The mitral valve is one of the four heart valves. It opens and closes to control blood flow between the left atrium and the left ventricle. The valve consists of two valves - front and rear.
With mitral valve prolapse, one or both valve leaflets are too large or the chordae (ligaments attached to the underside of the leaflets and connected to the ventricular wall) are too long. Due to such a violation, the valve bends back or is “sucked” into the left atrium, taking on the appearance of a parachute.
Additionally, during each heartbeat, the valve does not close tightly enough, which leads to the return of a portion of blood from the ventricle to the atrium.
What it is
Mitral valve prolapse (hereinafter referred to as MVP) is the most common valvular pathology of the heart.
The disease affects approximately 2.5% of the world's population. It is often found in children and adolescents. The predominant number of patients are women and girls. MVP is distinguished separately from valvular heart defects for two reasons. Firstly, the anomaly has a different nature of occurrence. Secondly, unlike heart defects, this pathology is benign, but can also have unpleasant consequences. Often a person does not know about its presence: MVP becomes an “accidental finding” during a medical examination or examination for another disease.
To understand the essence of this disease, it is important to understand the process of valve operation. The human heart has 4 cavities, or chambers. Normally, blood circulates in only one direction: from the atria to the ventricles, then to the large vessels (aorta and pulmonary artery). This is possible thanks to the synchronous operation of the valves, which open and close at the right time. Closed valves prevent regurgitation - the direction of blood flow in the opposite direction.
With MVP, its main function is disrupted. During the systole phase, when the left ventricle contracts, the valve leaflets cannot withstand the blood pressure and begin to protrude into the cavity of the left atrium. The main problem is that some of the blood returns to the left atrium. This is called regurgitation. All the ensuing adverse effects of MVP are associated with this process. Severe regurgitation can lead to disability.
Diagnostic methods
To accurately diagnose and assess the patient's condition, a detailed examination will be required. The following situations may trigger it:
- Accidental detection of prolapse during ultrasound examination of the heart during a preventive examination.
- Suspicion of the development of heart pathology upon examination by a therapist. The doctor, performing auscultation using a phonendoscope, will be able to hear the characteristic regurgitation noise. It indicates the release of blood back into the atrium during contraction.
- A pronounced clinical picture may be a reason to undergo a detailed examination.
The cardiologist will conduct a survey to find out the disturbing symptoms and examine the patient. A noise heard during auscultation is not always a sign of the development of a pathological process. If a teenager comes to the doctor, then other nuances have to be taken into account, for example, the extremely rapid movement of blood. Because of this specificity, a kind of turbulence arises, which is manifested by characteristic sounds. In a healthy child, such noise is equated to the individual characteristics of the body and does not in any way affect the functioning of the cardiovascular system. For the purpose of prevention, the specialist will suggest undergoing additional diagnostic methods to exclude the development of pathological processes:
- Electrocardiography (ECG) is prescribed to detect arrhythmia and ischemia of the left ventricular wall. It will not be possible to accurately detect the presence of MVP, but other pathologies can be excluded.
- Echocardiography is used to make an accurate diagnosis. The doctor will analyze the structure of the heart and its functioning, focusing on the information displayed on the screen. If at rest there are no deviations or they are minimal, then diagnostics will be required after physical activity. It is enough to squat or go up and down the stairs several times. The force with which the blood presses on the valves due to the resulting load will increase. The sagging becomes more obvious even if it is at 1 degree.
Causes of the defect
Based on its origin, mitral valve prolapse is of two types:
- primary;
- secondary.
Primary MVP is caused by genetic defects. And although the gene mutations responsible for the development of the pathology have not yet been precisely determined, there is evidence of the hereditary nature of the disease in the form of frequent cases of prolapse in close relatives.
Therefore, if one of your parents or siblings was diagnosed with MVP, there is a high probability that you have it too.
Primary prolapse is divided into types:
- MVP itself as an independent disease;
- MVP as a manifestation of connective tissue development disorders.
The latter refers to hereditary diseases caused by a defect in the formation of collagen protein. Such diseases include Marfan and Ehlers-Danlos syndromes, as well as common undifferentiated connective tissue dysplasias. In addition to MVP, these pathologies are characterized by different clinical manifestations:
- increased vulnerability and hyperextensibility of the skin;
- frequent subluxations and dislocations;
- hypermobility of joints - a person is able to bend his elbows and knees in the opposite direction, touch his thumb to his forearm, close his palms, placing his hands behind his back;
- chest deformities – keeled, funnel-shaped;
- curvature of the spine - scoliosis, kyphosis;
- flat feet;
- early myopia;
- aneurysms of the interatrial septum and aorta;
- early development of varicose veins of the lower extremities, hemorrhoids;
- diaphragmatic and vertebral hernias;
- frequent nosebleeds;
- prolapse of internal organs - stomach (gastroptosis), intestines (colonoptosis), kidneys (nephroptosis).
Secondary prolapse, as the name suggests, develops against the background of other diseases. MVP occurs due to expansion of the cavities of the heart, stretching of the fibrous ring of the valve, due to wrinkling, inflammation of the valve leaflets or the deposition of calcium salts in them.
Causes of secondary prolapse:
- cardiac ischemia;
- cardiomyopathy;
- myocarditis;
- congenital and acquired heart defects;
- chronic rheumatic heart disease.
Separately, I would like to highlight the “harmless or physiological” MVP, which develops due to the immaturity of the valve itself (fibrous ring, leaflets) and the subvalvular apparatus (tendon filaments or chords and papillary muscles). During ventricular systole, the papillary muscles contract and tighten the chordae, which keep the valve leaflets from sagging.
It often happens that in a growing child’s body, some heart structures develop earlier, while others develop later.
Consequences of this:
- the formation of too long valves or chords;
- large diameter of the fibrous ring;
- insufficient contraction of the papillary muscles.
This can lead to prolapse of the mitral valve leaflets. However, physiological prolapse is called “harmless” for good reason. By the age of 18–20, all structures of the heart have fully matured, and the valve functions as in a healthy person.
Classification of PMC
Depending on how strong the regurgitation is (the degree of filling of the left ventricle with residual blood) they are distinguished:
1st degree
The minimum deflection of both sashes is 3 mm, the maximum is 6 mm. Reverse blood flow is insignificant. It does not lead to pathological changes in blood circulation. And it does not cause any associated unpleasant symptoms. It is believed that the patient’s condition with grade 1 MVP is within normal limits. This pathology is detected by chance. No drug treatment is required. But the patient is recommended to periodically visit a cardiologist. Sports and physical education are not contraindicated. Running, race walking, swimming, skiing and skating are good for strengthening the heart muscle. Figure skating and aerobics are useful. Admission to practice these sports at a professional level is issued by the attending cardiologist. But there are also limitations. The following are strictly prohibited:
- Weightlifting sports involving dynamic or static lifting of weights;
- Strength training sessions.
2nd degree
The maximum deflection of the sashes is 9 mm. It is accompanied by clinical manifestations. Symptomatic drug treatment is required. Sports and physical exercise are allowed, but only after consultation with a cardiologist who will select the optimal load.
3rd degree
The 3rd degree of prolapse is diagnosed when the valves bend by more than 9 mm. In this case, serious changes in the structure of the heart appear. The cavity of the left atrium expands, the ventricular walls thicken, and abnormal changes in the functioning of the circulatory system are observed. They lead to the following complications:
- MK insufficiency;
- Development of heart rhythm disturbances.
In grade 3, surgical intervention is required: suturing the valve leaflets or MV replacement. Special gymnastic exercises are recommended, which are selected by a physical therapy doctor.
Based on the time of occurrence, prolapse is divided into early and late. In a number of European countries, including Russia, the classification of the disease includes:
- Primary
(idiopathic or isolated) MV prolapse of hereditary, congenital and acquired origin, which may be accompanied by myxomatous degeneration of varying severity; - Secondary
, represented by undifferentiated connective tissue dysplasia and resulting from hereditary pathology (Ehlers-Danlos disease, Marfan disease) or other heart diseases (complications of rheumatism, pericarditis, hypertrophic cardiomyopathy, atrial septal defect).
Frequent symptoms
Most people with “harmless” mitral valve prolapse, especially children and adolescents, have an asymptomatic course of the disease and nothing bothers them. Sometimes patients complain only of minor chest discomfort. I would like to note that the clinical picture may not correspond to the degree of pathology.
Symptoms of mitral valve prolapse:
- pain in the left side of the chest or behind the sternum: stabbing, pressing, squeezing, moderate intensity. The duration varies from a few seconds to a day. Pain can occur either during a strong experience or performing physical exercise, or spontaneously, for no apparent reason. Often the unpleasant sensation is accompanied by a feeling of lack of air, the appearance of cold sticky sweat, anxiety and even fear of death;
- dizziness due to low blood pressure;
- rapid heartbeat, sensations of “interruptions, rolling, freezing” in the chest;
- frequent pre-fainting conditions, in which a person experiences a feeling of lightheadedness and nausea, accompanied by flashing spots before the eyes and blurred vision;
- with severe and prolonged mitral regurgitation, signs of congestive heart failure are added - difficulty breathing, rapid onset of fatigue, swelling in the legs, especially in the evening, heaviness in the right side due to an enlarged liver.
Also, in people with mitral valve prolapse, often due to hereditary connective tissue disorders, I observe symptoms of autonomic dysfunction:
- constant pressure changes;
- fainting;
- increased sweating;
- neurotic disorders - such patients are usually anxious and suspicious, suffer from various phobias, hypochondriacal and obsessive-compulsive neuroses, they often invent non-existent diseases;
- “chilliness” and cold fingers and toes;
- increased sensitivity to cold;
- vegetative crises, better known as panic attacks.
Forecast
The prognosis for a patient with mitral valve prolapse depends on the course of the pathological process, its severity and the degree of regurgitation. The main role is played by timely diagnosis and compliance with specialist recommendations.
Mild cases are often not even detected and are not life-threatening. It is enough for the patient to be regularly examined and observed by a doctor. More severe forms have a less favorable prognosis. They are characterized by rapid development of complications and irreversible changes. The degree of recovery depends on the effectiveness of treatment and timely elimination of the causative factor.
Types and degrees of mitral valve prolapse
Echocardiography (ultrasound of the heart) is the main research method for diagnosing MVP. With its help, the severity of prolapse is assessed: the degree of prolapse of the valves and regurgitation. Prolapse refers to the extent to which the valve leaflets bend into the cavity of the left atrium.
Table. Classification of mitral valve prolapse
| PMC degree | Prolapse distance |
| 1st degree | From 3 to 6 mm |
| 2nd degree | 6 to 9 mm |
| 3rd degree | More than 9 mm |
There are pathologies:
- with regurgitation;
- without regurgitation.
The disorder is also assessed by ultrasound of the heart, but in Doppler mode.
There are 4 degrees:
- 1st degree - reverse blood flow penetrates into the cavity of the left atrium at a distance of up to 20 mm;
- 2nd degree – penetration to the middle of the atrium;
- 3rd degree - blood flow passes more than half of the atrium;
- Grade 4 – regurgitation to the opposite wall of the atrium.
Approximately 30% of people with MVP, which developed against the background of hereditary connective tissue diseases, additionally have tricuspid valve prolapse, and 4-5% have aortic valve prolapse.
Drug therapy for concomitant myocardial disorders
In addition to general tonic and sedatives, according to indications, the doctor prescribes drugs to improve metabolism in myocardial cells:
- Carnitine,
- Vitalayn,
- Tison,
- Panangin or Asparkam,
- Coenzyme Q,
- Riboxin.
It should be noted that these drugs do not have a sufficient confirmatory base based on the results of use. However, patients consider them effective. It is recommended to use in continuous courses for 2–3 months.
For arrhythmias, the doctor prescribes weak beta blockers in small dosages.
Treatment procedures are carried out under the control of ECG studies. The above therapy is aimed at compensating for autonomic and cardioneurotic disorders, but does not concern the mitral valve itself.
Diagnosis criteria
To make an accurate diagnosis, I use specially developed criteria:
- The main ones.
- Additional.
- Non-specific.
The first include:
- late systolic click/click, late systolic murmur at the apex of the heart on auscultation. Sometimes, in order to better listen to the noise, I resort to some tricks: I ask the patient to do 10 squats or lie on his left side;
- displacement of the leaflets at the time of ventricular systole, prolapse (bending) of the leaflets more than 3 mm.
Additional criteria:
- neurotic disorders;
- the presence of MVP in close relatives (father, mother, grandparents, siblings);
- The patient’s appearance is tall, thin, long arms and legs, malocclusion, deformities of the chest or spine.
Non-specific criteria include:
- patient complaints - pain in the heart, difficulty breathing, rapid heartbeat, panic attacks;
- changes on the ECG film - negative T wave in leads II, III, aVF, frequent extrasystoles and slowing of intraventricular conduction.
The presence of 2 main criteria or one main and 2 additional criteria allows one to reliably make a diagnosis of mitral valve prolapse. In addition, these criteria help to carry out differential diagnosis, that is, to distinguish MVP from acquired heart defects.
Clinical picture
With secondary MVP, all symptoms are associated with the underlying disease. For example:
- rheumatic prolapse develops gradually - the patient gradually develops shortness of breath during light exertion, malaise, and a feeling of irregular heartbeat;
- in case of a heart attack, the clinical manifestations are different – dagger-like pain in the heart area, dizziness up to loss of consciousness;
- a penetrating wound or trauma to the chest with rupture of the attaching chords is manifested by pain, tachycardia, cough - this is an emergency condition requiring emergency medical care.
In practice, doctors most often encounter primary MVP, which may not manifest itself at first; until a certain time, the patient has no complaints. The first signs of mitral valve prolapse are usually detected in adolescence and in adults. In the clinical picture, four main areas can be distinguished:
- Dysfunction of the autonomic nervous system is determined by a person’s subjective sensations. This can be cardialgia (pain) at rest, with excitement or stress, stabbing, pressing, aching of varying intensity and duration, a feeling of fear, weather dependence, increased heart rate or interruptions in heart contractions, a feeling of lack of air. In such patients, blood pressure is unstable, and thermoregulation may be impaired. Complaints from other systems are common - belching, nausea, bloating, pain around the navel, increased urination, joint pain. Panic attacks and depression are possible.
- Phenotype and indicators of physical development - the predominant asthenic body type with a deficiency of body weight, there are signs of congenital dysplasia of connective tissue structures (excessive ability of the skin to stretch, stretch marks on the back, scoliosis, flat feet, increased joint mobility, etc.).
- Changes in the heart and blood vessels are detected by auscultation (listening to systolic murmur), as well as on an ECG (various types of heart rhythm disturbances, including atrial fibrillation) and ECHO-CG (determining the degree of prolapse in the mitral valve).
- Multiple organ disorders, concomitant pathologies:
- diseases of the ENT organs;
- intervertebral hernias, osteochondrosis of young age, flat feet;
- peptic ulcer, biliary dyskinesia, pathology of the large intestine;
- varicose veins;
- chronic pyelonephritis;
- blood clotting pathology;
- neurological disorders, cerebrovascular disorders, etc.
Is treatment required?
Factors that help determine whether treatment for mitral valve prolapse is necessary:
- symptoms;
- degree of prolapse and regurgitation;
- presence or absence of complications.
If a person has a hemodynamically insignificant grade 1 MVP and does not experience any discomfort, then treatment is not required. For such people, I only recommend giving up smoking, excessive coffee consumption, and undergoing regular examinations with a cardiologist and echocardiography (once every 3 years).
Mitral valve prolapse of the 1st degree with regurgitation of the 1st degree and mitral valve prolapse of the 2nd degree, and even more so signs of rhythm disturbances and circulatory failure, are an indication for the prescription of specific drug therapy: drugs from the group of beta-blockers (Metoprolol, Bisoprolol).
These pharmacological drugs cope well with pain, normalize heart rate and blood pressure levels. They slow down the progression of regurgitation and prevent dangerous tachyarrhythmias. Also, with the help of beta-blockers, it is possible to compensate for the effects of heart failure. If they fail, then I use calcium channel blockers (Diltiazem, Verapamil).
However, it is important to remember that there are contraindications to the use of these medications:
- severe bradycardia, i.e. slow heart rate (less than 55 beats per minute);
- atrioventricular blockades of 2 and 3 degrees;
- low blood pressure (below 100 mmHg).
“Biogenic stimulants” help in the fight against hypotension:
- Eleutherococcus;
- ginseng;
- lemongrass
To treat anxiety, I first prescribe herbal sedatives - valerian, motherwort, hawthorn. For severe neurotic disorders and for the prevention of panic attacks, stronger drugs are needed (Diazepam, Phenazepam). To get a prescription for them, I refer patients for a consultation with a neurologist, psychiatrist or psychotherapist.
When chronic heart failure develops, I prescribe ACE inhibitors (Perindopril) and potassium-sparing diuretics (Spironolactone). For severe heart rhythm disturbances that cause deterioration in health, I use antiarrhythmic drugs (Amiodarone, Propafenone). To prevent blood clots in atrial fibrillation, I use anticoagulants (Warfarin).
In the later stages of prolapse with grade 4 mitral regurgitation or severe circulatory failure, surgery is required - plastic surgery or valve replacement.
Separately, it is worth considering the issue of pregnancy during MVP. Drug treatment is not fundamentally different. If severe regurgitation occurs (grade 3–4) and serious complications develop, further actions depend on the timing:
- up to 22 weeks - medical termination of pregnancy or vacuum aspiration;
- after 22 weeks - caesarean section and placing the child in a special incubator to preserve life.
Subsequently, surgical treatment of prolapse is performed. Such radical measures are due to the high danger for the mother and fetus: death is likely.
Prevention measures
In many cases, valve prolapse is congenital. It is impossible to prevent its development. All that remains is to slow down its transition to more advanced stages by eliminating irritating factors. The following tips will help with this:
- be examined and visit a cardiologist in a timely manner;
- relax more and pay attention to your favorite hobbies;
- adjust your diet;
- engage in physical therapy to strengthen the heart muscle;
- prevent and promptly treat diseases caused by infections;
- avoid mental and physical overload;
- if possible, undergo sanatorium-resort treatment annually;
- to refuse from bad habits;
- strictly follow all doctor’s recommendations;
- try to avoid stress.
Mitral valve prolapse is often a congenital anomaly. If it does not get worse, then there is nothing to worry about. It is only necessary to be observed by a cardiologist and periodically do ultrasound of the heart to assess the development of the pathological process. If there is severe regurgitation and a clinical picture, the patient will require symptomatic drug therapy. It can be supplemented with other treatment methods. If there is no positive effect, surgical intervention is performed.
Does the prognosis change for people with MVP?
Mitral valve prolapse is a benign pathology.
But the forecast directly depends on the following factors:
- degree of prolapse;
- regurgitation is present or absent;
- Are there any complications?
With minor prolapse (1st degree without regurgitation or with 1st degree regurgitation), the prognosis is favorable. This pathology does not affect life expectancy.
For prolapse with 2nd degree regurgitation, in addition to taking medications, it is important for patients to follow a restrictive regimen. For example, boxing, weightlifting, and professional running are contraindicated for patients. Young people have restrictions on their suitability for military service. At the military medical commission, depending on the presence of complications, they are assigned categories “B”, “C”, and “D”.
Possible and negative consequences
Despite its apparent harmlessness, mitral valve prolapse is dangerous due to complications that can become a real threat to the patient’s life.
Adverse effects of MVP include:
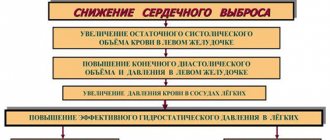
- chronic heart failure - due to regurgitation, some of the blood does not enter the aorta, so the left ventricle is forced to compensatory hypertrophy (thicken). Over time, this will lead to its dysfunction and deterioration of blood circulation throughout the body;
- heart rhythm disturbances (atrial fibrillation, prolongation of the QT interval, paroxysmal supraventricular and ventricular tachycardia). Regurgitation leads to stretching and expansion of the cavity of the left atrium, in the wall of which foci of pathological electrical activity may appear;
- ischemic stroke - a vortex flow of blood is created in the dilated cavity of the left atrium, which contributes to its thickening and the formation of blood clots;
- acute mitral regurgitation - with a pronounced degree of prolapse and regurgitation, the tendon threads that are attached to the valves are strongly stretched. As a result, their rupture and sudden overload of the parts of the heart located on the left are possible;
- infective endocarditis - during some medical procedures (tooth extraction, catheter installation, bronchoscopy), a small amount of bacteria enters the general bloodstream. With prolapse, they can settle on the valve flaps and begin to multiply. To prevent this, people with MVP are advised to take antibiotics before procedures.
These complications can quickly lead to the death of the patient.
Anatomical and physiological basis
To understand what MV prolapse is, you need to have an idea of the structure and function of the heart.
It consists of four main chambers located on 2 floors. Above are two atria, below are both ventricles. The cavities of the same name are separated from each other by muscular partitions; the atrial and ventricular chambers communicate with each other using special flaps - valves that regulate the flow of blood in a direct direction from top to bottom.
The right atrioventricular valve has 3 leaflets and is called tricuspid, the left has 2 leaflets and is called mitral. Both mitral valve leaflets, front and back, are attached to the papillary muscles of the inner walls of the left ventricle by tendon cords (chordae). There are similar valves between the left ventricle and the entrance to the aorta, as well as between the right ventricle and the common pulmonary vessel.
In a healthy heart, thanks to the coordinated work of papillary muscle fibers and tendon filaments, during systolic contraction of the atrium, the mitral valve opens and blood rushes into the ventricle, after which both valves close tightly. Next, the left ventricle contracts, and all the blood is pushed out of it into the aorta.
When there is prolapse in the mitral valve, one or both leaflets cannot close tightly, sag or bulge into the left atrium, so part of the blood returns back into it during systole. This can lead to a gradual increase in atrial volume and the development of valvular insufficiency. The prognosis for life depends on the degree of MVP and the severity of regurgitation (blood flow in the opposite direction).
Thus, this anomaly may be based on:
- pathology of one or two valves and (or) tendons attached to them (chords);
- Mitral valve DPM – dysfunction of the papillary muscles;
- violations of myocardial contractility of a local or systemic nature;
- conditions in which a decrease in the volume of the left ventricle occurs with a relative predominance of the area occupied by the chords and leaflets over the area of the atrioventricular opening (tachycardia, decrease in the amount of circulating blood, decrease in venous blood flow, etc.)
Most often, prolapse of the anterior leaflet of the mitral valve is detected, less often - both.
Expert advice: treatment of MVP for connective tissue dysplasia
People suffering from hereditary connective tissue disorders have a magnesium deficiency. This microelement promotes the formation of collagen fibers, and consequently the strengthening of connective tissue. Therefore, I recommend that such patients include foods rich in magnesium in their diet: oatmeal, bananas, nuts, buckwheat and others. It is also worth taking additional dietary supplements: Magne B6, Magnerot. To improve magnesium absorption, you can add ascorbic acid.
Etiology
It is believed that two reasons play a decisive role in the formation of PMC:
- Congenital (primary) pathologies transmitted by inheriting the abnormal structure of the fibers that form the basis of the valve leaflets. At the same time, the chords connecting them to the myocardium gradually lengthen. The sashes become soft and stretch easily, which contributes to their sagging. The course and prognosis of congenital MVP are favorable. It rarely causes complications. There were no cases of heart failure. Therefore, it is not considered a disease, but simply attributed to anatomical features.
- Acquired (secondary) cardiac prolapse. It is caused by a number of reasons, which are based on the inflammatory-degenerative process of connective tissue. Such processes include rheumatism, accompanied by damage to the mitral valve leaflets with the development of inflammation and deformation in them.
Case study: a woman with arrhythmias and prolapse
I would like to present to you a case of arrhythmia caused by mitral valve prolapse.
A 38-year-old woman approached me. For a long time, she was worried about “interruptions in the heart,” an irregular pulse, as well as episodes of rapid heartbeat, during which her well-being significantly worsened, which manifested itself in the form of nausea and dizziness. During the last such attack, the woman fainted, which is why she got scared and decided to turn to me. During the general examination, the patient’s thinness and tall stature were striking. During the examination, it was possible to note hypermobility of the elbow and wrist joints. The woman also said that as a child she often had dislocations in her arm joints. I ordered Holter ECG monitoring and echocardiography, which showed QT prolongation, episodes of torsade de pointes (TdP), and leaflet prolapse of 7 mm without signs of regurgitation. Based on the results, I made a diagnosis: grade 2 mitral valve prolapse without regurgitation with complications (prolonged QT interval, PVT, CHF class 0). I prescribed Bisoprolol (1 tablet once a day) and Magne B6 (2 tablets 3 times a day). I also provided the patient with a list of foods high in magnesium.
When taken again after 3 months, the woman noted a significant improvement: her pulse returned to normal and the attacks stopped. And the ECG showed no signs of heart rhythm disturbances.
How are prolapses treated?
In severe cases, prolapses require surgical treatment (replacement of the valve with an artificial one, or surgical measures to “strengthen” the structures of the living valve).
However, in most cases, prolapses do not require treatment, or treatment is limited to long-term intake of adequate (about 300 mg per day) magnesium preparations, which allows in the long term to normalize collagen metabolism and “strengthen” the structure of the valve. Taking magnesium supplements and mild herbal sedatives can also reduce the subjective unpleasant manifestations of vegetative-vascular dystonia, which often accompany prolapse.
In our clinic you can undergo a full range of examinations and receive advice on assessing the severity and need for treatment of prolapses.
Complications with MV prolapse
Most complications of mitral valve prolapse develop with age. An unfavorable prognosis for the development of many of them is given mainly to older people. The most serious complications that pose a threat to the patient’s life include the following:
- Various types of arrhythmias caused by dysfunction of the autonomic-vascular system, increased activity of cardiomyocytes, excessive tension of the papillary muscles, and disruption of atrioventricular impulse conduction.
- MK insufficiency caused by retrograde (in the opposite direction) blood flow.
- Infectious endocarditis. This complication is dangerous because it can cause rupture of the chords connecting the MV to the walls of the ventricle or separation of part of the valve, as well as various types of embolism (microbial, thromboembolism, embolism with a valve fragment).
- Neurological complications associated with cerebral embolism (cerebral infarction).
Prolapse in childhood
In childhood, MV prolapse occurs much more often than in adults. This is evidenced by statistical data based on the results of ongoing research. It is noted that in adolescence, MVP is diagnosed twice as often in girls. Children's complaints are of the same type. Basically, this is an acute lack of air, heaviness in the heart and chest pain.
The most common diagnosis is grade 1 anterior leaflet prolapse. It was detected in 86% of examined children. Stage 2 disease occurs in only 11.5%. MVP III and IV with degree regurgitation are very rare, occurring in no more than 1 child out of 100.
Symptoms of MVP manifest themselves differently in children. Some people practically do not feel abnormal heart function. In others it manifests itself quite strongly.
- Thus, chest pain is experienced by almost 30% of adolescent children who have been diagnosed with MVC (mitral valve prolapse). It is caused by various reasons, among which the most common are the following:
- chords that are too tight;
- emotional stress or physical stress leading to tachycardia;
- oxygen starvation.
- The same number of children experience heart palpitations.
- Often teenagers who spend a lot of time at the computer, preferring mental activity to physical activity, are prone to fatigue. They often experience shortness of breath during physical education classes or when doing physical work.
- Children diagnosed with MVP often exhibit neuropsychological symptoms. They are prone to frequent mood swings, aggressiveness, and nervous breakdowns. Under emotional stress, they may experience short-term fainting.
During the examination of the patient, the cardiologist uses various diagnostic tests, through which the most accurate picture of MVP is revealed. The diagnosis is established when noises are detected during auscultation: holosystolic, isolated late systolic or in combination with clicks, isolated clicks (clicks).
The disease is then diagnosed by echocardiography. It makes it possible to determine functional deviations of the myocardium, the structure of the MV leaflets and their prolapse. The defining signs of MVP according to EchoCG are the following:
- The MK valves are enlarged by 5 mm or more.
- The left ventricle and atrium are enlarged.
- When the ventricle contracts, the valves of the MV bend into the atrium chamber.
- The mitral annulus is dilated.
- The chords are elongated.
Additional signs include:
- Aneurysm of the septum between the atria;
- The aortic root is dilated.
The x-ray shows that:
- The pattern of the lungs is not changed;
- Bulging of the pulmonary artery arch is moderate;
- The myocardium looks like a “hanging” heart with reduced dimensions.
The ECG in most cases does not show any changes in cardiac activity associated with MVP.
Heart valve prolapse in childhood often develops due to a lack of magnesium ions . Magnesium deficiency disrupts the process of collagen production by fibroblasts. Along with a decrease in magnesium content in the blood and tissues, there is an increase in beta-endorphin and an imbalance in electrolyte balance. It has been noted that children diagnosed with MVP are underweight (inappropriate for height). Many of them have myopathy, flat feet, scoliosis, poor development of muscle tissue, and poor appetite.
It is recommended to treat MVP with a high degree of regurgitation in children and adolescents, taking into account their age group, gender and heredity. Based on the severity of the clinical manifestations of the disease, a treatment method is selected and medications are prescribed.
But the main emphasis is on changing the child’s living conditions. Their mental load needs to be adjusted. It must alternate with physical exercise. Children should visit a physical therapy room, where a qualified specialist will select the optimal set of exercises, taking into account the individual characteristics of the course of the disease. Swimming lessons are recommended.
In case of metabolic changes in the heart muscle, the child may be prescribed physiotherapeutic procedures:
- Galvanization of the reflex segment zone, with intramuscular administration of thiotriazoline at least two hours before the start of the procedure.
- Electrophoresis with calcium for vagotonic disorders.
- Electrophoresis with bromine for sympathicotonic dysfunctions.
- Darsonvalization.
The following medications are used:
- Cinnarizine - to increase blood microcirculation. The course of treatment is from 2 to 3 weeks.
- Cardiometabolites (ATP, Riboxin).
- Beta-blockers - for MVP accompanied by sinus tachycardia. The dosage is strictly individual.
- Antiarrhythmic drugs for persistent arrhythmias accompanying grade 3 MVP.
- Vitamin and mineral complexes.
Herbal medicine preparations are also used: horsetail decoction (it contains silicon), ginseng extract and other drugs with a sedative (calming) effect.
All children with BMD should be registered with a cardiologist and regularly (at least twice a year) undergo examinations aimed at timely detection of all changes in hemodynamics. Depending on the degree of MVP, the possibility of playing sports is determined. With prolapse of the 2nd degree, some children require transfer to a physical education group with a reduced load.
Recommendations for playing sports
With prolapse, there are a number of restrictions for playing sports at a professional level with participation in important competitions. You can familiarize yourself with them in a special document developed by the All-Russian Society of Cardiologists. It is called “Recommendations for the admission of athletes with disorders of the SS system to the training and competitive process.” The main contraindication for intensive training of athletes and their participation in competitions is prolapse, complicated by:
- Arrhythmia recorded by Holter monitoring (24-hour ECG);
- Relapses of ventricular and supraventricular tachycardia;
- Regurgitation above grade 2, recorded on echocardiography;
- A large decrease in blood output - up to 50% or lower (detected by echocardiography).
All people with mitral and tricuspid valve prolapse are contraindicated in the following sports:
- In which it is necessary to perform jerk-like movements - shot put, discus or javelin throwing, various types of wrestling, jumping, etc.;
- Weightlifting, associated with lifting weights (weights, etc.).