- Symptoms
- Diagnostics
- Treatment
- Prevention
Mastitis is an inflammatory lesion of the mammary gland, occurring in acute or chronic form.
Occurs when tissues become infected with pathogenic microflora and tends to spread. There are several ways pathogenic microflora enters breast tissue:
- entry of a microbial agent through dilated mammary ducts in the postpartum period;
- introduction of the microbe as a result of trauma to the mammary gland or through cracks in the nipples;
- spread of the pathogen from nearby affected areas.
Thus, in accordance with the mechanism of infection, they distinguish:
- lactation mastitis;
- non-lactational mastitis.
It is generally accepted that the main causative agent of this disease is Staphylococcus aureus. It is he who, in its majority, provokes the development of purulent-inflammatory processes in humans. However, favorable conditions are necessary for its penetration. These include:
- mastopathy disease;
- postoperative tissue changes;
- congenital anomalies of breast development;
- difficult pregnancy, childbirth;
- presence of concomitant diseases;
- past acute viral and bacterial infections.
Acute and chronic mastitis: causes of pathology
The main cause of the disease is an infectious process. The main culprit is Staphylococcus aureus, less often other types of bacteria (Staphylococcus epidermidis, streptococci, enterococci, E. coli). The infection is activated under the influence of unfavorable factors - both external and internal. Among them:
- Hormonal imbalance in the reproductive system weakens the body's defenses. Reason: prolonged mental and physical stress, treatment with hormonal drugs, steroid use (in particular among athletes), chronic endocrine diseases.
- Decreased immunity - gives the green light to various infections, including opportunistic microorganisms. Reason: hypothermia, poor diet, stress, lack of vitamins, microelements, fresh air.
- Stagnation (lactostasis in lactating women) - a violation of the outflow of milk creates a favorable environment for the development of bacteria. Reason: inept pumping of milk, improper attachment of the baby to the breast, tight bra, tight clothing, severe lack of physical activity.
- Various pathologies of the mammary glands (fibrocystic mastopathy, complications after plastic surgery, etc.).
Common provoking factors include poor ecology, stress, sudden climate change, and failure to comply with hygiene rules. In nulliparous women, the cause of the pathology can be unsuccessful piercing and too active sexual games with injury to the nipples.
Should I continue or stop breastfeeding if I have mastitis?
As for maintaining breastfeeding during mastitis, several decades ago the recommendations of pediatricians and gynecologists were categorical: interrupt breastfeeding for the period of treatment of mastitis.
Today, the situation has turned 180 degrees and all breastfeeding specialists are demanding that babies be breastfed, no matter what. It seems that the truth, as usual, is closer to the middle or, at a minimum, should be based on a set of arguments for and against. It is worth making a distinction between feeding the baby this milk and maintaining lactation as such:
Maintaining lactation
Lactation should be maintained in all cases where possible, since regular milk flow is very important; according to some data, only 4% of cases of acute mastitis, while maintaining lactation and feeding the child, progresses to an abscess or purulent mastitis.
Feeding a baby with breast milk with mastitis
And when it comes to feeding a baby with breast milk, it is worth weighing the risks and benefits for the baby of not breastfeeding and the impact of the mother's treatment. In each clinical case, the issue is resolved individually:
- With non-infectious mastitis, which is not so different from lactostasis, breastfeeding cannot be stopped. Of course, in conjunction with rational pumping (not to the last drop, but as necessary to avoid hyperlactation), gentle therapeutic massage and anti-inflammatory therapy (Ibuprofen, Traumeel, ultrasound).
- If we are talking about an infectious process. Here you will have to proceed from how severely the mother’s general condition is suffering (it is difficult to feed with a temperature of 40, wild pain and axillary lymphadenitis).
The second point is purulent discharge from the nipples. Breastfeeding instructors persistently argue that pus is just dead bacteria and white blood cells and that feeding a baby with it is not contraindicated. But excuse me, we object, why is purulent discharge still sown in bacteriological laboratories, obtaining good bacterial growth and determining the sensitivity of pathogens to antibiotics? Purulent discharge from the nipples should:
- or express very carefully before feeding
- or become an obstacle to continuing breastfeeding during the period of treatment for purulent mastitis.
You can maintain lactation during the treatment period with the help of regular pumping until the problem is resolved, but during this period, feeding the child and then treating intestinal disorders against the background of staphylococci acquired during feeding, as well as from the influence of antibiotic therapy, is an extremely unfavorable matter for the baby, long-term and costly.
Almost all antibacterial drugs administered to a nursing woman enter breast milk and the baby’s body, causing adverse effects - toxic and allergic reactions, and the normal microflora of the gastrointestinal tract suffers.
Depending on different pharmaceutical groups, some antibiotics easily penetrate into milk and create high concentrations of active substances, others pass in small quantities, which does not pose a real threat to the baby and is therefore approved for use during breastfeeding.
Types and forms of mastitis
There are acute and chronic forms of the disease. The first includes lactation or postpartum mastitis with pronounced symptoms. An example of the second is a non-lactation type of pathology, which is not associated with the period of breastfeeding and is not clearly linked to gender and age.
On a note! According to statistics, lactation mastitis occurs on average in 5% of lactating women. In unfavorable regions, this figure can rise to 15%. Moreover, 85% of all cases of the disease occur in first-time mothers. Non-lactation mastitis is less common (no more than 10% of the total number of all manifestations of mastitis) and can affect women of different ages, men, and children.
There are 3 clinical forms of the disease:
- Acute postpartum – develops against the background of congestion in nursing women.
- Plasma cell - more typical for multiparous women in the period after the end of lactation, as well as during hormonal changes during menopause. The disease occurs in a moderately acute form, with mild symptoms, which makes it similar to tumor pathologies of the mammary gland
- Neonatal mastitis – observed in infants of both sexes as a result of residual effects of maternal hormones (is a complication of physiological mastopathy in newborns).
On a note! Separately, it is worth mentioning cases of mastitis in men, which are considered a direct consequence of chronic endocrine diseases and hormone imbalance. The pathology manifests itself in the presence of diabetes mellitus, gynecomastia, tumors of the genital organs, as well as with long-term use of steroids in bodybuilders.
Depending on the nature of the inflammation, there are several types of mastitis:
- serous;
- infiltration;
- purulent.
Together they form 3 successive stages of development of the inflammatory process - from the appearance of the first symptoms in the form of serous exudate to active suppuration of the area of inflammation with the discharge of pus. Based on the type of localization of purulent structures, two more forms can be distinguished:
- phlegmonous - with the spread of pus throughout the entire volume of the affected tissue;
- abscess - with clear localization and delimitation of purulent contents from adjacent tissues.
In advanced cases, a gangrenous form may develop with tissue necrosis and septic complications, which poses a high risk to the patient’s life. The only way out in this situation is complete removal of the mammary gland and adjacent lymph nodes.
What can you do to prevent mastitis?
As with any health problem, the best cure for mastitis is prevention. Breastfeed your baby frequently to prevent clogged milk ducts. If the baby does not feed regularly enough, it is necessary to express the milk with a breast pump. Don't let an inflammatory process like mastitis ruin the wonderful mother-baby bonding experience that comes from breastfeeding. The methods listed in this article can help you cure mastitis naturally and leave only good memories of this period of motherhood.
Mastitis: symptoms
The composition of the symptom complex depends on the stage of the disease:
- Stage 1 – serous: slight hyperemia and swelling of the glandular tissue, pain on palpation (may radiate to the area of the axillary lymph nodes).
- Stage 2 - infiltration: swelling and soreness increase, a compaction is clearly palpable in the glandular tissue, the temperature rises sharply, regional lymph nodes enlarge, signs of intoxication appear, and general well-being worsens.
- Stage 3 – purulent: the severity of symptoms reaches its peak, purulent exudate appears. In the lactation form, purulent-bloody discharge can be seen in the milk (in this case, breastfeeding must be stopped).
In severe cases of mastitis, the symptoms may become more complicated - a general increase in temperature, fever, intoxication, and enlarged axillary lymph nodes are possible. In the absence of treatment, a gangrenous form develops with septic damage to the body.
Is it possible to make compresses for mastitis or use ointments?
When the first signs of lactostasis or mastitis appear, you should consult a doctor, establish a diagnosis, determine the stage of the disease and discuss treatment methods.
Non-infectious mastitis - warming compresses can only be used for lactostasis and non-infectious mastitis in complex treatment. It is possible to use semi-alcohol dressings on the affected area at night, cabbage leaves with honey, burdock leaves, etc. After the compress, rinse the chest with warm water. You can also use homeopathic gel Traumeel.
For purulent mastitis, warm compresses and the use of ointments can aggravate the course of the disease and are therefore not recommended.
Diagnosis of the disease
Acute mastitis is diagnosed during a medical examination and tissue palpation. The procedure allows you to find out the localization of the inflammatory process, check for symptoms, and collect information on your medical history. The chronic form requires differential diagnosis with a tumor process, mastopathy and other diseases of the mammary glands. Based on the results of the preliminary diagnosis, the doctor will refer you for additional examination using instrumental and laboratory methods.
Basic techniques:
- Ultrasound of the mammary glands - reveals characteristic thickening of the subcutaneous tissue, expansion of the milk ducts, shows the location of infiltration zones, abscesses and necrotic areas;
- aspiration biopsy of the breast with histological examination of the inflammatory infiltrate;
- collecting milk for bacteriological testing (for lactation mastitis);
- mammography (rarely prescribed, only in controversial cases of chronic disease).
Causes of the disease
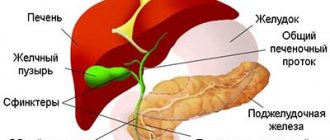
Inflammatory processes during mastitis occur when affected by a purulent infection,
in most cases it is Staphylococcus aureus. Such a microorganism leads to the development of severe suppuration in humans: from skin diseases (boils, acne, pimples) to fatal disorders in internal organs (pneumonia, meningitis, and osteomyelitis).
Any inflammatory process that occurs due to Staphylococcus aureus can lead to severe difficulties in the form of septic endocarditis, sepsis or infectious-toxic shock.
Over the last period of time, mastitis has become even more common due to the association of microorganisms. Combinations of Staphylococcus aureus with gram-negative Escherichia coli (a microorganism common in the outside world that normally lives inside the body’s intestines) have become more frequent.
Elimination of symptoms and treatment of mastitis
Mastitis is treated by a gynecologist and mammologist. In some cases, the help of an endocrinologist and surgeon will be required. A timely visit to a doctor is of great importance, since when mastitis passes into a purulent abscess form, surgical intervention becomes inevitable. In this case, an opening of the purulent focus is prescribed, followed by tissue drainage. Serous and infiltration mastitis can be cured using conservative techniques.
Attention! During treatment for lactation mastitis, you should stop breastfeeding. Reason: Breast milk contains bacterial toxins and antibiotics, which can harm the baby.
The main groups of drugs for drug treatment:
- antibiotics – to suppress and/or completely eliminate the infectious pathogen;
- painkillers and antipyretics as symptomatic treatment;
- drugs that suppress lactation (when the pathology becomes purulent);
- immunostimulants and vitamins - to maintain the body and improve resistance to infections;
- detoxification agents.
Ultrasound, magnetic therapy, phonophoresis, and darsonval are used as physical procedures. At home, cool compresses, including those based on herbs with an anti-inflammatory effect, are actively used to relieve pain and reduce inflammation.
Attention! Self-medication of mastitis is unacceptable - any miscalculation can lead to serious complications, including sepsis and necrosis. Advanced forms may require complete removal of the gland and adjacent lymph nodes. Home therapy methods can only be used after consultation with a doctor as an accompanying treatment.
About the lactation period
The shape, size and position of the breast are very individual, vary widely within normal limits and depend on:
- age
- phases of the menstrual cycle
- general build
- lifestyle
- state of the woman's reproductive system.
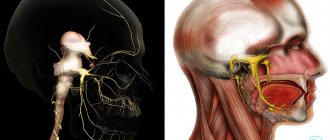
Anatomy of the mammary glands
A woman’s breast has a lobed structure; large lobes are separated by spaces of connective tissue into 20–40 segments, each of which consists of alveoli. The alveolus itself is lined with a single-layer glandular epithelium with an excretory duct, which are connected to each other into large ducts in which breast milk accumulates. The lobar ducts, merging with each other, open as excretory ducts at the tip of the nipple.
In the area of the border of the halos, the ducts have extensions called lacteal sinuses. Around the glandular structures, the breast space is filled with adipose tissue, which determines its size and also shape, along with the development of the glandular lobules themselves. A woman’s breast is surrounded by a whole complex of lymph nodes, so when the breasts become inflamed, they increase in size and are painful. Lymph nodes into which lymph flows from the mammary gland:
- axillary (97% outflow)
- supraclavicular
- subclavian
- parasternal
- mediastinal and bronchopulmonary
What happens to the breasts during pregnancy and immediately after the birth of the baby
Synthesis and secretion of breast milk for feeding the baby starting from the second trimester of pregnancy, when the production of colostrum is gradually activated.
- Colostrum - more like whey than regular milk, with a high content of proteins and fats, is secreted until the first 2-3 days after the birth of the child, and then is replaced by transitional and mature milk.
- The maximum amount of milk matures by 6–12 days of the postpartum period.
- Stabilization period - when the optimal amount of milk secreted for the baby’s nutrition occurs, this period lasts during the first 3 to 6 months of breastfeeding.
- The average duration of lactation ranges from 5 to 24 months.
Prevention
Measures to prevent lactation mastitis in women:
- Prevent stagnation of breast milk. Get advice about breastfeeding and, if necessary, pumping using special breast pumps.
- Attach your baby to the breast correctly. Make sure it completely covers the nipple and areola. Do not allow breastfeeding to be done “in vain”, without milk being sucked out.
- Maintain breast hygiene. Carefully prepare your nipples for feeding - this will prevent the appearance of microcracks and their subsequent infection.
- Try to visit a mammologist regularly - an experienced doctor will be able to determine the onset of the disease before the first unpleasant symptoms appear. This will greatly simplify treatment.
To prevent non-lactation mastitis, you should carefully monitor the general condition of the body. The trigger for pathology can be constant stress, hypothermia, poor environment, and too little physical activity. An important part of the prevention of inflammation of the mammary glands (including for men and children) is timely diagnosis and timely elimination of hormone imbalance.
When to Seek Medical Help
Seek help from your doctor if you feel any suspicious breast lumps, whether you are breastfeeding or not. You need to seek help if:
- You have suspicious discharge from your nipples;
- Chest pain negatively affects daily activities;
- Chest pain lasts inexplicably for a long time;
- You also have symptoms such as redness, swelling, pain that interferes with breastfeeding, painful lumps in the breast that do not go away after breastfeeding;
- If you suspect a breast infection, seek professional help immediately.
The symptoms of mastitis in your case should be assessed at a hospital department if the chest pain is associated with other signs of infection (for example, high body temperature, swelling or redness in the breasts). The following symptoms require emergency treatment:
- Constant high body temperature – over +38 °C;
- Nausea or vomiting that prevents you from taking your prescribed antibiotics;
- Pus released when expressing milk;
- Radiating red stripes on the chest;
- Dizziness, fainting, or confusion.
Lactational form
If an infection with lactose mastitis occurs, then its source is considered to be hidden bacteria coming from medical personnel, roommates or loved ones (from 20 to 40% of people are carriers of Staphylococcus aureus). The disease spreads through contaminated everyday personal items: care products, bedding, clothing.
In addition, a child sick with staphylococcus is also considered the source of infection for mastitis, for example, in the case of pyoderma (pustular rashes on the surface of the skin) or in umbilical sepsis.
It must be said that getting a staphylococcus infection on the skin of the chest does not always contribute to the development of mastitis. To be affected by an infectious-inflammatory process, all favorable conditions for its spread are needed - anatomical and functional.
Local anatomical factors that lead to this process include:
- mastopathy;
- genetic defects in body structure (lobed or inverted nipple);
- gross scar lesions of the breast, which can persist after suffering severe forms of mastitis, or after surgery for a benign neoplasm in the body.
If we talk about functional factors that lead to purulent mastitis, then their spectrum is more extensive. These include:
- difficulties in bearing a child (development of premature birth, late pregnancy, threat of miscarriage, acute form of toxicosis);
- processes of exacerbation of relevant diseases;
- development of puerperal fever;
- exacerbation of existing diseases;
- disorders in a woman’s nervous system, difficulty sleeping, stress;
- complications in labor (first birth with a large baby, manual separation of the placenta, deformation of the paths along which the fetus passes at birth, severe blood loss during childbirth).
Women who give birth for the first time are at risk of mastitis due to the fact that their glandular tissue that produces milk is poorly formed, there are physiological deficiencies in the glandular ducts, and the nipple is poorly formed.
In addition, great importance should be given to the fact that a first-time mother does not have any experience in breastfeeding a child, and also does not have the skill of properly expressing milk.
Acute pathology
With regular and correct expression of milk, bacteria that constantly fall on the breast are washed away and simply do not have time to develop an infection.
Traditional treatment at home
Alternative treatment is appropriate only for lactostasis and serous form of mastitis. Home remedies must be combined with antibacterial therapy and immunomodulators. The effectiveness of traditional treatment has not been proven, but many women use improvised remedies to reduce swelling, pain and redness of the breasts.
Compresses
Compresses for mastitis are prepared from medicinal herbs and vegetables. There are several options:
- pumpkin pulp boiled in milk;
- a mixture of baked onion and flaxseed oil;
- decoction of sweet clover or black alder leaves;
- flatbread made from flower honey and wheat flour;
- soybean puree;
- paste made from potato starch with olive and linseed oil.
The compresses are kept for 40 minutes to 2–3 hours. Warm lotions are prohibited for purulent mastitis.
Ointments
Infectious mastitis is treated with ichthyol ointment and Vishnevsky ointment. The drugs are applied directly to the inflamed area in the form of compresses. Ichthyol ointment is effective at the initial stage. It soothes itching, inflammation and slows down the proliferation of microbes.
Vishnevsky ointment is used for infectious mastitis, as well as in the postoperative period after opening an abscess. The product eliminates inflammation and accelerates the regeneration of damaged nipples and sutures.
Cabbage wraps
Cabbage leaves are useful for engorgement and redness of the breast. They are cooled to room temperature and applied for 1–2 hours, 6–7 times a day. Cabbage for a compress can be greased with natural butter, grated beets or yogurt.
Salt compresses
A salt compress is prepared from 50 ml of water and 30–35 g of regular or sea salt. The solution should be warm, but not hot. Cotton napkins with holes for the nipples are moistened in it and applied to the breast for 2-3 hours. The compress is contraindicated for cracks and wounds.
Water massage
Water massage is recommended for lactostasis. The procedure is carried out in the shower. The pressure should be average or maximum, the water temperature should be 37–42 degrees. The direction of the jet is from the center of the chest to the periphery. The massage is done in a circular motion and lasts 5–8 minutes.
Rubbing with alcohol
Alcohol compresses are contraindicated for mastitis. They will only increase inflammation. Rubbing the reddened area with alcohol can only be done after consulting a gynecologist.
Ice
In the first 4–5 days, it is recommended to apply an ice pack to the breast. Cold slows down the growth of bacteria and relieves discomfort. Ice is wrapped in a towel or scarf to prevent frostbite and kept for no longer than 3 minutes after each feeding.
Honey
Honey compresses and rubbing disinfect, prevent the proliferation of microbes and have wound-healing properties. Honey can be used in several ways:
- mix with onion juice;
- add to a flatbread made from wheat flour and vegetable oil;
- combine with dried duckweed and aloe juice;
- mix with sesame seeds and olive oil.
Honey compresses are used only cold and no more than 2 times a day.
Essential oils
Essential oils are recommended for non-lactation mastitis. They are contraindicated for breastfeeding women. Essential compounds can cause allergies in a child.
Oils are added to cold compresses and lozenges. The most effective:
- mint – reduces fever, has antimicrobial properties;
- camphor – relieves pain and reduces inflammation;
- juniper – disinfects and removes swelling;
- fir – destroys staphylococcus, suppresses inflammation.
Add 2-3 drops of essential oil to the compresses. Before using the component, be sure to do an allergy test to prevent rashes and swelling.
Medicinal herbs
Decoctions based on medicinal herbs are a good basis for cold compresses. Water infusions can also be taken orally, but only after consulting a doctor.
For mastitis, a woman is recommended to:
- sage – suppresses lactation, has antibiotic properties;
- sweet clover - relieves spasms in the milk ducts, reduces pain;
- alder – has anti-inflammatory properties;
- mint – soothes, relieves pain;
- chamomile is a natural antiseptic, recommended for infectious mastitis.
Timely treatment of mastitis allows you to maintain the health and function of the mammary gland. And to prevent relapses, a woman should follow the rules of hygiene, put the baby to the breast as often as possible, follow the recommendations of specialists and not refuse therapy, and if necessary, surgical intervention.
Surgical treatment
The abscess form of mastitis is treated surgically. If there is one small formation, puncture aspiration of pus is possible. A thin needle is inserted into the capsule filled with secretion. The process is monitored using an ultrasound machine. Using a needle, the capsule is emptied and an antibiotic is injected into it to stop the inflammation.
For multiple and large abscesses, surgery is recommended. It is performed in a hospital under local or general anesthesia - depending on the patient’s condition and the stage of the disease. The surgeon makes a longitudinal incision from the nipple to the base of the breast, less often a horizontal one, passing under the mammary gland. The doctor removes capsules with pus and damaged tissue, connects multiple formations and washes the wound with an antiseptic solution. A drainage is inserted into the cavity, which will remove the purulent contents. It is left for 3-4 days. If the inflammation decreases, the drainage is removed and the hole left behind is sutured.
After the operation, the woman is prescribed infusion therapy - cleansing the body of toxins with special solutions. The patient is also prescribed antibiotics, non-steroidal anti-inflammatory drugs and immunomodulators.