds, in the armpits and other places. At the same time, the localization of foci depends on the form of the pathology. For example, streptococcal infection is localized in the corners of the lips; streptococcal diaper rash - in the groin area, armpits, behind-the-ear/intergluteal folds; streptococcal impetigo - most often on the torso, face, upper/lower extremities; bullous impetigo - on the legs, hands, feet; streptococcal ecthyma - on the buttocks, upper/lower limbs, etc.
How is it different from other diseases?
Even not every doctor will be able to make the correct diagnosis and differentiate streptoderma from other diseases from the first examination.
The problem is that this infection is very “many-faced”; it has many varieties that are localized on different parts of the body.
Parents can all the more easily confuse the manifestations of streptococcal pyoderma with other infectious and dermatological diseases - herpes, chickenpox, eczema, urticaria, atopic dermatitis, allergies.
The general symptoms are similar for many diseases, but each of them has special, characteristic signs, which are used to make a diagnosis.
In skin diseases, the main symptom is rashes, which differ in their location and appearance:
- For example, a herpetic rash is distinguished by pain, while a chickenpox rash is distinguished by the presence of rashes of different stages at the same time - from pimples to crusty dried blisters.
- With streptoderma, there are no catarrhal symptoms - no runny nose or cough. The rash is also different from skin lesions associated with other diseases. With streptococcal infection, the contents of the blisters are clear, not cloudy.
- Seizures with streptoderma differ from similar formations with herpes in that the conflicts quickly open, and then cracks form in the corners of the mouth. Herpes blisters last longer, but then no cracks form.
Such nuances distinguish streptoderma from other, at first glance, similar diseases. But only an experienced doctor can correctly differentiate the infection.
If you are interested in how to quickly treat a cold on your lip, read our post and find out.
Instructions for using Belogent ointment, its cost and consumer reviews of the drug are presented in this material. Find out more!
Pathogenesis
The pathogenesis of the disease is determined directly by the properties of streptococci themselves and substances that are produced by microorganisms and released into the external environment (toxins, enzymes hyaluronidase , streptokinase ). Streptococci that cause pyoderma belong predominantly to serological groups A and D. Streptococci of serogroup A synthesize various types of toxins: O- and S-streptolysin, necrotic/hemolytic toxins, leukocidin and several variants of enterotoxins . After the pathogen penetrates through microdamages on the skin/mucous membranes, they begin to actively multiply and also release factors of aggression (toxins) and protection from the body’s immune system into the environment. The depth of skin damage is determined by the state of cellular/humoral immunity. The chronicity of the acute process is based on a decrease in the production of immunoglobulins A and G, the phagocytic activity of neutrophils, and a decrease in subpopulations of T-lymphocytes.
Classification
The classification is based on several factors. Based on the nature of their occurrence, they are distinguished:
- Primary streptoderma (the causative agent of the infection enters the body through damaged areas of the skin/mucous membrane with the development of an acute inflammatory process).
- dermatoses already present in the body (chronic eczema , atopic dermatitis , scabies , etc.).
There are 3 forms of the disease:
- Bullous impetigo (accompanied by the formation of painless, large, fluid-filled blisters).
- Nonbullous impetigo (accompanied by the formation of pustules, after rupture of which a yellowish-brown crust forms).
- Dry streptoderma (erymatosquamous). The dry form occurs without weeping elements and is expressed in the appearance of uneven rounded spots of a reddish-pink color with flaking whitish particles of the epidermis.
According to clinical variants, several types of streptoderma are distinguished: streptococcal impetigo , bullous impetigo , crevice impetigo (seizures), paronychia (superficial panaritium), papulo-erosive streptoderma , intertriginous streptoderma , erysipelas , streptococcal toxic shock syndrome , acute , diffuse streptoderma chronic streptoderma , ecthyma .
Causes of streptoderma
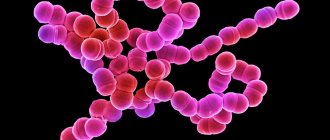
The leading etiological factor of streptoderma is serological group A streptococcus (beta-hemolytic), which affects damaged skin. Normally, these microorganisms can be present in small concentrations on human skin without causing disease. Streptococci are gram-positive microorganisms measuring 0.5-2.0 microns in diameter and having a spherical shape (picture on the right).
They are relatively stable in the external environment: they can withstand heating up to 60˚C for 30 minutes, tolerate drying well and remain in sputum/dried pus for a long time (months). They quickly die under the influence of disinfectants ( chloramine , phenol ). They can multiply in various food products (minced meat, milk, salads, compote). When released into the external environment, streptococci lose their capsule and their ability to cause an acute infectious process.
What causes streptoderma? A number of exogenous and endogenous factors contribute to the development of the disease:
- Skin contamination.
- Violations of the integrity of the epidermis/infection of wound surfaces.
- Shift in skin pH to the alkaline side.
- Increased sweating.
- The presence of diseases that damage the integrity of the skin: pediculosis , atopic / allergic dermatitis , scabies , as well as a tendency to scratch wounds and insect bites.
- Effect of low/high temperatures.
- Immunodeficiency conditions (primary/secondary).
- Prolonged physical fatigue/frequent stress.
- Lack of personal hygiene, especially scratching bites or abrasions with dirty hands.
- Rare/frequent water procedures (with a lack of water procedures, opportunistic microflora and dead epidermal cells are not removed from the skin, and with frequent water procedures, the protective skin barrier is broken).
The source of streptococcal infection is humans. Is streptoderma contagious or not and how is streptoderma transmitted? Yes, this is a contagious disease, transmitted by contact (directly by touching the skin of a carrier/sick and healthy person, by kissing, playing together, etc.) or by household contact when using common household items: toys, dishes, towels, books etc. In closed institutions with close contact (military units, pioneer camps, preschool/school institutions), streptoderma often occurs as an epidemic outbreak.
How many days is contagious and is the disease contagious in the early period? The incubation period of streptoderma varies between 7-10 days and already during this period the probability of infection is very high, as well as throughout the entire period of the disease. Impetigo is a particularly contagious disease , so it is necessary to isolate sick people from healthy children to prevent epidemic outbreaks.
Routes of infection
You can get infected even from a healthy person (who does not have streptoderma, but has this infection on the skin). Streptococcus is present in many people. And enough weakening of the immune system, a scratch. The disease will begin to develop.
It is difficult and difficult to treat when infected from a person with streptoderma, or objects with which he has been in contact. You can become infected from people with an infectious disease caused by streptococci.
Can be transmitted by airborne droplets, contact and household contact. The disease is most quickly transmitted in public places (baths, saunas, swimming pools). It is not transmitted from animals to humans.
Symptoms of streptoderma
Streptoderma can occur in various clinical forms. The localization of the pathological process, the depth of the lesion and its prevalence are of great importance. How does streptoderma begin in adults? The main symptoms of streptoderma in adults are presented below:
- Phlyctena is a rash on the skin in the form of flat blisters, surrounded by hyperemia (redness) and filled with serous-purulent contents, in the place of which, after opening, a crust forms, and after it falls off, peeling and subsequent pigmentation of the skin occurs.
- Skin itching is moderate and painful.
- General symptoms of body intoxication: weakness, lethargy, increased body temperature, lack of appetite.
Moreover, each clinical variant of the disease has its own characteristic symptoms. What streptoderma looks like will be presented when describing one or another clinical variant. Due to the small volume of the article, we will consider only some clinical forms of streptoderma.
Streptococcal impetigo . The predominant localization of rashes is on open areas of the skin of the face, the back surface of the forearms/hands. Characteristically, against the background of hyperemic/edematous skin, conflicts appear, vesicles 2-8 mm in size, filled initially with transparent and later with purulent turbid contents. As a rule, in place of the phlyctena, after 2-3 days, straw-yellow thin loose crusts are formed, corresponding to the size of the previous blisters. It is extremely rare that impetigo is limited to a single element without its peripheral growth. More often, the number of elements quickly increases, which grow along the periphery and merge with each other, forming a ring-shaped impetigo , in the center of which there are crusts, and along the periphery there are fresh conflicts / vesicles and erythema (Fig. below).
The evolution of the rash lasts 4-7 days, and the duration of the disease is 3-4 weeks. Complications in the form of lymphadenitis / lymphangitis . In some patients, after impetigo resolves, pityriasis-flaky spots of post-inflammatory depigmentation of a pink-bluish color remain for a long time. In cases where streptococcal lycten is located in the deeper layers of the epidermis or in areas with a pronounced stratum corneum, it often does not open on its own and does not shrink into a crust, but rather increases in volume, reaching the size of a large bubble, that is, bullous impetigo .
Superficial panaritium (Fig. below). It develops in the area of the nail folds, surrounding the nail plate in a horseshoe shape. In a chronic course, the skin of the nail fold becomes bluish-pink in color, infiltrated, a fringe of exfoliating epidermis is located along the periphery of the nail plate, and pus is periodically released from under the nail fold. onycholysis may develop .
Streptococcal impetigo (slit-like impetigo)
Streptococcal seizure (in the corner of the mouth) occurs more often in patients who have the habit of licking dry lips (with chronic eczema , atopic dermatitis , actinic cheilitis . It is an erosion surrounded by exfoliated epidermis remaining from the phlyctena. In the center of the erosion, there is a radial crack, which is partially may be covered with honey-yellow crusts. Slit-like impetigo is characterized by an extremely persistent course, especially if the disease develops against the background of atopic cheilitis. The healing process of erosions is hampered by constant traumatization/maceration of the corners of the mouth. Often, seizures and streptococcal impetigo of the face are combined with damage to the mucous membranes of the nasal cavity , mouth, eyes.The forming conflicts quickly open, and the resulting erosions on the mucous membranes are covered with a yellowish-gray coating.
Streptococcal diaper rash
The development of diaper rash is promoted by severe forms of seborrheic dermatitis , obesity , type 2 diabetes mellitus hypercortisolism . The favorite localization of diaper rash is large folds: intergluteal/inguinal-femoral folds, armpits, behind the ears, folds under the mammary glands, abdomen and neck, mainly in people with increased body weight (obesity). The disease develops as a result of friction of skin surfaces in the fold and maceration of the stratum corneum, caused by intense sweating , as well as natural secretions in the absence of adequate hygienic skin care. These factors contribute to the development of an inflammatory reaction in the folds of the skin and the addition of streptococcal flora, often in association with yeast-like fungi.
Manifestations of streptococcal diaper rash are typical: the skin surfaces in contact in the folds are swollen, hyperemic, maceration of the stratum corneum and its subsequent erosion are observed. Due to constant friction, the resulting conflicts quickly open and in place of the opened conflicts on the contacting surfaces, an extensive bright red erosive surface with scalloped edges is formed, and along the periphery - exfoliated epidermis. The eroded zones become wet, and cracks appear directly in the depths of the fold. Patients complain of itching, a burning sensation, and if cracks occur, severe pain. With regression of the pathological process, persistent pigmentation may remain for a long time (Fig. below).
Acute diffuse streptoderma
The predominant localization is the skin of the lower extremities, the skin around burns, fistulas, and infected wounds. The inflammation is characterized by a serous nature, the appearance of multiple conflicts, prone to peripheral growth and fusion with the formation of continuous superficial erosions, bordered by a rim of exfoliated stratum corneum of the epidermis with scalloped outlines.
The infectious process develops against the background of swelling of the lower extremities and severe hyperemia , and is characterized by abundant diffuse oozing and the presence of serous honey-yellow crusts. Often, ring-shaped conflicts appear along the outer edge of the exfoliated stratum corneum, caused by the peripheral growth of the lesion. Acute diffuse streptoderma is often complicated by lymphangitis and lymphadenitis . In the absence of adequate treatment and the presence of predisposing factors ( varicose veins , trauma , maceration ), a transition to a chronic form is observed.
Chronic diffuse streptoderma
Clinically, the form of the disease is an inflammatory focus of extensive skin lesions, (usually the legs) which is characterized by hyperemia , often with pronounced stagnant infiltration of the skin of a bluish-brownish color with large scalloped, clearly defined boundaries. The surface of the skin in the lesion is covered with lamellar serous-hemorrhagic or purulent crusts, under which there are erosions and areas of weeping. The course of the disease is long-term with periodic exacerbations and subsidence of the inflammatory process. It is often complicated by sensitization of the body to streptococcal flora and the subsequent development of microbial eczema.
Ecthyma (ulcerative streptoderma)
The predominant localization is the skin of the lower extremities. It is characterized by the appearance of a purulent phlyctena, which over the course of several days shrinks into a crust, under which a deep ulcer is revealed. The bottom of the ulcer and the edges are soft and inflamed. Covered with necrotic purulent mucous coating. The ulcer scars within 2-4 weeks (Fig. below).
How long does streptoderma last? Normally, the disease with adequate therapy, depending on the clinical form, lasts from 3 days to 2-3 weeks.
Oral medications: names of drugs, instructions
Along with ointments and antibiotics, other medications taken orally are also prescribed. Their main purpose is to relieve itching and restore immunity.
Main concomitant medications:
- Anaferon (for adults). The tablets are taken to fight bacteria and strengthen the immune system. Prescribed in complex therapy. The first 3 days are taken in 8 tablets, the subsequent days 4. The course of treatment is up to 3 weeks. Side effects include an allergic rash. Not suitable for use by children under 18 years of age.
- Retinol. Fights skin diseases, restores the functioning of the gastrointestinal tract, strengthens the immune system. Take up to 3 capsules per day. The exact course of treatment is prescribed by the doctor. Not recommended for use if: drug intolerance, liver problems, age under 7 years. Side effects: skin rashes, headache, vomiting.
- Pyrogenal. Accelerates skin regeneration, improves the functioning of the digestive system, strengthens the immune system. The dosage and course of treatment are prescribed by the doctor. A side effect is an increase in body temperature. Do not take if you have a fever or if you are pregnant. Sold by prescription.
- Suprastin. Prescribed to relieve an allergic reaction. Take 1 tablet up to 4 times a day. The full course of treatment is prescribed by a doctor. Side effects: dizziness, abdominal pain, cramps. Not suitable for pregnant women and children under 3 years of age.
- Claritin. Used to combat allergies. Take 1 tablet 1 time per day. The full course is prescribed by the doctor. Side effects: headache, weakness, nausea. Should not be taken by children under 3 years of age or if they are intolerant to the drug.
- Tavegil. Antiallergenic agent. Take 1 tablet in the morning and evening. The course is prescribed by the doctor. Side effects: weakness, nausea, low blood pressure. Do not take: for asthma, pregnant women and children under 6 years of age.
You cannot start taking medications on your own. The full course of treatment and dosage is prescribed by the therapist.
Treatment of streptoderma in children
Most often, streptoderma in children is localized on the face and other areas not protected by clothing (arms, neck), and in the absence of adequate and timely treatment, it can spread to other areas of the skin. Unlike adults, most common forms of the disease in children are often accompanied by a violation of the general condition, including an increase in temperature in the evening, as well as polyadenitis and changes in the peripheral blood ( leukocytosis , increased ESR, neutrophilia).
The symptoms of streptoderma in children are not fundamentally different from the symptoms of adults. We can only note that dry streptoderma , which is a type of streptococcal impetigo, is much more common in children. Dry streptoderma in children (lichen simplex) often develops with frequent visits to the swimming pool, which is caused by a shift in skin pH to the right (to an alkaline environment). Lesions begin on the skin of the face (around the mouth, lower jaw, cheeks), torso, and extensor surfaces of the limbs. Initially, the disease looks like a pink-red spot, covered with many thin whitish scales, which gradually increase due to peripheral growth. Children complain of dry skin and slight itching in the affected areas. After the process is resolved, depigmented spots remain.
Another type of streptococcal impetigo is papular syphiloid impetigo , which occurs in children mainly in the first years of life. How streptoderma begins in children (photo below).
The symptoms often resemble weeping erosive syphilitic papules. The predominant localization is on the skin of the buttocks, legs, and thighs. This form often occurs with insufficient hygienic care and is characterized by the appearance of erythematous spots of varying sizes, on the surface of which papules with clear boundaries of a pinkish-red color or with a bluish tint are formed. Subsequently, conflicts appear on the surface of the papules, in the place of which, after opening, erosions form.
Drugs for the treatment of streptoderma in children at home are similar to those for adults, especially drugs for local therapy. That is, you can use almost all solutions of aniline dyes and the ointments described above. Parents are often interested in the question: how to treat streptoderma in a child’s nose and specifically what to smear the nasal mucosa with? Treatment of streptoderma on the mucous membranes, including the nose, is not fundamentally different and similar preparations can be used, including ointment/cream/gel for external use containing antibiotics, unless their use in children is prohibited or limited by the child’s age. In addition to the drugs described in the treatment of adults, we can recommend drugs for external use such as Retapamulin and Monocycline , the safety of which for use in children is approved by the FDA. Drugs for systemic therapy for children are prescribed taking into account indications/contraindications for children, as well as taking into account the age (weight) of the child.
As E. Komarovsky says about the treatment of streptoderma in children (see forum), it is important to prevent streptoderma from spreading to other areas of the skin. In his opinion, it is important not to forget about the characteristics of children's skin, especially the sensitive skin of a baby. Therefore, you should avoid using highly concentrated aniline dyes with alcohol, as they can cause burns, and use a weak solution of potassium permanganate to treat leather.
When the process is localized on the scalp, salicylic Vaseline . For wound healing, antiseptic Fukarcin ointment or ointments containing antibiotics are recommended - Tyrose gel , Tetracycline / Erythromycin ointment .
The prescription of hormonal ointments is allowed only in cases of advanced streptoderma. When prescribing systemic antibiotic therapy, Dr. Komarovsky recommends simultaneously prescribing probiotics , children's multivitamins, and drugs that strengthen the immune system. With timely treatment and adequate and appropriate treatment, the disease in children goes away in 4-7 days without significant complications. Advanced streptoderma is treated in a hospital.
Antibiotics: names, instructions
Antibiotics are the best way to fight infection. Before prescribing the drug, the dermatologist identifies the pathogen and selects the appropriate medicine. You need to know what medications you are intolerant to.
Commonly prescribed antibiotics:
- Amoxiclav. The active substance is amoxicillin and clavulinic acid. The drug has a long effect. Destroys streptococcal, staphylococcal and gonococcal infections. Take 1 tablet 2 times a day (every equal period of time). Do not use if you have liver disease or allergies. Side effects may include: diarrhea/constipation, rash, cramps. Antibiotics are used to treat streptoderma in adults.
- Augmentin. Has a wide spectrum of action. Resists various types of bacteria. The course of treatment and daily dosage are prescribed by a dermatologist. Do not take: if you are allergic to the medicine, pregnant women, people with liver problems. An adverse reaction may include various allergic rashes.
- Azithromycin. Destroys bacteria and harmful microorganisms. The course of treatment is up to 12 days. On the 1st and 2nd days, take 2 tablets 1 time per day. In subsequent ones, 1st. Prohibited to take: if you have liver disease, kidney disease, or heart problems. Adverse reaction: abdominal pain, rash, loose stools.
- Erythromycin. Antimicrobial agent (kills streptococci, meningococci, gonococci). When treating, take 0.5 g of the drug at a time, do not exceed 2 g per day. The course and exact dosage are prescribed by a dermatologist. It is not recommended for people with kidney or liver problems. Side effects: allergies, vomiting, loose stools.
- Ceftriaxone. Most often prescribed for streptoderma. Has bactericidal properties. The medicine is used intramuscularly. 0.5 mg of medication mixed with 2 ml of water is administered at a time. You can use up to 4 g of the product per day. Contraindications are: liver disease, pregnancy, lactation. Side effects: rash, problems with the digestive tract.
The listed medications are prescribed by a dermatologist, and the course of treatment is determined by a single/daily dosage. You can buy it at the pharmacy only with a prescription.
Streptoderma during pregnancy
Uncomplicated streptoderma during pregnancy does not pose a threat to the course of pregnancy itself and the development of the fetus.
With timely and adequate treatment, no serious consequences for the fetus are expected. The risk of intrauterine infection of the fetus exists only when streptococcal infection is generalized and the pathogenic factor enters the systemic bloodstream, as well as when the fetus passes through the birth canal, if at the time of birth there are elements of a rash on the woman’s body. Therefore, it is extremely important to undergo treatment before childbirth, however, treatment should be carried out under the supervision of a specialist, taking into account the gestational age, since many drugs used in the treatment of purulent skin diseases during pregnancy are prohibited as they pose a potential danger to the fetus.
Diagnostics
An experienced doctor will be able to diagnose streptoderma based on external signs and by examining the patient. It is important to distinguish the infection from other diseases with similar initial symptoms.
In cases where doubts arise and it is necessary to confirm the diagnosis with laboratory tests, the following may be prescribed:
- blood tests - general, biochemical, sometimes for HIV infection;
- urine test (general);
- bacteriological culture of liquid from affected areas to determine the causative agent of the disease and its sensitivity to various antibiotics;
- examination of stool for the presence of worm eggs.
The decision on the need for such tests is made by the attending physician. It is better to undergo additional examinations to make a correct diagnosis and begin adequate treatment.
Diet
Recommended Diet for skin diseases , which involves limiting the consumption of all simple carbohydrates (baked goods, sugar, honey, sweet fruits, jam, sweets, confectionery, etc.) by increasing the consumption of complex carbohydrates (cereals, vegetables, whole grain bread, bran) by background of physiological norms of protein and fat consumption with an emphasis on vegetable fats rich in vitamins A and E , which increase the body’s overall resistance and promote the healing of skin damage.
Prevention
Prevention of streptoderma includes:
- Maintain personal hygiene of skin surfaces.
- Timely/adequate antiseptic treatment of wound surfaces, microtraumas, scratches, insect bites, cracks in the skin.
- Identification and treatment of diseases against which streptococcal skin lesions may develop (diseases of the ENT organs, digestive tract, diabetes mellitus ).
- A balanced diet enriched with vitamins.
- Timely treatment of various pustular diseases.
What to do if streptoderma does not go away for a long time or occurs again?
With timely and correct treatment, streptoderma is usually well cured, and recovery occurs within a week. But there are situations when streptoderma drags on for several weeks, or even months.
Reasons for ineffective treatment of streptoderma:
- A chronic course of streptoderma developed. In this case, long-term treatment is required by a dermatologist and family doctor (or pediatrician) using hormonal drugs and immunomodulators, as well as treatment of concomitant diseases.
- Lack of treatment or use of counterfeit drugs. In order to avoid purchasing dummy drugs, all medications must be purchased only from official certified pharmacies.
- Failure to comply with personal hygiene rules, bathing, and scratching rashes leads to the appearance of new lesions of the rash.
- The use of antibiotics (both externally and internally) that do not act on the pathogen. If streptoderma does not go away for a long time, then it is simply necessary to find out the sensitivity of bacteria to antibacterial drugs (unfortunately, we rarely carry out an antibiogram). Only properly selected antibiotics can cope with infectious diseases.
- Weakened immunity as a result of concomitant diseases or previous viral and other infectious diseases. When the body’s defenses are reduced, it is difficult to cure any infectious pathology, even when using the most “powerful” antibiotics.
- This is not streptoderma. Some skin diseases are very similar to streptoderma, which can lead to incorrect diagnosis and, accordingly, inadequate treatment. Therefore, do not self-medicate, but seek help from experienced specialists.
- Repeated development of streptoderma (relapse) usually indicates reduced immunity. In this case, you just need to see a doctor, undergo a full examination and eliminate the causes of the body’s poor resistance to infections.
Consequences and complications
Various forms of streptoderma can cause various complications. Thus, a complication of impetigo , diffuse streptoderma , ecthyma is often lymphadenitis / lymphangitis . With intertriginous streptoderma, the addition of a secondary infection (microbial eczema) is often observed. A common complication of various forms of the disease is an allergic reaction. In patients with chronic diseases or with a weakened immune system, complications may occur in the form of the transition of an acute disease to a chronic form.
List of sources
- Dermatovenerology. National leadership. (Ed. by Yu.K. Skripkin, Yu.S. Butov, O.L. Ivanov) M.: GEOTAR-Media, 2011. – 1024 p.
- Rodionov A.N. Dermatovenerology. A complete guide for doctors. – St. Petersburg: Science and Technology, 2012. – 1200 p.
- Belkova Yu. A. Pyoderma in outpatient practice. Clinical microbiology and antimicrobial chemotherapy. 2005; No. 7 (3): pp.255–270.
- Korotkiy N.G., Taganov A.L., Tikhomirov A.A. Modern external therapy of dermatoses (with elements of physiotherapy). Ed. N. G. Korotkoy. Tver: Provincial Medicine, 2001.
- Nurullin R.M., Abdrakhmanov R.M., Khaliullin R.R. New possibilities for local therapy of pustular skin diseases/ // Kazan Medical Journal - 2012 - T.93, No. 2.