Pathogens
Pathology is caused by parasitic fungi of the genus Microsporum. The pathogen received this name because as a result of its vital activity it forms multiple small spores. Most often found in the middle zone are Microsporum canis and Trichophyton tonsurans.
Microsporum canis is a zoonotic fungus. If it comes into contact with a person, it causes a mild form of the disease and responds well to treatment.
Trichophyton tonsurans is an anthroponotic fungus. Only people become infected; it is severe and becomes chronic.
In soil and pathological material, fungi persist for up to 7 years.
Contributing Factors
People with low immunity are at particular risk, those who already have a skin disease of non-contagious etiology, if there are wounds or scratches. Frequent stress, depression, and working with soil without gloves increase the risk of contracting an infection.
Microsporia or cat lichen is usually seasonal. Outbreaks occur in August - September. Children become infected through contact with kittens infected with microspores, but outwardly completely healthy.
Adults rarely become infected with this fungus. This is due to the fact that on the skin of an adult there is a conditionally pathogenic fungus that suppresses microspores. Also in adults, undecylenic acid is produced in the sebaceous glands, which suppresses fungus.
An adult can get microsporia in several cases:
- during pregnancy;
- scalp wounds;
- if you wear an infected hat for a long time;
- in hot, humid climates;
- long illness and taking antibiotics.
Trichophytosis is not seasonal; people suffer from it all year round.
How can you get infected?
Infection can occur from sick people and animals. Most often, stray cats and dogs are carriers of ringworm. Puppies and kittens are especially often affected. In them, the disease passes more easily than in people and areas of lichen may not be noticeable.
Infection occurs when skin particles, hair or fur elements infected with a fungus come into contact with the skin of a healthy person. If fungal spores fall to the ground, they can live there for up to three months. However, they remain active and can cause disease. When the fungus gets on the skin, it penetrates the cells and begins to multiply. If there are hair follicles nearby, then the fungi grow inside them and fill the entire space of the hair follicle. Then they move up the hair. Fungal spores accumulate between the hair scales and destroy it. As a result, the hair breaks off under its own weight close to the skin. The fungus creates a white sheath around the remaining hair, which is visible to the naked eye.
The source of infection can be a sick person. You can become infected by communicating with him or by sharing towels, combs, nail scissors, hats, bed linen and washcloths. The likelihood of getting sick increases sharply if the skin has abrasions, scratches, or the person has a weakened immune system.
Incubation period
The fungus enters the human body, adapts, and begins to develop without causing visible changes on the skin for up to 8 weeks.
Superficial lichen (trichophytia) appears 5-7 days after contact with the skin. Infiltrative-suppurative (microsporia) can “dormant” for several months. This is dangerous because the infected person does not yet know about his disease, but is already spreading it.
What it is?
Ringworm is a highly contagious infection of the skin, hair or nails caused by pathogenic fungi.
The infection can be caused by two types of fungi - Trichophyton and Microsporum. The correct designation of the disease is based on the name of the fungus that caused it, so doctors distinguish trichophytosis and microsporia. Both of these forms of fungal infection (trichophytosis and microsporia) are combined under the general term ringworm.
Thus, ringworm is also called trichophytosis, microsporia, dermatophytosis, dermatomycosis or dermatophytosis. Trichophyton fungi are microbes that parasitize only on human skin, while Microsporum infect both humans and animals. Ringworm is most contagious in children 4 to 13 years of age.
Trichophytosis
The first signs of trichophytosis appear 14 days after infection. At the beginning of the disease, small round spots with dry white scales are found on the head. At the border of the spots, bubbles with pus and crusts form. Hair breaks 1-2 mm from the scalp.
A clear sign of difference from microsporia is that with trichophytosis, broken hairs look like an exclamation or question mark. Some hair does not break, but simply becomes weak and dull. The general condition of the infected person does not change.
Mostly children are infected. Without treatment, the disease can become chronic and last for several years. Most patients heal on their own when they reach adulthood.
The chronic form of trichophytosis can occur in women at a young age. At the same time, the signs are subtle and often the patient is not aware of her illness. Such people are carriers of the disease and infect children for many years.
All signs of ringworm are clearly visible in the photo.
Photo of a person
When the fungus infects smooth skin, a pink, swollen and flaky spot with clear boundaries appears in this place. It is covered with small pimples, in the middle of which a yellow transparent liquid is visible, and crusts that appear after these vesicles burst. Gradually, the center of the spot becomes less swollen and lowers. The skin becomes pink and covered with small scales.
Ringworm is surrounded by a bright red ridge that rises above the skin. It consists of small vesicles. The skin underneath is red and swollen. The spot has the shape of an uneven circle. Often a new ring of lichen appears in its center. This phenomenon is called “ring within a ring” and is a characteristic sign of this disease. The skin around the lichen is not changed, but often smaller foci of the disease may appear around it.
Diagnostics
The final diagnosis is made by a dermatologist. The doctor examines the affected areas under a fluorescent lamp. If the pathogen is Microsporum, then the hair glows bright green, and if Trichophyton, then white-blue.
A scraping is taken from the infected area of skin, culture and microscopy are done. After 5 days, a colony grows in a Petri dish by which the pathogen is identified.
Lichen is differentiated from syphilis and alopecia of non-contagious etiology.
Hygiene measures when in contact with a sick person
If you or your child have touched a sick animal or interacted with a sick person, then you need to take immediate action.
- The sooner you wash away particles containing fungus from your skin, the less likely you are to become infected.
- Wash your hands several times with antifungal soap. The simplest remedy, which is available in almost every store, is cinnamon laundry soap, or better yet, soap with birch tar.
- Wash your entire body with this soap. Suddenly, particles of the patient’s skin got under his clothes. Do not use a hard washcloth. It leaves micro-scratches on the skin, into which fungus easily penetrates.
- To wash your hair, you must use an antifungal shampoo. For example, Nizoral. You can also use it as a shower gel.
- A modern remedy with a powerful antifungal effect is Citeal. Dilute it in a small container five times. You will end up with a foaming liquid that can be used to wash your hands and entire body.
- Lavender oil, tea tree oil and turpentine have an antifungal effect. They can be used to treat small areas of skin.
Also, five days after contact, it is advisable to consult a dermatologist. He examines the body with a Wood's lamp. If you do become infected, the disease can be detected in the early stages. This will help you quickly treat her at home and avoid going to the hospital.
Treatment
We have come to the main question “how to treat ringworm in humans?”
Treatment for microsporia should be started immediately, before the disease develops into a more serious form. In this case, it will become more difficult to get rid of the disease.
Traditional and medical methods are used to treat ringworm. But you shouldn’t choose any of them on your own.
Self-medication can worsen the disease. Only a specialist – a dermatologist – should develop a treatment regimen!
Prevention
In addition to general hygiene measures, there are specific rules of behavior when a patient infected with ringworm appears in the house:
- daily external examination of all family members;
- constant disinfection of common areas;
- daily shower;
- wash your hands with tar soap after any visit to public places;
- regular examination of pets;
- contacting a specialist should occur no later than 24 hours after detection of suspicious symptoms.
Ointments against lichen
Many types of ointments have been developed for the treatment of microsporia and human trichophytosis. They differ in composition, method of action on the parasite and healing rate.
The ointment is thicker than other drugs. It lasts longer on the treated area, penetrates into the deeper layers of the skin, and therefore fights mycosis better.
An alcohol solution of iodine is used in combination with ointment. It has a detrimental effect on fungi and bacteria, disinfects the affected area of the skin:
- Iodine is used in the morning, ointment at night.
- 20% sulfur ointment. The sulfur contained in the preparation dries out the ulcers. Kills the causative agent of lichen and accumulated bacteria.
- Salicylic. Reduces inflammation, kills parasitic mycoses. The surface treated with ointment must be covered with a napkin. It is strictly forbidden to treat wounds on the face.
- Sulfur-tar. Kills the pathogen and disinfects the surface. The product is used to treat the affected area and adjacent tissues. If the focus of inflammation is strong, then apply a bandage.
- Lamisil. Inhibits the reproduction of the parasite and kills it.
- Mikospor. Destroys microsporid cells. The drug is applied to the wound in a thin layer.
Gels
Gel medications contain a high concentration of the drug. They are quickly absorbed without leaving marks on the skin and clothes:
- Exifin 1%. Apply 2 times a day for 3-4 weeks.
- Mycogel-KMP. It has a destructive effect on the integrity of the cell wall of the dermatophyte and accompanying microorganisms. Used in the same way as Exifin.
Before applying medications, the skin is cleaned of scales, crusts and other dirt.
Solutions for the treatment of trichophytosis and microsporia
The solutions are used mainly to treat the affected skin on the head. Smooth skin is wiped with medicinal solutions before applying the ointment.
- Yodicirin. The drug contains iodine and glycerin. Accelerates healing, promotes separation of scales. The drug is applied to a napkin and applied to the affected area for 20-30 minutes.
- Vokadin. Contains iodine. Fights fungi and bacteria. Duration of therapy is 2.5 months.
- Nitrofungin. Treat wounds 2-3 times a day until recovery.
Causes
Ringworm is an infectious disease caused by anthropophilic trichophytons that parasitize human skin, in the stratum corneum and inside the hair, and zooanthropophilic perichophytons that live on the skin of animals (cats, dogs, horses, cattle, mice and some wild animals ).
Trichophytosis
This is a highly contagious fungal infection that affects the scalp and smooth skin. Its causative agents are imperfect pathogenic molds of the genus Trichophyton, which reproduce asexually. Their spores are very stable in the external environment. In hair and fallen crusts, they can maintain their virulence for one and a half years. Within 30 minutes, the spores are inactivated under the influence of ultraviolet radiation, after 2-3 minutes they die in boiling water, and in 15-20 minutes they are disinfected with disinfectant solutions.
Microsporia
This is dermatomycosis, affecting the skin and hairy areas. Its causative agent is keratophilic mold parasites belonging to the genus Microsporum, which live on keratinized substrates. Once on the skin, the pathogen penetrates into the deeper epidermal layers, after which it begins to actively multiply there. In the case when fungal spores are located near the mouth of the hair follicle, they grow and lead to damage to the hair, forming a sheath around it and tightly filling the entire follicular apparatus.
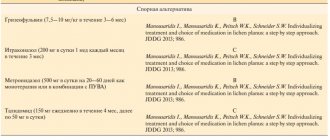
Pills
Prescribed for severe inflammation of the skin. Taking pills speeds up recovery.
- Orungal. Stops the development of dermatophyte and kills it. The course of taking the drug is 15 days, 100 mg per day.
- Griseofulvin. Stops the development of the parasite. Directions for use: 8 times a day with a spoonful of sunflower oil. Use until laboratory results are negative.
- Lamisil. Destroys dermatophyte. Use for 2.5 months, 1 tablet 2 times a day.
All of these drugs are effective, but you should not choose your own medicine. The specialist decides how best to treat ringworm for a particular patient.
Pathology photographs
Ringworm in the photo does not look the most attractive. This means we need to worry about preventing such a disease. You must wash your hands thoroughly after contact with animals and treat them with antiseptic solutions.
Folk remedies
Propolis tincture
Preparation: propolis and ethyl alcohol in a ratio of 1:4. Mix everything in a glass jar. Leave for 1 week.
Application: 4 times a day, treat the affected area with a napkin moistened with tincture. The course of application is 10 days.
Chicken egg
Preparation: the contents are removed from the egg. The film is removed from the shell. Under this film there is a liquid that is used for treatment.
Application: treat wounds with the collected liquid for a week.
To quickly cure ringworm and prevent relapses and complications, you must strictly follow all the doctor’s instructions. Treatment must be comprehensive - using only one drug will not give the desired effect in treatment.
Questions for a dermatologist
During a ringworm illness, a person is contagious, so contact can infect others.
How long does it take to treat ringworm?
No one can say for sure how long it takes to treat ringworm. It all depends on the form and stage of the disease, on impeccable adherence to the treatment regimen, which usually lasts up to 6 weeks.
When the hairline is restored, the fungi begin to feed on keratin again and characteristic spots appear. Therefore, after recovery, the patient is under observation by a dermatologist for 3 months. During this period, a person undergoes tests 3 times to detect a relapse of the disease.
Will hair grow at the site of the plaque?
After treatment, hair grows back. But on the affected area of the scalp with advanced disease, hair will no longer grow. Therefore, it is important not to let the disease progress and to start therapy on time.