Sialadenitis is an inflammation of the salivary glands. There are three pairs of major salivary glands in the oral cavity: parotid, submandibular and sublingual. They secrete saliva and remove it through special ducts into the oral cavity to ensure normal digestion. Saliva softens food and also helps in swallowing it. The inflammatory process not only complicates the production of saliva and the process of nutrition, but also causes a lot of inconvenience due to the appearance of painful symptoms. The disease is treated by a doctor in the department of maxillofacial surgery, and in some cases by an infectious disease specialist.
Content
- Features of the salivary glands
- General symptoms of salivary gland diseases
- Classification
- Diseases of the salivary glands in children (classification)
- Diagnostic methods
- Inflammatory diseases of the salivary glands: symptoms and treatment
- Chronic processes
- Reactive dystrophic diseases
- Tumor diseases Benign neoplasms
- Malignant tumors
Symptoms
Salivary gland infections cause pain and swelling in the neck.
Most salivary gland infection symptoms last only about a week, although some swellings can last several weeks.
Symptoms usually affect parts of the head or neck and may cause:
- pain;
- skin redness;
- edema;
- unpleasant taste in the mouth;
- problems or pain when chewing or swallowing;
- chills.
For many people, symptoms worsen after eating.
Seek emergency medical help if symptoms:
- very heavy;
- interfere with drinking, swallowing and breathing;
- very painful;
- last longer than two weeks.
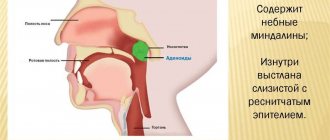
Anatomical features
The salivary glands are part of the endocrine system and are divided into small and large. The large ones include three pairs: parotid, submandibular and sublingual. The parotid is the most massive of the glands and has the shape of a triangle. Occupies the space between the cheekbone and the angle of the lower jaw, rising to the ear canal. The sublingual is located at the bottom of the mouth at the base of the tongue. The gland is enclosed in a thin fascial capsule. The submandibular is placed in the pits under the lower jaw.
Each gland has parenchyma, its own vascular network, and innervation. The body of the gland lies outside the oral mucosa, but opens the salivary ducts into it. The minor salivary glands are located on the cheeks, lips, palate and tongue.
Traditional methods of treatment: recipes for effective remedies
Drug elimination of the inflammatory process in the salivary gland is recommended to be combined with traditional medicine recipes. It is important that the products can only be used after consultation with the treating specialist.
Compresses
List of recipes for preparing compresses and rules for their use:
- Infuse 150 g of celandine roots (crushed) and 50 g of yarrow flowers in 600 ml of vodka for 7 days. Soak the gauze for the compress in this solution and apply it to the skin near the inflamed gland for 20 minutes. Carry out the procedure once a day;
- Place 40 g of celandine herb in 300 ml of boiling water and leave for 3 hours. Apply a compress for 1 hour up to 4 times a day;
- Apply homemade cottage cheese to the affected area (previously wrap it in gauze). The frequency and duration of the procedure are determined by a specialist.
Before using compresses, conduct a sensitivity test to the composition. If an allergic reaction occurs, the procedure is cancelled.
Ointments
Inflammation of the salivary gland (symptoms make it possible to determine the severity of the pathology and timely adjust treatment) can be eliminated or the course of the disease can be alleviated by using ointments.
Recipes for preparation and use:
- Mix melted pork fat (100 g) and camphor powder (20 g) until a homogeneous consistency is obtained. Apply to the skin near the gland for 3 hours once a day;
- Combine birch tar and petroleum jelly in a ratio of 10:1. Frequency of application 1 time per day for 2-3 hours;
- Place 10 g of celandine herb powder in 40 g of petroleum jelly and mix until smooth. Apply morning and evening.
If your doctor prescribes treatment using ointments and compresses. It is necessary to maintain the interval and completely remove the remaining ointment before applying the compress.
Internal funds
Recipes for internal use:
- put the mummy under the tongue for 20-30 minutes. The frequency of the procedure is 2 times a day;
- Chew 5 g of propolis for at least 10 minutes. Swallow or spit out the remainder;
- rinsing with a solution of soda;
- drink decoctions or teas of chamomile or mint.
Herbal decoctions can be used to rinse the mouth; the frequency of the procedure is not limited.
How do diseases of the salivary glands manifest?
Regardless of the cause, salivary gland diseases have a number of common symptoms:
- Changes in the amount of secretion released. More often there is a reduction or, on the contrary, an increase in production.
- Enlargement and thickening of the gland itself. Periodically occurring feeling of fullness and internal pressure.
- Local pain appears on palpation. Pain radiating to the ear, throat, tongue, depending on the location of the process.
- The ability to fully chew and swallow food and speak is impaired.
- With inflammation, the local temperature rises and redness at the site of the lesion.
- Mucous or purulent discharge from gaping ducts.
If complications occur in the form of an abscess or phlegmon, the general condition suffers: intoxication, increased body temperature.
Diagnosis of sialadenitis
People susceptible to inflammation of the salivary gland do not always know which doctor to contact for a correct diagnosis and recommendations for treatment. Based on the age of the patient, the etiology of sialadenitis and the main complications that accompany it, the disease can be diagnosed by a pediatrician, virologist, otolaryngologist, therapeutic specialists, surgeons, phthisiatricians, venereologists, rheumatologists. Therefore, to answer the question “Which doctor treats sialadenitis?”, each patient needs an individual approach and analysis. During a visual examination, local swelling is observed in the area where the secretion of the exocrine glands is located (outside or from the side of the oral cavity), and the protrusion of purulent deposits from the opening of the excretory canal when pressure is applied to it with special medical devices.
If there are signs that clearly confirm the symptoms of the disease, it is better not to self-medicate and not to postpone a visit to the doctor for a long time. If you are puzzled about what to do if you feel a general deterioration in your condition and weakness, you need to forget about self-diagnosis and undergo a general examination to identify diseases at the clinic.
Classification of diseases of the salivary glands
Diseases of the salivary glands can be divided into two main groups using the following classification.
Group | Salivary gland disease | Etiological factor |
| Infectious diseases |
|
|
| Non-communicable diseases |
|
|
Causes of siladenitis
Depending on the nature of the causes of inflammation, sialadenitis can be epidemic or non-epidemic. In the first case, we are talking about infections, and the most common cause of damage to the salivary glands is mumps, or mumps. In this case, the virus is transmitted by airborne droplets from an infected person to a healthy person.
Non-epidemic sialadenitis is most often associated with blockage of gland ducts. Such a disorder can be triggered by injury, foreign body entry, or the formation of stones - sialolithiasis.
There are factors that increase the likelihood of developing sialadenitis. Among them:
- irregular or improper oral hygiene;
- systemic, somatic diseases leading to changes in the composition and viscosity of saliva;
- past infectious diseases - viral encephalitis, influenza, ARVI, etc.;
- undergone surgical interventions.
Based on localization, unilateral and bilateral sialadenitis is distinguished, and according to the nature of inflammation, the pathology can be serous, purulent and gangrenous.
Ask a Question
Features of the development of the disease in childhood
Conventionally, there are 4 groups of pathologies of the salivary glands inherent in childhood:
- Inflammatory processes:
- specific;
- nonspecific.
- Salivary stone disease.
- Tumor-like formations
- cysts;
- benign tumors.
- Mechanical injuries.
In terms of incidence rate in children, the leading position is occupied by acute sialadenitis of viral or bacterial etiology with localization in the parotid gland.
Diagnostics
To diagnose salivary gland infections, your doctor will ask about your symptoms and perform a physical exam. Ultrasound examination may be required for a detailed examination of the parenchyma of the gland.
Risk factors for developing salivary gland infections:
- dehydration;
- a person breathes through the mouth;
- age over 65 years or newborns;
- recent surgery;
- radiation therapy or chemotherapy to the mouth, head, or neck;
- radioactive iodine therapy for the thyroid gland;
- Sjögren's syndrome;
- lymph node infections;
- renal failure;
- antihistamines, diuretics, sedatives, antipsychotics, anti-Parkinsonian and immunosuppressive drugs.
Diagnostic approach
Not all examination methods are approved and effective for various groups of pathologies. Therefore, diagnosis begins with a visual examination and medical history. Further tactics are determined depending on the preliminary diagnosis and identified symptoms.
- To establish sialadenitis, it is sufficient to determine the clinical picture and ultrasound examination.
- In nonspecific sialadenitis, family history of the disease plays an important role.
- If sialolithiasis is suspected, sialography is performed - injection of a contrast agent into the duct followed by x-ray irradiation. The images are used to determine the number and size of stones, as well as the presence of expansions and narrowings in the ducts.
- Ultrasound and MRI give a clear picture of the existing tumors.
- Biopsy is a method that reliably informs about the nature of the tumor.
- Cytological analysis of the secretion reveals a chronic, sluggish process.
Certain services are involved in the diagnosis and treatment of diseases of the maxillofacial area: pediatrics, dentistry, therapy, surgery, oncology.
Diagnosis of sialadenitis
If we talk about what diagnostic methods are used for inflammation of the salivary glands, the most common and informative are sialography and ultrasound.
In the acute course of the disease, an experienced specialist will only need the patient’s complaints and objective data that can be obtained by examining and palpating the gland. To clarify the extent of the process or differential diagnosis, ultrasound, computed tomography or magnetic resonance imaging can be used.
For chronic sialoadenitis, sialography is performed, the essence of which is to introduce contrast into the gland duct and take an x-ray. In this study, signs of inflammation of the salivary gland may be narrowing of the ducts, the presence of stones or cysts.
Diseases of the salivary glands of bacterial origin: symptoms and treatment
The parotid gland is most often affected. Bacterial inflammation is provoked by the constant microflora of the oral cavity - staphylococci and streptococci. The leading symptom is unilateral enlargement and purulent lesion. In addition, there are:
- dry mucous membranes, unpleasant purulent taste;
- lumbago in the ear area on the affected side;
- feeling of internal pressure;
- the temperature may rise to 38 degrees.
Treatment of sialadenitis is not complete without antibacterial drugs. Antibiotics are prescribed depending on the patient's age and body weight. Compresses with dimexide are applied locally. Auxiliary therapy: salivary drugs, antipyretics, painkillers. When an abscess develops, the cavity is drained. In most cases, bacterial sialadenitis is treated conservatively.
Symptoms of the disease
The main symptoms of sialadenitis include the following:
- pain while chewing;
- redness, swelling of the cheeks, neck;
- violation of taste perception;
- unpleasant taste in the mouth;
- dry mucous membranes;
- general deterioration of health;
- difficulty opening the mouth.
In acute sialadenitis, symptoms increase quickly and can also subside quickly. However, in the absence of proper treatment, the disease can become chronic, so even if you feel better, it is important to consult a dentist.
Lack of therapy can cause complications, the most common of which include the formation of ulcers (abscesses), secondary infection - the addition of a bacterial infection to a fungal infection, etc. This will require more serious intervention and long-term treatment, so you should not postpone a visit to the doctor.
Chronic sialadenitis: signs, treatment
It is observed when the parenchyma of the gland is damaged, where the inflammatory process proceeds for a long time with alternating periods of exacerbation and remission. Relapses of symptoms of a chronic disease occur when immunity decreases: after hypothermia, past illnesses, in women at certain stages of the monthly cycle. In the acute stage, the clinic is similar to the manifestations of acute sialadenitis. During the remission period, the gland can be felt as a lumpy compaction, painless and mobile. A characteristic viscous cloudy secretion is released from the ducts into the cavity, the amount of which decreases over time.
Treatment consists of two stages:
- during the remission period - support of the immune system, prophylactic intake of an oil solution of vitamin A, rinsing of the salivary ducts with antiseptic solutions;
- during an exacerbation, all therapeutic measures intended for the acute stage are carried out.
Frequent, difficult to treat relapses are an indication for surgical removal of the organ.
Chronic mumps
Acute mumps rarely becomes chronic, so chronic mumps often occurs as a primary disease.
Chronic mumps are classified into 2 groups: parenchymal and interstitial.
Chronic parenchymal parotitis
Chronic parenchymal parotitis is often asymptomatic. However, the clinic is varied. Patients may complain of swelling, pain in the gland area, and a taste of pus in the mouth. The disease lasts a long time, periodically exacerbating. Most often one gland is affected.
Objectively we can see a swelling of the gland with clear contours. Palpation is painless, the gland is dense, the surface is lumpy. When massaging the gland - saliva with pus.
Diagnostics
For diagnosis, a contrast sialogram is performed. On the sialogram you can see deformation and/or necrosis of the ducts of 2-4 orders and the parenchyma of the gland - in the image there are cavities filled with a contrast agent. As the disease progresses, the cavities merge, areas of necrosis increase until the glandular tissue is replaced by fibrous tissue.
The radiosialographic method allows us to identify the stage of the disease. At the initial stage, there is a rapid accumulation of radioactivity. In the stage of pronounced signs - slow accumulation. In the late stage, radioactivity is low.
The cytological method for diagnosing punctate and gland secretions is also used.
Treatment of chronic parenchymal parotitis
Treatment of chronic parenchymal parotitis is difficult due to the inability of dead gland tissue to regenerate. Therefore, the dentist’s task is to relieve the disease.
The gland is stimulated with ocular probes and washed every day with antibiotic solutions and massaged, freeing it from solution and pus until clear saliva appears. The ducts can also be washed with chymotrypsin, a solution of potassium iodide. Novocaine blockades and radiotherapy are indicated.
With frequent relapses, extinguishing the function of the gland is carried out by three times instillation of ethyl alcohol with increasing concentrations of 60-80-96.
Surgical treatment: parotidectomy, extirpation of the parotid duct + denervation of the auriculotemporal nerve.
Dystrophic changes
Sialosis is a special group of pathologies, most often of the sublingual and submandibular glands, the cause of which is diseases of other organs and systems.
Hypersalivation - an increased amount of secretion occurs with peptic ulcers of the digestive tract, heavy metal poisoning, and helminthic infections. It may result from a disturbance in the functioning of the parasympathetic nervous system.
Hyposalivation is a symptom of decreased secretory function, drying out of the mucous membrane. Occurs when the endocrine system malfunctions (hypothyroidism, diabetes mellitus). It is noted in chronic inflammatory diseases of the digestive system.
Completely dystrophic reactive sialadenitis is eliminated only by curing the underlying disease. Temporary measures include radiotherapy to suppress secretory function or drugs that stimulate salivation.
Neoplasms of the salivary glands
Among the representatives of benign tumors, the most common is adenoma, affecting the parotid and submandibular glands. This painless, mobile formation grows slowly without affecting the facial nerve. It can reach significant sizes, causing visual deformation of the face. Another common tumor is lipoma; in childhood, hemangiomas predominate.
A malignant neoplasm is characterized by intensive growth, germination into the body of the gland and surrounding tissues. An increase in size causes paralysis of the facial nerve and spasm of the masticatory muscles. Squamous cell carcinoma can affect both major and minor salivary glands. Specific treatment is required - a combination of chemotherapy with surgery.
Treatment of the disease
Comprehensive treatment of sialadenitis includes:
- adherence to dietary nutrition, prescribed by the treating specialist (the basis of the diet is sour dishes that enhance the production of saliva);
- medicines to increase salivation;
- the use of antibiotics orally or by injection for a bacterial disease;
- the use of antiviral drugs for viral etiology of the disease;
- use of anti-inflammatory, painkillers and antipyretic medications;
- taking immuno-strengthening drugs and vitamin complexes with reduced immunity;
- physiotherapy (compresses, electrophoresis, UHF) and massages. Prescribed for the chronic form of the disease;
- surgical intervention for severe or advanced disease or if it is necessary to remove stones from the ducts.
Depending on the form and severity of the pathology, specialists select a therapeutic complex.
Antibiotics: list of drugs, instructions for use
List of antibiotics used to eliminate the inflammatory process in the salivary gland.
| Name of drugs | For what form of disease are they used? | Dosage form | Therapeutic course | Notes |
| Dimexide | For all shapes | As a solution | Compresses using the solution are applied up to 3 times a day for no more than 20 days. | If the disease is bacterial in nature, the drug is injected into the gland itself in a hospital setting. |
| Sulfazine | In case of inflammation with the formation of fluid (not pus) | Pills | Tablets are taken 2 times a day for up to 5 days. | The course of treatment is adjusted according to the dynamics of therapy. |
| Penicillin | For purulent inflammation | Injection | Injections are given every 3 hours. The duration of treatment is selected individually. | For mild forms of the pathology, you can use the drug in tablet form. |
| Streptomycin | With inflammation accompanied by the release of pus from the salivary glands | Injection | Injections are given once a day, the concentration of the drug and the course are determined individually. | The drug has a long list of side effects, so it is used with caution. |
| Tsifran | In severe or advanced forms of pathology | IV solution and tablets | The therapeutic course is selected individually. | Due to the large list of side effects, it is recommended to use the drug in a hospital setting. |
| Azithromycin | For all shapes | Tablets and capsules | Use once a day for 3 days. | A single dosage is selected according to age and severity of the disease. |
| Oxacillin | For all shapes | Tablets and powder for solution for injection | The course of therapy lasts 10 days; single and daily dosages are selected individually. | The solution is used both for injection and for administration using a dropper. |
When prescribing antibiotics, it is recommended to familiarize yourself with contraindications and possible side effects. If necessary, a specialist will immediately replace it.
Drugs for local therapy
For local treatment the following are used:
- Dioxidin and potassium furaginate for washing the salivary ducts;
- compresses with Dimexide, camphor oil or alcohol;
- rinsing with antiseptics (Furacillin, Miramistin, Chlorhexidine);
- administration of potassium iodide, heparin using electrophoresis.
Local therapy is prohibited in the presence of elevated temperature. The dosage and course are prescribed by the attending physician.
Surgery: indications, contraindications, recovery, complications
Inflammation of the salivary gland, the symptoms of which are hidden, may lead to the need for surgical intervention.
Indications for surgery for sialadenitis:
- drug treatment did not eliminate the pathology;
- for removing or opening pustular formations;
- to remove stones or foreign substances from the salivary ducts;
- the beginning of necrosis of glandular tissue.
Sometimes complete removal of the gland may be necessary. After surgery, the patient is prescribed antibacterial agents to completely destroy the causative agent of the pathology and adheres to dietary nutrition.
The operation is prescribed only according to indications, since during its implementation there is a high risk of damage to the facial nerve. If there is an allergic reaction to the anesthetic, the procedure is cancelled.
Autoimmune processes
Sjögren's disease is a systemic pathology characterized by general damage to glandular tissue. At risk are adult women during menopause.
The main complaints presented by patients:
- dry oral mucosa;
- causeless enlargement of the salivary glands;
- fatigue, drowsiness;
- Dry eyes and increased photosensitivity are a feature of this disease.
Treatment measures are carried out in two directions: rheumatological drugs; symptomatic remedies depending on the problem present.
Why do they become inflamed?
The culprits of inflammatory changes are most often:
- Bacteria:
streptococci and corynobacteria of the oral cavity, - Staphylococcus aureus,
- E. coli and other anaerobes,
- Mycobacterium tuberculosis,
- causative agents of syphilis.
When an infectious agent enters the salivary gland, the mucous membrane swells, the salivary duct narrows, clear or purulent fluid accumulates in it, and salivation becomes difficult. If this situation persists for a long time, the gland gradually atrophies or scars, ceasing to produce and secrete a sufficient amount of saliva.
The infection most often penetrates through the mouth of the duct, less often through the blood and lymph:
- against the background of respiratory infections of the pharynx, trachea, periodontitis, skin boils
- or by contact from nearby areas (with purulent diffuse inflammation of soft tissues).
Main reasons:
- The causes of inflammation of the salivary glands in 30% of cases are mumps viruses (or Mumps).
- In addition to the infectious process, damage to the glands may be part of the program of rheumatic diseases (Sjögren's syndrome)
- and radiation damage.
- Up to 40% of all inflammations occur in dentistry.
Acute sialadenitis is often infectious.
Chronic inflammation involves the gland tissue itself (parenchymal), its connecting capsule (interstitial) or duct. In this case, the disease lasts more than 3 months with periods of heightened and subsided inflammation.
Inflammation of the salivary glands of viral origin
About 40% of viral infections occur due to mumps. This childhood disease begins suddenly with symptoms:
- chills;
- temperatures up to 40 degrees;
- severe swelling;
- the child complains of pain in the ears and head.
Viral sialadenitis, which affects the adult population, can develop rapidly if the cause is the influenza virus or herpes. Swelling of the maxillofacial area appears, the general temperature rises, and headaches and muscle pain are added. Other viral pathogens, for example, HIV, cytomegalovirus, act gradually.
The basis of therapy is antiviral drugs and immunostimulants. As a general strengthening remedy, you can use the folk method - inhaling the vapors of coniferous trees.
How to treat inflammation of the parotid salivary gland at home
In some cases, it is possible to use folk remedies in combination with traditional methods (but we should not forget that the main cause of inflammation is treated by a doctor). Proven recipes for combating sialadenitis are:
- tinctures of linden, rose hips, mint, which have a general strengthening and anti-inflammatory effect (they should be consumed warm);
- compresses from celandine, cottage cheese and grated carrots (the products are mixed in equal proportions and applied to the swollen gland 3 times a day);
- a mixture of yolk (1 piece), vegetable oil (1 tablespoon) and honey (1 teaspoon) - all ingredients are thoroughly mixed, heated over low heat until thickened, then cooled and applied as a bandage to the parotid area.
It is useful to rinse your mouth with fresh decoctions of sage, chamomile, eucalyptus and raspberry.
Despite the harmlessness of the components included in folk recipes, it is still worth seeking advice from a specialist before using them. Patients often develop an allergic reaction to the natural substances that make up many tinctures, the development of which can only be prevented by a doctor.
Inflammation of the parotid salivary gland is a serious disease that requires timely diagnosis and the prescription of a whole complex of various drugs and physiotherapy. Only a qualified specialist can establish the correct diagnosis and select the appropriate treatment. If the patient wishes to seek the help of traditional medicine, he is also recommended to visit a doctor to determine the advisability of this therapy. If all instructions are strictly followed, the patient returns to his usual lifestyle in a short time.
Gland care after recovery
Any disease is stressful for the body, rehabilitation sometimes takes months and years. To quickly restore performance, regardless of the chosen tactics (conservative or surgical), you should follow simple rules:
- maintain personal hygiene;
- eliminate foci of inflammation in a timely manner;
- take vitamin complexes for preventive purposes;
- avoid nervous fatigue.
It is important to remember that acute diseases of the salivary glands are always easier to cure than chronic forms. Timely consultation with a doctor and proper oral care will help maintain the health of the salivary glands.
What you can do at home
Treatment of inflammation of the salivary glands at home is acceptable, but only at the very initial stages of the disease or in combination with traditional methods of therapy. To avoid complications, you must consult a doctor .
To speed up recovery, you can drink and rinse your mouth with decoctions based on the following herbs:
- chamomile;
- mint;
- raspberries;
- needles;
- eucalyptus;
- feverweed;
- sage;
- elder.
You can use a folk recipe with the addition of baking soda. To do this, you need to dissolve a tablespoon of soda in a glass of warm boiled water and treat the inflamed oral cavity with a cotton pad soaked in a soda solution several times a day after meals.
An excellent folk remedy for reducing pain and inflammation is aromatherapy with essential oils of fir, pine needles, eucalyptus and many other oils.