Pyelonephritis
Diabetes
Hepatitis
Rheumatism
17303 October 27
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. We remind you that independent interpretation of the results is unacceptable; the information below is for reference only.
Urea in the blood: indications for prescription, rules for preparing for the test, interpretation of the results and normal indicators.
Blood urea level (table)
The level of urea in the blood is a relatively unstable indicator, unlike other nitrogenous compounds (for example, creatinine), since it is more dependent on nutrition.
| Age | Urea level in blood, mmol/l |
| Newborns | 1,4-4,3 |
| Children under 14 years old | 1,8-6,4 |
| Adults from 14 to 60 years old | 3,5-8,3 |
| Adults over 60 years old | 2,9-7,5 |
For comparison: the normal level of urea in urine is 330-580 mmol/l.
The danger of high levels of urea (azothermia) lies not in the increase in blood levels itself, but in the possible disruption of the chemical processes of protein breakdown or malfunctions of the excretory system (kidneys, gall bladder and bile ducts).
In order for the analysis indicators to correspond to the real state of urea in the blood, it is necessary to adhere to certain rules before the procedure, namely:
- take the test in the morning on an empty stomach;
- do not eat 10-12 hours before the procedure;
- on the day before the analysis, do not consume excessive amounts of protein foods and sports nutritional supplements;
- Avoid physical activity on the eve of the procedure.
In what cases does a deviation from the norm not indicate pathology?
According to the rules, any test must be taken in the morning on an empty stomach , biochemistry is no exception. There are times when urea is elevated, but there is no cause for concern. For example:
- Strong and frequent physical activity.
- Constant stress.
- Abuse of protein foods or fasting.
- Taking certain medications (Corticosteroids, anabolics, etc.).
To identify pathology, it is necessary to donate blood from a vein.
In order for the urea indicator to be accurate, a number of rules must be followed:
- Do not overload the body 24 hours before the examination.
- The day before the test, give up meat, fish and sweets.
- In the morning it is better not to drink or eat anything.
- Avoid stress.
Causes of increased urea in the blood
If urea in the blood exceeds normal levels, then there are production and retention reasons for the increase in levels.
Productive causes of high urea content in the blood are the result of pathological processes associated with an increase in the rate and excess amount of protein breakdown in the body. As a rule, such processes occur in the following diseases:
- fever;
- acute hemolytic anemia;
- hemolytic jaundice;
- hypoparathyroidism;
- leukemia,
- cachexia (muscle atrophy due to prolonged fasting or illness);
- purulent processes (abscess, gangrene);
- surgical interventions;
- poisoning with chemicals (mercury, phenol, chloroform);
- therapy with glucocorticosteroids (hypocortisone, prednisolone, fludrocortisone, dexamethasone);
- taking androgens - male sex hormones (bicalutamide, nilutamide, gestrinone, testosterone, flutamide, etc.).
Among the reasons for the increase in urea content in the blood is the accumulation (retention) of metabolic products in the body. A retention increase is observed if urea in the blood is increased due to disruption of the excretory system:
- disorders of the kidneys (glomerulonephritis, pyelonephritis, amyloidosis, renal tuberculosis);
- impaired urine output (stones and tumors in the urinary tract, prostate adenoma);
- circulatory disorder when blood flows poorly to the kidneys (internal and external bleeding, burns, hypertensive or coronary heart disease, intestinal obstruction).
Symptoms
A high concentration of urea in the blood is most often manifested by symptoms from the excretory system, namely:
- severe pain in the lower back;
- acute pain in the lower abdomen;
- rare or frequent urination;
- blood in the urine and pain when urinating;
- presence of edema;
- increased blood pressure;
- weakness and fatigue.
Consequences
Lack of drug treatment for elevated urea levels can lead to acute or chronic renal failure. In this case, the urea content can reach 100-200 mmol/liter with a norm of 1.4-8.3 mmol/l.
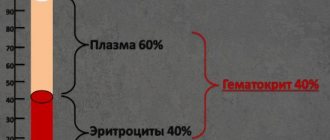
The development of renal failure leads to an increase in urea and other chemical metabolic products in the blood, since there is no filtration of blood plasma by the kidneys. In this case, associated complications are observed, namely:
- arterial hypertension (persistent increase in blood pressure);
- proteinuria (protein in urine);
- hyperelipidemia (increased levels of lipids in the blood);
- hyperparathyroidism (overactive parathyroid gland);
- problems with blood clotting;
- electrolyte imbalance.
What indicators should we use to consider urea?
If the biochemical test results show high urea levels, the doctor will first look for other characteristics that can provide information about the health of the kidneys, liver and muscles. Considering them together, it is possible to determine the causes of violations and the degree of their danger to the patient’s health.
Bilirubin
This is the name of the pigment that is produced by the liver and concentrated in bile. In large quantities, it enters the bloodstream in case of obstruction of the bile ducts and various diseases of the gland. The substance is also released when red blood cells (erythrocytes) break down.
If bilirubin and urea are elevated, liver disease (cirrhosis, hepatitis) can be suspected. However, you still need to pay attention to transaminase indicators (ALT, AST). With liver pathologies, the levels of these compounds also increase, and based on their ratio, the doctor can guess the essence of the changes in the gland.
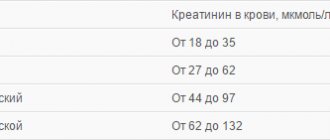
Creatinine
It is also a product of protein metabolism, which is predominantly produced by muscle tissue. Its concentration is influenced by gender, body weight, diet and lifestyle.
High creatinine levels are traditionally considered an indicator of a meat-based diet. Often the concentration of this substance increases in athletes, bodybuilders, against the background of heavy strength loads and intensive consumption of protein substances. The compound is excreted by the kidneys, and therefore is considered a marker of their work. If urea and creatinine are significantly elevated, glomerular filtration disorders may be suspected.
Blood proteins
Indicators of protein compounds in blood serum provide information about the state of metabolism. The level can increase in many diseases, but more often it indicates massive tissue destruction. C-reactive protein detects inflammation in the body.
There is a special polypeptide that in modern medicine is considered a reliable marker of kidney function - cystatin C. If its content in plasma increases, they speak of the development of renal failure.
Uric acid
Urea and uric acid levels are often confused. However, these are completely different substances that reflect different metabolic processes. The acid is formed as a result of purine metabolism - the transformation of purine bases in the body. Their sources are meat products (broths, fatty meats), legumes. Disorders of purine metabolism lead to the accumulation of uric acid in the body and an increased risk of deposition of its salts in tissues. The most well-known disorder on this basis is called gout.
How to lower blood urea levels
To reduce the concentration of urea, it is necessary to use a whole range of measures:
- drug therapy;
- therapeutic diet;
- no intense load on the muscular system.
The use of medications for high urea is prescribed depending on the cause that caused the high level of nitrogenous substances in the blood.
In order to prevent urea from accumulating in the body, first of all, it is necessary to normalize the functioning of the excretory system (kidneys and biliary tract), heart and strengthen the vessels of the circulatory system with the help of:
- diuretics are medications that promote increased urination, during which urea is intensively removed from the body (spinorolactone, furosemide);
- beta-blockers - drugs that normalize blood pressure, since high blood pressure often occurs when kidney function is impaired (atenolol, timolol, metoprolol, etc.);
- ACE inhibitors are drugs used to treat heart and kidney failure. ACE inhibitors normalize pressure, including in the capillaries of the kidneys, thereby improving blood filtration by the excretory organs (captopril, quinapril, lisinopril, etc.).
What is urea
The natural metabolism of protein structures produces nitrogen-containing amino acids, which include ammonia, a chemical whose elevated levels are highly toxic to the human body. Under normal conditions, it, like other elements, undergoes filtration by the liver with further conversion into urea - the end product of metabolism. The substance is excreted along with urine, through processing by the kidneys.
A deviation from the normal value indicates renal dysfunction, which may indicate the presence of serious diseases. Without timely treatment, increased concentrations can lead to dangerous complications, including the development of gout.
Diet
Elevated urea in the blood can be normalized after nutritional correction: animal proteins that promote the active formation of urea are excluded from the diet.
In order to lower the level of urea, a therapeutic diet of table 7 is used, which is gentle on the organs of the excretory system.
The basic principles of a therapeutic diet to reduce urea levels are as follows:
- eat 4-5 times a day in small portions to avoid stress on the liver and kidneys;
- drink plenty of fluids (1.5-2 liters per day);
- completely eliminate protein of animal origin (meat, sausages, by-products and dishes made from them, canned meat and fish, smoked meats, meat and fish broths);
- exclude chocolate and cocoa, strong tea and coffee, baked goods, alcoholic drinks;
- limit the consumption of fermented milk products (low-fat cheese, cottage cheese, sour cream, yogurt) and eggs (up to 2 per week);
- You can consume vegetable oil, butter and biscuits on a limited basis.
The diet should consist of complex carbohydrates, the digestion of which does not release ammonia and does not produce increased urea, namely:
- cereals (buckwheat, oatmeal, rice, wheat, etc.);
- fresh and thermally processed vegetables (carrots, onions, zucchini, cabbage, potatoes);
- fruits and berries, nuts, dried fruits.
Diagnostics
To determine the most correct treatment method, a number of necessary diagnostic studies are carried out, which makes it possible to detect additional features of the patient’s body. Biochemical analysis is the main diagnostic method if elevated urea levels are suspected. To study the functioning of internal organs, ultrasound of the liver and kidneys, as well as intravenous urography, can be prescribed.
Methodology
The diagnostic method of testing serum for urea concentration is carried out in several ways, which are conventionally divided into the following groups:
- gasometric;
- enzymatic;
- photometric.
The main purpose of biochemical analysis is to assess the functionality of the kidneys and liver, as well as to determine the amount of nitrogenous elements in the body.
For the purpose of prevention, it is recommended to undergo a comprehensive study of the biochemistry of blood and urine at least 2 times a year, regardless of the indications. Along with the analysis, additional methods are prescribed to determine the amount of creatinine, protein and other important elements.
Preparation
In order for the test results to be as accurate as possible, the patient must adhere to certain recommendations. General tips when conducting biochemical and microbiological tests include:
- Exclusion from the diet of the following foods for 2 days before the start of the analysis: fish, meat, liver, coffee, tea, alcohol;
- No heavy physical activity for 3 days before;
- Refusal to take medications, alcohol and smoking for 8 hours;
- Avoiding stressful situations.
It is advisable to come to the study 10-15 minutes earlier to restore calm breathing, since this factor also affects the results. A serum sample is collected on an empty stomach from the ulnar or radial vein, or in rare cases from the wrist or foot.
Treatment with folk remedies
The action of many medicinal herbs used in traditional medicine recipes to reduce urea is aimed at normalizing the condition of the kidneys and removing metabolic chemical compounds from the body.
Bearberry
. Bearberry leaves contain flavonoids, organic acids and arbutin. It is arbutin that has a beneficial effect on the kidneys, relieves inflammation, and has a diuretic effect, which helps reduce urea in the blood and eliminate metabolic products in the urine.
To prepare the infusion, you will need to pour 2 tablespoons of crushed dry bearberry leaves with boiling water and heat the medicine in a water bath for 20 minutes. After cooling, the infusion is filtered and taken 3 tbsp. 4-5 times a day before each meal. The course of treatment is three weeks.
Liquorice root
. The healing plant is used for various diseases, including problems with the excretory system. Licorice root contains glycyrrhizic acid, which relieves inflammation, and flavonoids, which relax the smooth muscles of the kidneys, resulting in urea being actively eliminated from the body.
Preparation: 1.5 tablespoons of crushed licorice root must be brought to a boil in 500 grams of water and simmered over low heat for 10 minutes. Next, the broth is filtered and taken half a glass three times a day after meals for 20 days.
Drug treatment regimen
An increase in blood urea levels greater than 10 mmol requires medication. This is extremely necessary, since the body cannot cope with the problem on its own, even with nutritional adjustments. Independent choice of a regimen for how to treat the disease is strictly prohibited, since an uncontrolled decrease in the level of the substance by drugs leads to serious complications.
An effective drug is Probenecid, which copes well with removing the substance, but interacts poorly with other drugs. Interaction with drugs of various groups affects the renal system, in which the active substances of any medications are retained.
Taking this drug is not recommended during acute periods of gout attacks, since the patient experiences a strong deterioration in the condition. An absolute contraindication for use in women during pregnancy and breastfeeding, as well as in children under 2 years of age.
A safer alternative is Allopurinol, which dissolves urates and removes urea. Even infants can take this drug. The course of treatment is determined by the treating specialist, who monitors the effectiveness of therapy through regular testing. The drug is discontinued when the level of urea in the blood plasma normalizes. Taking all medications is accompanied by strict adherence to the recommended diet.
Prevention
To avoid an increase in urea in the blood, you need to carefully monitor your diet, give up bad habits, and also adhere to the following recommendations:
- do not use nephrotoxic drugs (many medications inhibit kidney function, for example, non-steroidal anti-inflammatory drugs, iron supplements, etc., after discontinuation of which urea in the blood normalizes);
- avoid using high-protein diets for weight loss (Atkins, Dukan, Kremlin diet, etc.);
- combine a low-calorie diet with drinking alcoholic beverages;
- engage in feasible physical activity, but avoid exhausting sports.