What is urethritis in men
Urethritis is a constant background discomfort in the penis. For some it itches, itches, for others it hurts. As a rule, inflammation of the urethra is the first sign of the development of an infection, and not necessarily a sexually transmitted one. The pathogen can be introduced with your own hands, for example, from the rectum, or you can provoke the reproduction of existing ones. Stimulating factors include hypothermia, decreased immunity due to illness or stress, and alcohol intake.
Urethritis begins with mild discomfort in the penis, which increases during the day, or suddenly manifests itself after sleep with severe pain. Potency naturally decreases due to pain.
Many men tend to self-medicate or simply wait until the symptoms subside. Signs of inflammation may indeed weaken and even disappear completely over time, but this does not mean a cure. Pathogens will not go away, and the result of their hidden activity will be a violation of the structure of the urethral epithelium.
Anatomy and functions of the male urethra
The length of the male urethra varies from 18 to 20 cm, a significant part of the urethra is located inside the pelvis. In addition to the fact that the urethra performs the function of removing liquid waste from the body, sperm comes out through it.
While urination occurs, the muscles surrounding the canal relax; when ejaculation occurs, the muscles, on the contrary, tense. As in women, the canal along its entire length consists of three shells:
- external, from connective tissue;
- middle tissue, which is muscle fibers;
- internal, mucous membrane.
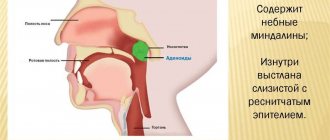
The male urethra has several anatomical parts. It emerges from the neck of the bladder and passes through the prostate. This small section of the urethra is called the prostatic part and is only 40 mm long.
Leaving the prostate gland, the channel, thinning, passes into the membranous section; it is even smaller than the previous one, has a length of 1.5 - 2 mm. This section is surrounded by muscles that form the sphincter that closes the urethra.
Next comes the bulbous section, its length is 50-60 mm. This is the part of the urethral canal that is located inside the pelvis.
It passes into the penial, or hanging, section, which is the longest, 70-80 mm in a relaxed form and passes through a significant part of the penis.
The male urinary canal ends with the glandular section, which passes inside only the head of the penis.
The last two sections are surrounded by the spongy and cavernous bodies, through which veins and vessels pass. During sexual arousal, they fill with blood and allow the penis to increase in size, stretching the urethra.
When a man reaches the peak of arousal, semen passes from the testicles through the vas deferens and all parts of the male urethra. A person cannot urinate and ejaculate at the same time.
Classification of urethritis
The classification of urethritis depends on its origin. There are two main groups: infectious and non-infectious. Infection occurs most often. Depending on the type of pathogen, it can be specific or nonspecific. The cause of specific inflammation is sexually transmitted infections. Types of urethritis:
- Gonorrheal;
- Herpetic;
- Trichomonas;
- Gardnerella;
- Ureaplasmosis;
- Mycoplasmosis;
- Chlamydial.
Nonspecific inflammation is provoked by opportunistic microorganisms. These include Escherichia coli, staphylococci, streptococci, and fungi.
Non-infectious urethritis occurs much less frequently. Its cause is an inflammatory reaction as a response to mechanical or chemical damage or tissue irritation. For example: diagnostic and therapeutic interventions in the urethra, allergies, radiation therapy (traumatic, allergic, radiation urethritis, respectively). Inflammation can develop against the background of metabolic disorders due to stagnant processes (congestive urethritis).
Depending on the source of occurrence, primary and secondary urethritis are distinguished. In the first case, inflammation begins from the urethra, in the second, pathogens penetrate from the prostate, bladder and other organs.
According to the form of its occurrence, urethritis can be acute, subacute (torpid) and chronic. In the latter case, periodic inflammations occur, which are often themselves replaced by remissions.
Depending on the location of inflammation, urethritis can be anterior, posterior or total. The anterior part is considered to be the part of the urethra from the external opening to the membranous (membranous) section. The parts of the urethra are shown schematically in the figure below.
Causes of the disease
Almost always, urethritis is an infectious inflammatory process. This implies that the pathological pathogen most often enters the urethra from the outside or from other affected tissues of the patient’s body. The most common cause of infection is unprotected sexual intercourse (about 85%). There is also a household route of infection, when infection occurs through the use of shared personal hygiene products or laundry.
If we are talking about the migration of infection within the body, then 2 mechanisms of its spread dominate:
- hematogenous - from inflamed tissues the pathogen enters the bloodstream and then settles on the urethral mucosa;
- descending – from higher located organs of the genitourinary system along with urine or sperm.
The most common causative agents of infectious urethritis are:
- Gonococcus is a paired gram-negative bacterium that can infect the mucous membranes of the urinary system, rectum, eyes and oral cavity.
- Urogenital Trichomonas is a single-celled organism that colonizes only the mucous membrane of the genital organs.
- Chlamydia is a bacterium that is an intracellular parasite of the epithelium of the urethra. May provoke the development of autoimmune reactions (Reiter's syndrome).
- Ureaplasma and mycoplasma are small types of bacteria that parasitize inside the epithelium of the urinary tract.
- Escherichia coli is a gram-negative bacterium that is normally found in the digestive system. Capable of colonizing and destroying the urethral epithelium.
- Streptococci and staphylococci are groups of gram-positive bacteria that can cause purulent inflammation with severe intoxication.
- Candida is a conditionally pathogenic fungus. Activated when the reactivity of the immune system decreases.
- Genital herpes virus. Affects the skin, as well as the mucous membranes of the urinary organs.
In less than 1% of patients, non-infectious urethritis is observed. During diagnostics, it is not possible to isolate the pathological pathogen. It is believed that the reasons for its development are:
- exposure to ionized radiation (during radiation therapy);
- allergic reactions to topical use of ointments;
- traumatization of the urethra by the introduction of foreign objects into it;
- thermal or chemical damage due to self-washing of the urethra with solutions or antiseptics.
Risk factors for developing urethritis
The conducted studies made it possible to identify factors that may contribute to the development of urethritis:
- urological surgery;
- abnormalities in the development of the urethra;
- placement of a catheter in the bladder (longer than 48 hours);
- obstruction of the urethra with partial or complete disruption of its patency (urolithiasis, oncological processes);
- diabetes mellitus, if therapy fails to normalize blood glucose levels
- sexual intercourse with frequent changes of partners;
- diseases and abnormalities of connective tissue development;
- end-stage renal failure;
- hormonal disorders;
- the need for long-term use of drugs that suppress the immune system;
- oncological pathologies, regardless of their location.
Symptoms of urethritis in men
All types of infectious urethritis in the acute phase manifest themselves approximately equally. Main symptoms:
- Mucous or purulent discharge;
- Redness, swelling, sticking of the urethral sponges, which is why in the morning there is a bifurcated stream of urine;
- Stinging during urination, itching and dull pain after;
- Discomfort in the penis during erection and during sexual intercourse.
The spread of the inflammatory process to the prostate and bladder is indicated by an increased urge to urinate and the appearance of diffuse pain in the perineum and rectum.
The table below shows the characteristic signs of various types of urethritis, identified on the basis of a clinical study of a group of patients.
Symptoms of the most common types of urethritis
Characteristic symptoms include gonorrheal, trichomonas, and fungal urethritis. These types of inflammation of the urethra can be called classic.
Trichomonas
The incubation period of Trichomonas urethritis lasts from 5 to 15 days. Symptoms: mild itching in the urethra, foamy whitish discharge. For some men, this type of inflammation causes virtually no symptoms.
Urologist, dermatovenerologist Sergei Gennadievich Lenkin tells more about the causes and symptoms of the trichomonas form of urethritis
Gonorrheal
Infection occurs through sexual contact, less commonly through household contact with common hygiene items or contact with biological fluids. The first signs appear after 3-7 days, but it happens that inflammation develops after 2-3 weeks. The main symptom of acute gonorrheal urethritis is yellow-gray discharge and burning in the urethra. If the inflammation is localized in the anterior section, then the patient’s condition is normal. When it moves to the back, signs of intoxication appear: weakness, temperature rise to 38-39 ˚C.
When the prostate is involved, gonorrheal urethritis often becomes chronic. Inflammation is accompanied by a slight tingling sensation at the beginning of urination, a slight burning sensation, and occasional itching. In the morning there is scanty discharge. Gonorrheal urethritis provokes inflammation of the urethral glands (litreitis). In the first portion of urine, hooked purulent clots become noticeable. Blockage of the glands with pus leads to the formation of small foci of abscess, which can be felt as painful lumps. Chronic gonorrheal urethritis can lead to difficulty in the outflow of urine, deterioration of the general condition, and severe pain when urinating.
Chlamydial
Chlamydia hides inside cells and spreads throughout the body, affecting joints and the conjunctiva of the eyes. The inflammation is sluggish; 20-30% of men have no symptoms at all. Chlamydia is found in scrapings from the walls of the urethra in the form of crescent-shaped cellular inclusions.
Candidomycosis
This type of urethritis develops after a long course of antibiotics or unprotected sex with a woman suffering from fungal inflammation of the vagina. The main signs: mild itching in the urethra, white discharge accumulating on the head and behind the foreskin.
Diet
You will have to adhere to the rules and norms of nutrition not only during treatment, but also for several months after it. Any foods that irritate the mucous membranes should be completely excluded from the diet. These are fried foods, canned food, pickled and smoked foods.
A prerequisite is to limit salt intake.
It is important for the patient to drink a lot (water, decoctions, fruit drinks, compotes) and stop bad habits. Alcohol is strictly prohibited in the treatment of urethritis.
Treatment of urethritis (especially chronic) can be lengthy, and incorrectly selected therapy can lead to complications and sad consequences. Therefore, you should not start the course of the disease, or even better, prevent its occurrence at all, always using contraception and taking a responsible attitude towards your own health.
For information on the symptoms and treatment of urethritis in men, watch the video:
Useful articles on the topic:
Spermogram: preparation for delivery and interpretation of the analysis Treatment of chlamydia in men Trichomoniasis in men Symptoms of gonorrhea in men
This article has been verified by a current qualified physician, Inna Zhikhoreva, and can be considered a reliable source of information for site users.
Rate how helpful this article was
5 2 people voted, average rating 5
Did you like the article? Save it to your wall so you don’t lose it!
Diagnostics
With signs of urethritis, contact a urologist or andrologist. First, the doctor conducts an external examination of the penis, assesses the condition of the sponges and the nature of the discharge, then palpates the urethra. By palpation, you can detect soft areas of inflammation, painful compactions, and protrusions.
The main material for laboratory research is scraping from the urethra. It is taken after 4 hours of abstaining from urination. To diagnose chlamydia, it is recommended to use two methods: PCR and PIF.
What tests should be taken if you suspect urethritis, says urologist, dermatovenerologist Sergey Gennadievich Lenkin
After taking a smear, the patient gives a two-glass urine sample according to Thompson. If threads of pus and cloudy flakes are present only in the first glass, then the inflammation is localized in the anterior urethra. If red blood cells are detected, an endoscopic examination (urethroscopy) is prescribed.
Other diagnostic methods: palpation and ultrasound of the prostate, secretion analysis, general analysis of urine and blood, uroflowmetry, urethrocystoscopy. Chronic inflammation of the urethra is often accompanied by sluggish pyelonephritis, prostatitis, diabetes mellitus, and paraurethral fibrosis. These pathologies are in most cases discovered during diagnosis.
Redness of the urethra with urethral condylomas
Papillomavirus is a sexually transmitted pathogen. It causes condylomas to appear on the genitals and sometimes inside the urethra.
The incubation period for this disease is very long.
Redness of the urethra after sex does not appear immediately, but on average after six months. The patient feels itching. Sometimes there are no subjective symptoms.
Condylomas appear in the urethra. They arise in its distal part.
They may be clearly visible upon examination. Inside the urethra, condylomas are often injured. Because they are constantly exposed to a stream of urine.
Damage to the mucous membrane may appear, and a bacterial infection may develop.
Men often have difficulty urinating. Therefore, such condylomas must be removed.
Redness of the urethra if the penis is rubbed
The cause of inflammation is not always an infection. This can be traumatic.
Redness of the urethra can develop as a result of a one-time strong mechanical impact. In other cases, it is caused by low-intensity physical irritation that continues for a long time. It could be chafing.
The reason is prolonged sex, uncomfortable underwear or trousers. Redness, swelling, and soreness occur. Erosion may appear. Usually, an unpleasant odor and discharge are not typical.
Medical procedures and redness of the urethra. As a result of medical procedures, the urethra may become red and inflamed. Most often this is a temporary phenomenon. It is not dangerous and goes away on its own within a few days.
Redness of the urethra may occur after:
- Miramistin (antiseptic to prevent sexually transmitted infections)
- smear for infection
- instillations (urethral lavage)
- urethroscopy
- dilation of the urethra
- removal of intraurethral condylomas
- bladder catheterization
- performing any transurethral surgical interventions
Redness of the urethra is a natural reaction to a chemical or physical irritant. Its occurrence does not indicate infection.
You may experience discomfort when urinating for several days. Then the mucous membrane regenerates and the symptoms go away. Sometimes allergic reactions develop as a result of the use of medications. For example, when using intraurethral Miramistin or chlorhexidine.
Patients often use these antiseptics to prevent sexually transmitted diseases. But they irritate the mucous membrane. Sometimes they can provoke hypersensitivity reactions.
Then symptoms of allergic urethritis develop. Transparent discharge appears. There is itching and burning sensation.
Redness of the urethra: tests and diagnosis
To diagnose redness of the urethra, various methods are used: laboratory, instrumental. Their goal is to find out the cause of inflammation. If it is infectious, it is necessary to determine the causative agent of the pathological process.
Topical diagnostics are carried out to find out which organs are involved in the process. Often this is not only the urethra, but also the internal genital organs.
If the urethra is red, a smear is taken from it. It is examined under a microscope. If there are active signs of inflammation and discharge, sometimes it is possible to detect the pathogen. The smear may reveal Candida, Trichomonas, and gonococci fungi.
Gonorrhea is detected microscopically more often in men. Especially if they have copious discharge.
Trichomonas are detected more often in women. Moreover, it is very rare in urethral smears. Much more often - in vaginal ones.
Candida can be detected in patients of any gender. They are clearly visible if there is a white coating in the area of the urethral sponges.
If a nonspecific nature of the inflammatory process is suspected, bacteriological culture is performed. Colonies of bacteria grow on the nutrient medium. They are identified.
The study allows not only to determine the type of pathogen. It also makes it possible to assess the sensitivity of various bacteria to antibiotics, which greatly facilitates the choice of treatment regimen.
If sexually transmitted infections are suspected, PCR is done for the most common pathogens. In this way, any viruses or bacteria can be detected.
Using PCR, chlamydia, ureaplasmosis, trichomoniasis, gonorrhea, and herpes are detected. It is possible to establish the type of papillomavirus to determine the risk of malignant degeneration of condylomas.
Redness of the urethra: treatment
Treatment for redness of the urethra depends on the reason for its occurrence. It is usually caused by sexually transmitted infections. It could be gonorrhea.
Then cephalosporins are prescribed for treatment, usually ceftriaxone. If the pathology is caused by Trichomonas, nitroimidazoles are used.
In case of fungal infection of the urethra, fluconazole is prescribed orally. Clotrimazole can be used externally. If chlamydia is detected, doxycycline is used orally.
Herpes infection is treated with acyclovir and other drugs in this group. The drugs are used both internally and externally in the form of a cream.
Nonspecific urethritis requires antibiotic therapy. Penicillins, fluoroquinolones, and tetracyclines may be prescribed. Additionally, local treatment is used.
The urethra is washed with silver solutions. This is done 2 times a week.
The procedure is performed by a doctor using a soft catheter. If condylomas are detected, their removal is required. Inside the urethra, they are evaporated with a laser or frozen with liquid nitrogen. After necrosis of the condyloma tissue, it gradually dies. A scab remains at the site of formation. After 1-2 weeks, all damage heals completely.
Some patients try to treat redness of the urethra with folk remedies. We do not recommend doing this. We have already found out that there can be many reasons for redness of the urethra. There is no universal treatment that could eliminate all etiological factors.
For effective treatment, the pathogen must be identified. And then choose therapy using effective drugs. Folk remedies will not help here, and delaying the start of treatment can result in complications.
How to treat urethritis in men
Treatment is carried out strictly under the supervision of a doctor. The treatment regimen is prescribed individually according to test results.
At home
A prerequisite for the effectiveness of treatment: temporary cessation of sexual activity, limitation of physical activity, avoidance of alcohol, spicy and salty foods. You should drink more pure water and herbal infusions. It is important to maintain genital hygiene: regularly wash the head and foreskin with a weak solution of manganese, furatsilin, chlorhexidine.
Medicines
To treat infectious urethritis, antibiotics are used, which are selected in accordance with test results.
For gonorrheal inflammation, cephalosporins and fluoroquinolones are prescribed. In cases where granulations begin to grow inside the urethra, solutions of collargol and silver nitrate are poured inside. With the development of cicatricial processes, forced dilatation (bougienage) of the urethra is used. A week later, an analysis of the discharge is performed. If gonococci are not detected, then provocation is carried out (exposure to various provoking factors). After which, over the course of 3 days, biomaterials are taken and examined: prostatic juice, smears from the urethra, urine. If there are no pathogens and leukocytes, then the provocation is repeated after a month. A total of 3 control examinations are performed. If the results are negative, then the man is removed from the register.
With timely treatment, the prognosis is favorable. If the inflammation has become chronic, then there is a high probability of developing chronic prostatitis, vesiculitis, inflammation of the testicles and appendages. If adhesions have formed in the vas deferens, obstructive infertility is diagnosed.
Trichomonas urethritis is treated with specific drugs: Trichopolum, Flagyl, Metronidazole, Tibiral. In the chronic form, local therapy is prescribed: for 5 days, a 1% solution of Trichomonacid is poured into the urethra and held for 10-15 minutes.
Trichopolum is an antimicrobial drug prescribed for the treatment of diseases caused by protozoa. Price from 77 rub.
Treatment of chlamydial inflammation is complicated by the fact that not all antibacterial drugs can penetrate the cell wall, which is why the disease often recurs. Macrolides (Sumamed, Azithromycin), tetracyclines, fluoroquinolones are prescribed. Tetracycline, Dimexide, and ozonated saline solution are poured into the urethra. The effectiveness of therapy is increased with the help of corticosteroids (Prednisolone, Dexamethasone). The course lasts 2-3 weeks. Additionally, vitamins “Aevit” and “Bifidumbacterin” are prescribed.
For fungal urethritis, specific drugs are used: Lamisil, Nystatin, Fluconazole. A solution of Levorin or Clotrimazole is poured into the urethra.
Ureaplasmas are sensitive to tetracyclines, macrolides, gardnerella - to cephalosporins, sulfonamides, ampicillin, clindamycin. For nonspecific urethritis caused by bacilli, staphylococci, streptococci, broad-spectrum antibiotics (Levomycetin) are prescribed.
Complications
Complications arise due to pathological changes in the inflamed tissues of the urethral canal and the spread of infection. After purulent melting, adhesions and fibrous foci are formed. Consequences of urethritis:
- Difficulty urinating;
- Mental and sexual disorders;
- The development of inflammation of other organs of the genitourinary system, head and foreskin.
In some cases, acute urinary retention occurs, which is eliminated by installing a cystostomy (urine drainage through the abdominal wall).
Drainage tube (cystostomy) for urinary retention
Redness of the urethra with prostatitis
Prostatitis itself does not manifest itself as redness of the urethra. But it is very often combined with urethritis.
On the one hand, with prostatitis exudate appears. It enters the urethra because it is anatomically connected to it. The secretion of the prostate gland is released into the external environment through the urethra. Therefore, it becomes infected, inflamed and reddened.
On the other hand, with primary damage to the urethra, the infection can spread upward. It often reaches the prostate gland. Prostatitis can be acute and chronic.
Acute is most often caused by gram-negative flora. It enters the prostate by hematogenous or lymphogenous route.
Main symptoms:
- heaviness in the rectum
- pelvic pain
- difficulty urinating
- general intoxication (fever, headache, etc.)
Chronic prostatitis often occurs as a result of infection with an STD. The infection enters the prostate through an ascending route.
Symptoms are mild. Dysuria, redness of the urethra, and nagging pain in the pelvis may be observed.
Reviews about the treatment
Acute urethritis can be successfully treated with antibiotics, provided they are prescribed correctly. The biggest problem for men is the chronic form of inflammation, which is difficult to respond to antibiotic therapy. In some cases, doctors themselves carry out an insufficiently complete diagnosis and prescribe superficial treatment. Below is a question from a patient exhausted by urethritis on the forum.
In response, the doctor recommended donating prostate juice for bacterial culture and undergoing a course of treatment for prostatitis.
Advice from a urologist for a man with suspected candidiasis:
Stages of the disease
Fresh (acute) urethritis occurs in three stages:
- The incubation period is the time from the moment of infection to the onset of the disease, lasting from 1-2 days to 2 weeks.
- Period of severe symptoms.
- The period of convalescence is a complete recovery under favorable conditions (treatment) or chronicization of the process, i.e., the transition of the disease to a chronic form in an unfavorable variant.
The consequence of gonococcal urethritis in men can be a stricture (narrowing) of the urethra. Chlamydial urethritis can cause the development of Reiter's syndrome.
In the clinical picture of chronic urethritis, three alternating periods are also distinguished:
- Exacerbation (symptoms are pronounced).
- Remission (asymptomatic, but the inflammatory process is not resolved, it continues in an indirect form).
- Unstable remission (scanty clinical manifestations).