Inflammatory diseases of the large intestine are observed in both adults and children.
Spastic colitis is a nosological form that in recent years has become a pressing problem among people of different age categories, which requires the prescription of certain medications. The pathology has a varied clinical picture. It may occur with constipation, with diarrhea, or of a mixed nature. Exacerbation of the process is accompanied by unpleasant manifestations. Therefore, comprehensive medical care is needed, which includes diet, medication and folk remedies.
Spastic colitis - what is it?
Spastic colitis is a persistent disorder of the functional state of the intestine. The pathology is accompanied by the occurrence of painful spasms. The disease does not provoke organic disorders in the organ. A characteristic manifestation of this type of colitis is a dystrophic change in the tissues of the digestive tract. The inflammatory process is less pronounced than in other forms of diseases in this category.
In women, spastic colitis is diagnosed more often than in men. The risk group also includes children (from an early age).
Forecast
Official medicine does not have a clear opinion about the course of spastic colitis. In the course of numerous trials, it was determined: despite actively carried out therapy, the clinical picture of the disease in most patients remains the same, but does not intensify. The chance of eliminating symptoms within a year and a half is about 40%. Circumstances that negatively affect the prognosis and course of the disease include:
- poor patient adherence to therapy;
- variant of colitis with predominance of diarrhea;
- chronic fatigue syndrome, frequent stress;
- the patient’s anxiety about the risks of his illness;
- serious impairment of quality of life;
- long course;
- concomitant neurological or psychiatric pathology.
Colitis of the intestine Ulcerative colitis of the intestine Erosive colitis of the intestine Irritable bowel syndrome Bowel cancer Crohn's disease
Causes
The main cause of the development of spastic colitis is considered to be a violation or lack of diet. Some foods have a negative effect on the mucous membranes of the digestive organs. When they are regularly consumed as food, the functional state of the digestive tract is disrupted. In combination with a decrease in the body’s protective functions, this factor provokes spasms of smooth muscles. The consequence is spastic colitis.
Other reasons:
- consequences of hormonal imbalance in the body;
- complications of allergic processes;
- hereditary predisposition;
- infection of the digestive system by parasites;
- excessive sensitivity of the digestive organs;
- lack of diet;
- consequences of regular stressful situations;
- complications after surgery in the digestive system;
- disorders of the body's immune system;
- excessive consumption of fatty and fried foods, coffee, alcohol;
- non-compliance with sanitary and hygienic standards;
- consequences of injuries to the digestive tract;
- disturbances in the functional state of intestinal tissues;
- abuse of bad habits;
- uncontrolled use of certain types of laxatives;
- regular constipation;
- uncontrolled antibacterial therapy.
Causes and risk factors
Spastic colitis refers to functional disorders (with them there is no specific organic pathology). The intestines do not change; their work in uniform passage of feces is disrupted. Colitis can be caused by:
- imbalance of microflora;
- colonization of the intestinal tract by parasites;
- intoxication of the body;
- drug therapy;
- cholecystitis;
- gastritis;
- gout;
- enteritis;
- dysbacteriosis.
The causes of some types of colitis are still unknown.
Risk factors that contribute to the development of the disease include:
- poor nutrition;
- food poisoning;
- poisoning with toxic substances;
- hereditary factors;
- passion for starvation diets;
- physical or psychological fatigue;
- mechanical effects on the rectum;
- allergic reactions;
- undergone operations.
Forms of the disease
Spastic colitis has several forms of manifestation. Each type of disease differs in provoking factors, additional symptoms and implies a special treatment regimen.
You can identify some forms of pathology yourself, but only a specialist can make an accurate diagnosis through a comprehensive examination of the patient.
Forms of the disease:
- acute type (the main cause of development is an infectious lesion of the digestive tract, or irritation of the intestinal mucous membranes by harmful substances);
- chronic type (is a consequence of the acute form, dysbacteriosis may be a concomitant condition);
- toxic type (the provoking factor is the effect of chemicals on the intestinal mucous membranes);
- allergic type (is a complication of chronic allergic reactions);
- nutritional type (develops due to a lack of fiber in the diet, regular violations of the diet);
- medicinal type (in most cases develops against the background of uncontrolled use of laxatives and antibiotics).
Additionally, in medical practice another classification of spastic colitis is used. There are different forms with a predominance of constipation, diarrhea, or alternation of these conditions. A separate group includes unclassified colitis. This type of pathology is difficult to diagnose. Symptoms can change quickly. It is not possible to identify the predominant symptoms.
Types and forms of colitis
There are various classifications of colitis based on the nature of the disease, the causes of its occurrence, severity, localization, and so on.
According to the course, colitis is distinguished into:
- Acute is a condition that occurs with pronounced symptoms. It appears suddenly. It is often combined with inflammation of the stomach and small intestine and is called “gastroenterocolitis”. Causal factors for such inflammation: infections, taking antibiotics, acute circulatory disorders in the mesenteric vessels that feed parts of the large intestine.
- Chronic - occurs with periodic intensification and weakening of symptoms, does not manifest itself during remission. The reasons are varied: pathogenic and opportunistic microorganisms, parasites and protozoa, circulatory insufficiency in the intestinal vessels, medication, nutritional factor (diet), collagenosis (systemic scleroderma and vasculitis), intestinal endometriosis and many others.
According to the nature of pathological changes in the wall of the colon and the depth of the lesion, colitis is distinguished:
- Catarrhal is the initial stage of inflammation, when only the mucous membrane is involved in the process. There is swelling and dysfunction. More often it occurs in an acute form, accompanied by pain, changes in the nature of stool and increased frequency of bowel movements, and possibly an increase in temperature.
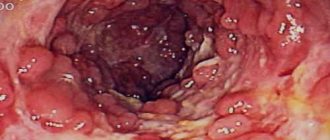
- Erosive – the integrity of the intestinal mucosa is compromised. The inflammation is deeper than in catarrhal colitis. Erosion forms on the inner lining of the intestine, which can transform into deeper defects - ulcers.
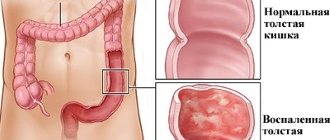
- Ulcerative is a severe degree of inflammation in which all layers of the intestine are affected. The resulting ulcers (Fig. 2) can bleed and pose a threat of peritonitis, a serious condition associated with inflammation of the entire abdominal cavity.
- Spastic. Associated with spasms of smooth muscle muscles and impaired peristalsis (motor function of the intestines). As a result, constipation and a feeling of incomplete bowel movement occur.
- Atrophic - colitis, in which, as a result of prolonged spasms and stagnation of feces or systemic diseases of the connective tissue, thinning of the mucous and muscular layers of the intestine occurs. Ulcers often appear against the background of atrophic colitis.
- Diffuse. In this case, the small and large intestines become inflamed and enterocolitis develops.
Figure 2. With ulcerative colitis, damage to the intestinal mucosa occurs - ulcers. Source: depositphotos.com
Symptoms
The main symptom of spastic colitis is the presence of paroxysmal pain in the patient in the area of the digestive organs. The condition occurs regularly throughout the day and night. Spasms weaken after defecation. The clinical picture is complemented by other abnormalities in the digestive tract and a deterioration in general well-being. The intensity of symptoms depends on the degree of progression of the inflammatory process.
Other symptoms:
- flatulence accompanied by pain;
- disruption of the bowel movement process (diarrhea, constipation);
- spasms occur on an empty stomach or immediately after eating;
- regular false urge to defecate;
- excessive gas formation and rumbling in the stomach;
- lack of appetite (the sight of food causes nausea);
- belching with air (in the presence of complications - with acid);
- irregular bowel movements (constipation may be followed by diarrhea);
- heavy coating on the tongue, bitterness in the mouth, unpleasant odor from the oral cavity;
- overly tense abdominal muscles;
- feeling of incomplete bowel movement after bowel movement.
A distinctive feature of spastic colitis is the absence of elevated body temperature and a sharp decrease in body weight. Blood and mucus in the stool are also optional symptoms. These conditions arise under the influence of concomitant pathological processes. For example, if a patient develops a peptic ulcer or gastritis simultaneously with spastic colitis.
Classification
For a differentiated approach, it is customary to classify the disease. Spastic colitis can occur in various ways. Therefore, the following categories are distinguished to make a diagnosis.
Table 1. Classification
| Criterion | Kinds |
| Process stage | Exacerbation Remission |
| Clinical course | With abdominal pain and flatulence - there is practically no stool disturbance; With constipation - dense feces predominate, cases of diarrhea are observed in no more than 25% of all bowel movements; With diarrhea - more than 50% of the stool is liquid, watery, stool retention is rarely observed; Mixed form - diarrhea alternates with constipation in an equal number of cases |
Features of the disease in children
The main causes of spastic colitis in children are bacterial and infectious lesions of the digestive system. Unlike adult patients, children may have a rise in body temperature during an exacerbation. Pain in the abdomen provokes constant crying and irritability of the child. Impurities of mucus and blood in the stool appear faster than in adults with a similar diagnosis.
Features of spastic colitis in children:
- in childhood, the main cause of the development of pathology is the impact of psychotraumatic factors;
- the second common cause of colitis in children is considered to be complications after infectious or bacterial damage to the digestive organs;
- bottle-fed children (as well as weakened babies) are at risk;
- extraintestinal manifestations of spastic colitis in children may include headaches, difficulty swallowing, excessive sweating, heartburn, nausea and signs of tachycardia.
Diet therapy
During the period of exacerbation of spastic colitis, it is necessary to adhere to a gentle diet. The list of recommended and prohibited products is given in the table.
| Featured | Prohibited |
| Dried white bread. | Grain bread. |
| Pasta dishes. | Hard cheeses. |
| Vegetable soups with weak broth. | Whole milk. |
| Turkey meat, chicken, veal. | Fried foods, smoked meats, semi-finished products. |
| Boiled and steamed vegetables. | Fibrous meat, rendered fats. |
| Potato. | Legumes. |
| Lactic acid products. | Strong tea and coffee. |
| Ripe sweet fruits without peel. | Carbonated drinks. |
| Compotes and jelly from fresh berries. | Alcohol. |
After treatment, the diet is gradually expanded. In order to prevent relapses, you should follow certain nutritional rules:
- Limit the consumption of foods that cause gas formation - fresh cabbage, legumes, confectionery, sugar.
- Increase the amount of plant fiber - eat more vegetables, fruits, and garden herbs.
- Avoid spicy, fried and fatty foods.
- Instead of milk, use fermented milk products, cottage cheese, soft cheese.
- Avoid marinades, canned food, semi-finished products, and smoked foods.
It is better to prepare dishes immediately before eating and serve warm. You need to eat 4-5 times a day in small portions. Baby food should be high in calories and appropriate for the child's age.
Diagnostics
To diagnose spastic colitis, a comprehensive examination of the patient is necessary. If you have symptoms of the disease, you should contact a gastroenterologist. After a visual examination of the patient, compiling a list of complaints and palpation of the abdomen, the doctor prescribes the procedures necessary to determine the cause of the condition.
The set of diagnostic measures includes laboratory studies of biological material and instrumental procedures.
Laboratory research methods
The subject of laboratory tests for suspected spastic colitis is stool, urine and blood. Biological material is studied for the presence of parasites, signs of the inflammatory process and deviations in the level of vital substances. Laboratory tests are a mandatory step in diagnosing the disease.
Laboratory methods:
- general blood analysis;
- blood chemistry;
- examination of stool for helminth eggs;
- examination of stool for blood and mucus;
- blood test for celiac disease;
- coprocytogram.
Instrumental research methods
The list of instrumental examination methods depends on the general clinical picture of the patient’s health status. In some cases, an ultrasound, x-ray or CT scan of the intestine is sufficient to confirm the diagnosis.
To determine the extent of pathological processes in the digestive system, additional procedures are prescribed.
Instrumental methods:
- irrigoscopy;
- anorectal manometry;
- colonoscopy;
- Ultrasound of the pelvic organs;
- colon-fibroscopy;
- sigmoidoscopy;
- X-ray of the intestines;
- Ultrasound of the abdominal organs;
- sigmoidoscopy;
- CT scan of the intestines.
Diagnostic test
The symptoms listed above are the cause of many gastrointestinal diseases. The following examination will help establish an accurate diagnosis. It is necessary to conduct a general blood test and biochemistry. A general urine test and stool test for bacterial infections and occult blood will be required. Ultrasound of the digestive organs or X-ray examination using barium.
The most reliable diagnostic method is considered to be endoscopic methods, such as colonoscopy or sigmoidoscopy, which visually make it clear what the mucous membrane is like inside. When examined with a probe, the patient is diagnosed with a loose membrane covered with erosions and cracks. At the atrophy stage, pallor and dryness of the intestinal walls are detected.
Palpation is one of the methods for identifying pathology, in which only a highly qualified gastroenterologist will discover that a person suffers from colitis.
Treatment of spastic intestinal colitis
Therapy for spastic colitis includes conservative treatment and mandatory diet. The patient should be provided with the most comfortable conditions possible. Stressful situations, emotional tension or excessive fatigue can reduce the tendency to recover.
The therapy package must be drawn up by a doctor. Self-medication can cause serious complications.
Conservative treatment
Spastic colitis does not provoke organic changes in the digestive tract. This feature of the disease precludes the use of surgical treatment methods. The need for surgery arises only in the presence of concomitant pathologies or their complications. Functional bowel disorder is treated conservatively (with medication). A doctor should draw up a list of medications.
Examples of drugs:
- antispasmodics (No-Shpa, Drotaverine);
- enzyme agents (Mezim, Festal);
- antidiarrheals (Imodium);
- enterosorbents (Enterosgel, Polysorb);
- anti-inflammatory medications (Ibuprofen, Baralgin, Analgin);
- means for restoring intestinal microflora (Bifindumbacterin).
Video - Therapeutic diet (TABLE) No. 3 (Chronic inflammatory bowel diseases)
Folk remedies
Alternative medicine recipes are highly effective in treating spastic colitis. Decoctions and infusions based on herbal components can eliminate pain, restore intestinal motility, increase immunity and improve the functional state of the digestive tract as a whole. Such drinks are prepared using the standard method. A teaspoon of dry raw materials is poured into a glass of boiling water, the preparation is infused and consumed in small portions throughout the day.
Examples of folk remedies:
- decoctions with anti-inflammatory effects (sage, coltsfoot, chamomile);
- means for stabilizing the nervous system (melissa, peony);
- infusions to reduce gas formation (dill seeds, anise, fennel, mint);
- means to improve the process of bowel movement (rowan, buckthorn bark).
How to quickly eliminate pain?
To get rid of pain in the shortest possible time, follow these steps:
Step 1. Take a comfortable position (preferably lying in bed).
Step 2. Unbutton any tight clothing.
Step 3. Refuse to drink or eat.
Step 4. Place a warm heating pad on your abdominal area.
Step 5. After about half an hour, you can take a bath with decoctions of chamomile, birch buds and/or calendula (1 tablespoon of herb per 200 ml of boiling water).
Step 6. Drink an antispasmodic.
Diet and nutrition for spastic colitis
Correction of the diet is a mandatory step in the treatment of spastic colitis. Violation of the regime, consumption of harmful foods, frequent fasting or overeating are among the provoking factors for this disease.
Diet can have a healing effect. A properly formulated diet will accelerate the tendency to recovery. Diet principles can be used to prevent relapses of colitis.
Nutrition Features:
- Baked goods and other flour products are excluded from the diet (to eliminate fermentation processes in the digestive system);
- It is forbidden to eat fatty, salty, spicy, fried, pickled foods;
- exclusion from the menu of foods that cause excessive gas formation;
- It is recommended to replace milk and dairy products with fermented milk products.
Basic principles of nutrition
The principles of nutrition for spastic colitis depend on the symptoms of the disease. If the disease develops with a predominance of constipation, then the diet should include raw vegetables and fruits, baked beets and pumpkin, whole grain bread and dried fruits. If diarrhea is present, the rules change. Vegetables and fruits should be heat treated.
Products with a laxative effect are prohibited for consumption. The basic principles of diets for constipation and diarrhea are no different.
Diet principles:
- fractional meals (small portions, 5-6 times a day);
- compliance with the drinking regime (at least two liters of water per day);
- dishes should be free of dyes, preservatives and other harmful components;
- products should be high in calories, but easily digestible by the digestive system;
- if constipation predominates, the principles of Diet No. 2 should be followed;
- if colitis is accompanied by diarrhea, then the principles of Diet No. 4 are taken as the basis for nutrition.
Enemas
How to treat spastic colitis if diet therapy and the use of medications do not produce positive results? In this case, local treatment of intestinal inflammation is prescribed using cleansing and medicinal enemas.
Cleansing enemas
Cleansing enemas are divided into two types: those that act immediately and those that have a subsequent effect.
- Enemas, which act immediately, stimulate bowel function due to the volume of fluid and its temperature. For spastic colitis, it is forbidden to use cleansing enemas with cold water, as this will lead to even greater intestinal spasm. Patients are prescribed warm enemas with water up to 36 degrees. Water should be introduced gradually and evenly, controlling the pressure level to avoid spasms and rapid eruption of incompletely administered liquid.
- Enemas with subsequent action are performed as follows: liquid is injected into the intestine and left there. The action comes after some time. This enema is given not with water, but with vegetable oil or a water-oil suspension, the volume of which can vary: from two hundred to five hundred milliliters. The oil is injected into the rectum, it spreads upward and separates dense stool from the intestinal walls, gently stimulating peristalsis.
Possible complications and consequences
With spastic colitis there is no tendency for symptoms to increase. The disease significantly reduces the quality of life. The disease is not accompanied by organic disorders of the digestive tract. However, if the symptoms of the pathology are ignored for a long time, serious complications can arise. Diarrhea provokes dehydration, constipation causes intestinal obstruction. The consequences of such conditions are disruptions in the functioning of the entire body. With intestinal obstruction, pathological processes develop that require surgical intervention.
What happens in the body during KS?
Unpleasant symptoms - the need to frequently visit the restroom, bloating and rumbling that others hear - are only one side of the coin.
Against the background of stool disorder, the patient develops dehydration (with diarrhea) and intoxication (with constipation). Poisoning with toxins that stagnate in the intestines leads to even greater irritation of the mucous membrane, bitterness in the mouth, impairs the absorption of vitamins and microelements, and disrupts the functioning of other organs. The load on the liver increases, which needs to neutralize accumulated toxins, therefore, in the absence of treatment, pathologies of the liver and gall bladder develop over time.
IMPORTANT: In severe cases, KS can cause severe weakening of the immune system, anemia and vitamin deficiencies. Ulcers form on the surface of the colon mucosa.
Prevention
Prevention of spastic colitis involves eliminating provoking factors. Intestinal motility can be disrupted by a sedentary lifestyle. If there is insufficient physical activity, it is recommended to do basic exercises in the morning.
The diet must be controlled. Frequent snacking, sudden changes in diet, overeating and other factors have a negative impact on the condition of the digestive system.
Prevention measures:
- prevention of stressful situations and timely treatment of nervous disorders;
- compliance with the rules of a balanced and rational diet;
- timely identification of the causes of gastrointestinal disorders;
- prevention of parasitic and bacterial infections;
- regular examination by a gastroenterologist;
- healthy lifestyle and sufficient physical activity;
- adherence to sleep and rest patterns.
Video - Super food for intestinal motility.
Treatment methods
Treatment of the acute phase of spastic colitis consists of prescribing medications , physiotherapy, manual therapy, and physical activity .
Medication
To reduce symptoms and stabilize the functions of the intestinal tract, the following drugs are prescribed:
- antispasmodics (“Spazgan”, “Drotaverine”);
- laxatives (“Microlax”, glycerin suppositories, “Forlax”, “Fortrans”);
- remedies for diarrhea and diarrhea (“Smecta”, “Diarol”, “Creon”);
- antidepressants or sedatives for the psychogenic nature of IBS;
- rehydration agents to reduce signs of dehydration (Regidron, Acesol);
- anti-inflammatory non-steroidal drugs (Ibuprofen, Diclofenac);
- antibiotics of different groups in case of bacterial complications;
- absorbents (“Polysorb”, “Enterosgel”);
- vitamin complexes to strengthen the body;
- coating agents for irritation of the stomach and intestines (“Gastal”, “Omeprazole”).
Medications are necessary for the treatment of concomitant diseases and require a mandatory prescription from a doctor. In pediatrics, it is important to consider age-related dosages and the risks of long-term side effects.
Physiotherapy
Physiotherapy enhances the effect of drug treatment ; in the chronic form, it helps not only relieve symptoms, but also completely eliminate discomfort. High therapeutic results are shown by oxygen baths, paraffin applications, mud wraps, galvanic currents, and ozokerite therapy.
of the lumbosacral spine and abdominal cavity has a good effect Manual therapy increases muscle tone, improves intestinal motility, and restores blood and lymph flow.
Folk remedies
Alternative medicine knows many recipes for improving intestinal health :
- Infusion No. 1 : 2 tbsp. spoons of calendula are poured into 1 liter of boiling water, left in a water bath for about an hour, and left to cool completely. Drink during the day after meals.
- Infusion No. 2 : 1 tbsp. a spoonful of anise seed is poured into a glass of boiling water, infused, filtered, and drunk three times a day an hour before meals.
- Recipe with potato juice : 2-3 fresh potato tubers are peeled, grated on a fine grater, allowed to settle, the resulting mass is filtered through a sieve, the juice is drunk in the morning on an empty stomach and at night.
For persistent constipation, you can try decoctions based on senna leaves, buckthorn, and castor oil. For diarrhea, decoctions of rice, oatmeal, and oak bark are suitable.
Diet
Nutrition correction is an important aspect of successful recovery and achieving stable remission . No special diet is required - the basic principle of nutrition is balance and moderation.
Diet rules for IBS and spastic colitis:
- eating frequent small portions;
- exclusion of foods that cause increased gas formation (grapes, cabbage);
- exclusion of ingredients that cause constipation (fresh baked goods, legumes, dry rice);
- increasing the volume of fiber and drinking water;
- exclusion of canned food, smoked meats, carbonated water, alcohol.
A gastroenterologist or clinical nutritionist will help you create an approximate menu. In the future, you can cook your own food for the whole family.