How are lymphocytes formed?
The main organs that form lymphocytes are the thymus (before puberty) and the bone marrow. In them, cells divide and remain until they encounter a foreign agent (virus, bacteria, etc.). There are also secondary lymphoid organs: lymph nodes, spleen and formations in the digestive tract. This is where most lymphocytes migrate. The spleen is also the depot and place of their death.
There are several types of lymphocytes: T, B and NK cells. But they are all formed from a single precursor: a stem cell. It undergoes changes, eventually differentiating into the desired type of lymphocyte.
Why are lymphocytes necessary?
B-lymphocytes, when in contact with foreign proteins, secrete protective immunoglobulins. They provide long-term, and often lifelong, immunity to diseases, including after vaccination.- T-lymphocytes destroy intracellular parasites, virus-infected cells, and are also responsible for the intensity of the immune response.
- NK lymphocytes attack cancer cells.
Functions
The main function of lymphocytes, regardless of their type, is the formation of the body's immune system . These cells destroy viruses and bacteria, as well as any foreign bodies.
Each type of lymphocyte performs its own functions . For the immune system to function fully, all types of these cells are necessary. If at least one of the types begins to form incorrectly, then this factor negatively affects the body’s performance of protective functions.
General functions of lymphocytes:
- destruction of infections entering the body;
- recognition of agents foreign to the body;
- preventing the development of pathological formations;
- implementation of immune memory;
- destruction of cells with cancerous elements;
- participation in the elimination of inflammatory processes;
- preventing pathogenic microorganisms from entering the body;
- destruction of mutated cells;
- participation in the process of tissue regeneration after damage;
- production of specific antibodies;
- formation of immunity to a previous infectious disease;
- identification and binding of antigens;
- formation of the body's immune barrier;
- production of enzymes that break down viruses and bacteria of various types;
- destruction of body cells that are infected with any infections.
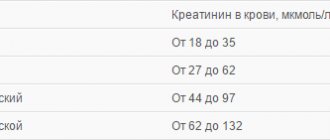
How to determine the number of lymphocytes?
The number of lymphocytes is reflected in the general blood test. Previously, all cell counts were carried out manually using a microscope. Nowadays, automatic analyzers are more often used to determine the number of all blood cells, their shape, degree of maturity and other parameters. The standards for these indicators for manual and automatic determination differ. Therefore, confusion still often arises if the analyzer results are close to manual standards.
In addition, the forms sometimes do not indicate the rate of lymphocytes in the child’s blood. Therefore, it is necessary to clarify the standards for each age group.
How the analysis is carried out:
For the patient, everything is extremely simple: he just needs to come to the treatment room on an empty stomach and donate blood. A few drops of blood from a finger are enough for the study, but in some cases, in order to determine the increase or decrease in lymphocytes, patients have to sacrifice the integrity of the vein. The source of blood depends on how the test is performed.
If the test is done the “old fashioned way”, using a microscope to count cells, then blood will be taken from a finger. However, most laboratories now use automatic cytometer counters. The most “advanced” of these devices can count the number of lymphocytes, erythrocytes and other cells simultaneously in 10-50 samples in a short time! This is an excellent saving of time and labor for laboratory technicians, so such counters are quite popular and are available in most clinics. Unfortunately, they have one “trouble”: they are effective only if the blood sample is submitted for analysis in a volume of more than 5 ml. If it is less, then the device will not be able to determine whether the patient has high or low lymphocytes.
Norms of lymphocytes in the blood
| Relative values of lymphocytes: | Absolute values of lymphocytes: |
|
|
What do elevated lymphocytes in the blood mean?
Lymphocytosis is an increase in the number of lymphocytes. It can be relative and absolute
- Absolute lymphocytosis is a condition in which the number of lymphocytes exceeds age norms. That is, in adults there are more than 4 * 109 cells per liter.
- Relative lymphocytosis is a change in the percentage of white cells in favor of lymphocytes. This happens when the total number of leukocytes decreases due to the neutrophil group. As a result, the percentage of lymphocytes becomes larger, although their absolute value remains normal. A similar blood picture is considered not as lymphocytosis, but as leukopenia with neutropenia.
It is important to remember that if neutrophils are reduced and lymphocytes are increased only as a percentage, this may not reflect the true picture. Therefore, most often in blood tests they focus specifically on the absolute number of lymphocytes (in cells per liter).
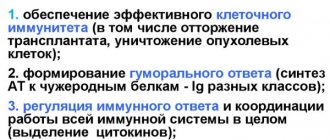
Basic properties and functions, types of lymphocytes
Lymphocytes (LYM) are rightly called the main figure of the human immune system. They, maintaining the genetic constancy of homeostasis (internal environment), are able to recognize “theirs” and “theirs” by the signs known to them. In the human body they solve a number of important tasks:
- Antibodies are synthesized.
- They lyse foreign cells.
- They play a major role in transplant rejection, although this role can hardly be called positive.
- Provides immune memory.
- They are engaged in the destruction of their own defective mutant cells.
- They provide sensitization (increased sensitivity, which is also not very beneficial for the body).
To make this entire immune process more clear to the reader, let us consider in more detail which of the lymphocytes are, what they do, and what these cells are called in connection with their functions.
The lymphocyte community has two populations: T cells, which provide cellular immunity, and B cells, which are entrusted with the function of providing humoral immunity; they implement the immune response through the synthesis of immunoglobulins. Each population is divided into varieties depending on its purpose. All T lymphocytes within a species are morphologically uniform, but differ in the properties of surface receptors.
The T cell population includes:
- T-helpers (helpers) - they are omnipresent.
- T-suppressors (suppress the reaction).
- T-killers (killer lymphocytes).
- T-effectors (accelerators, amplifiers).
- Immunological memory cells from T-lymphocytes, if the process ended at the level of cellular immunity.
The following types are distinguished in the B-population:
- Plasma cells that enter the peripheral blood only in extreme situations (irritation of lymphoid tissue).
- B-killers.
- B-helpers.
- B-suppressors.
- Memory cells from B-lymphocytes, if the process has passed the stage of antibody formation.
In addition, in parallel there is an interesting population of lymphocytes, which are called zero (neither T nor B). It is believed that they turn into T- or B-lymphocytes and become natural killers (NK, N-killers). These cells are produced by proteins that have the unique ability to “drill” pores located in the membranes of “enemy” cells, for which NKs were called perforins
.
Natural killer cells, meanwhile, should not be confused with killer T cells; they have different markers (receptors). NKs, unlike T-killers, recognize and destroy foreign proteins without developing a specific immune reaction.
Causes of elevated lymphocytes in the blood
- Stress and hormonal fluctuations
- Long term smoking
- Infections Viral (respiratory viruses, infectious mononucleosis, chicken pox, measles)
- Bacterial (tuberculosis, syphilis, whooping cough, cat scratch disease)
- Parasitic (toxoplasmosis)
- Chronic lymphocytic leukemia
- Acute lymphoblastic leukemia
- Autoimmune processes (thyrotoxicosis)
- Lead, arsenic, carbon disulfide poisoning
- Taking certain medications (levodopa, phenytoin, valproic acid, narcotic and non-narcotic analgesics)
- Splenectomy
Infectious diseases
The entry of an infectious agent into the body leads to the activation of all protective forces. During bacterial infections, a large number of neutrophils are produced that destroy microbes. And when viruses penetrate, lymphocytes come into play. They mark cells affected by viral particles, produce antibodies against them and then destroy them.
Therefore, with almost any viral infection, relative lymphocytosis occurs, and often absolute lymphocytosis. This indicates the beginning of the formation of immunity to the disease. The elevated level of lymphocytes remains throughout the entire recovery period and sometimes a little longer. Blood tests are especially affected by infectious mononucleosis. Some chronic bacterial infections also cause an increase in lymphocytes (tuberculosis and syphilis, for example).
Mononucleosis
This is an infection caused by the Epstein-Barr virus. This virus affects almost all people sooner or later. But only in some people does it lead to symptoms collectively called infectious mononucleosis. The virus is transmitted through saliva during close household contacts, as well as through kissing. The latent period of the disease can last more than a month. The main target of viral particles is lymphocytes. Symptoms of the disease:
- temperature increase
- a sore throat
- enlarged lymph nodes
- weakness
- night sweats
The disease is more easily tolerated by young children. Teenagers and adults may feel the signs of infection much more strongly. To diagnose mononucleosis, complaints, examination and test analysis are usually sufficient: lymphocytes in the child’s blood are elevated, abnormal mononuclear cells are present. Sometimes an immunoglobulin test is used. Treatment for a viral infection is usually symptomatic. Requires rest, drinking enough fluids, and for fever, antipyretic drugs (paracetamol, ibuprofen). In addition, it is better to avoid playing sports during illness. Mononucleosis causes an enlargement of the spleen, which processes blood cells. This increase, combined with trauma, can lead to organ rupture, bleeding, and even death.
Whooping cough
This is a severe infectious disease of the respiratory tract. It most often affects children, although high vaccination coverage in recent years has sharply reduced the incidence of infection.
Whooping cough begins as a typical cold, but after 1-2 weeks a paroxysmal cough occurs. Each attack can end in severe vomiting. After 3-4 weeks, the cough becomes calmer, but persists for a long time. Previously, whooping cough was a common cause of death and disability in children. But even now children are at risk of cerebral hemorrhage and convulsive syndrome during an attack.
The diagnosis is made based on symptoms, PCR and enzyme immunoassay results. In this case, in a general blood test, significant leukocytosis almost always occurs (15-50 * 109), mainly due to an increase in the number of lymphocytes.
Antibiotics are used to treat whooping cough. However, they rarely shorten the duration of the disease, but can reduce the incidence of complications. The main protection against this serious illness is vaccination with DTP, Pentaxim or Infanrix.
Treatment and prevention
Treatment of lymphocytosis involves eradicating the root cause, that is, the disease that formed the basis of the inflammation. There is no need to treat an increased white blood cell count as a symptom.
If lymphocytes have increased due to infectious pathologies and pathogens, the best solution would be to provide the body with the conditions to independently fight the virus. It is important for the body to get plenty of rest, healthy and proper nutrition, and good sleep. Over time, the level of cells will decrease to normal, but this will not happen instantly, sometimes it will take a period of up to a couple of weeks.
Leukemia, lymphoma or myeloma are treated differently. The body is not able to restore balance, so for recovery it is important to go to the doctor to select the right and effective treatment and therapy. Otherwise, the situation can be fatal. All necessary tests and therapy are prescribed by the doctor. Treatment is accompanied by chemotherapy, radiotherapy, and bone marrow transplantation.
Infections with severe pathogens, for example, AIDS, require long-term therapy and a course of antibiotics.
Traditional methods
The methods mentioned can only be used after consultation and permission from a doctor! Otherwise, it is important to refrain from folk remedies and rely on medications.
A patient can increase the level of lymphocytes in the blood with tinctures of herbs: barley, sweet clover, rose hips, pollen. The presence of animal products in the diet is important, especially dairy, nuts, dried fruits, beets, pomegranates and honey. Adding a little physical activity will have a positive effect on the patient's well-being. Among medications, the patient can take drugs that play a positive role in increasing the duration of white cell activity, for example, Lenograstim.
To reduce the content of white blood cells, the patient is able to drink a course of herbs: horsetail, linden, sloe berries, lingonberry and strawberry leaves, birch and propolis. In nutrition, it is important to focus on eating fresh vegetables and seafood, buckwheat and dried fruits. It is important to avoid fried, fatty, smoked and salty foods. Limit food to small portions, drink at least two liters of water per day. It is important to add regular physical activity and healthy sleep. Inclusion of antibiotics, antihistamines, antiviral drugs.
Prevention
To prevent an increase or decrease in the content of lymphocytes, it is important to donate blood for a blood test once a year. This is important for monitoring the condition of the body and preventing inflammation in the early stages.
Preventive measures to strengthen the immune system, for example, maintaining a healthy lifestyle, more physical activity, giving up bad habits, will play an important role in preventing an increase or decrease in the number of lymphocytes.
It is important to treat all chronic and acute pathologies on time to avoid complications. The main thing to remember is that an increase in the level of blood cells is not an independent pathology, it is a symptom of an inflammatory process occurring in the body.
Increased or decreased lymphocytes in the blood are a clear sign of problems in the body. This indicates pathologies that are most likely to lead to death if complications occur. You are supposed to treat your own health with care and respect, and regularly visit doctors for the purpose of prevention and timely treatment of diseases! By following the rules, a person will not experience an increase or decrease in the level of cells in the blood and will be healthy.
Blood tumors
Unfortunately, lymphocytosis is not always reactive in response to infection. Sometimes it is caused by a malignant process that causes cells to divide uncontrollably.
Acute lymphoblastic leukemia (ALL)
A tumor disease of the blood in which immature lymphoblasts are formed in the bone marrow that have lost the ability to turn into lymphocytes is called ALL. Such mutated cells cannot protect the body from infections. They divide uncontrollably and inhibit the growth of all other blood cells.
ALL is the most common type of blood tumors in children (85% of all childhood hemoblastoses). It is less common in adults. Risk factors for the disease include genetic abnormalities (Down syndrome, for example), radiation therapy and intense ionizing radiation. There is information about the effect of pesticides in the first three years of a child’s life on the risk of developing ALL.
Signs of ALL:
- Symptoms of anemia: pallor, weakness, shortness of breath
- Symptoms of thrombocytopenia: unreasonable bruises and nosebleeds
- Symptoms of neutropenia: fever, frequent severe infectious diseases, sepsis
- Enlarged lymph nodes and spleen
- Bone pain
- Neoplasms in the testicles, ovaries, mediastinal area (thymus)
To diagnose acute lymphoblastic leukemia, a complete blood count is required. It most often has a reduced number of platelets and red blood cells. The white blood cell count may be normal, low, or high. At the same time, the level of neutrophils is reduced, and the level of lymphocytes is relatively increased, often there are lymphoblasts. If there is any suspicion of a tumor, a bone marrow puncture is performed, with the help of which a final diagnosis is made. The criterion for a tumor is a large number of blasts in the bone marrow (more than 20%). Additionally, cytochemical and immunological studies are carried out.
Treatment of ALL
The main principles of treatment of blood tumors are the introduction of remission, its consolidation and maintenance therapy. This is achieved with the help of cytostatic drugs. Chemotherapy is difficult for many, but it is the only treatment that gives a chance for recovery. If the disease does return (relapse), then more aggressive cytostatic therapy regimens are used or a bone marrow transplant is performed. Bone marrow transplantation is performed from a relative (if suitable) or from another suitable donor.
Prognosis for ALL
Advances in oncohematology make it possible to cure a large number of patients with acute lymphoblastic leukemia. Factors for a positive prognosis include young age, a leukocyte count of less than 30,000, the absence of genetic damage, and the introduction of remission within 4 weeks of treatment. In this situation, more than 75% of patients survive. Each relapse of the disease reduces the chances of a full recovery. If there have been no relapses for 5 years or more, the disease is considered defeated.
Chronic lymphocytic leukemia (CLL)
A blood tumor in which the level of mature lymphocytes in the bone marrow increases is called CLL. Although tumor cells differentiate into their final forms, they are unable to perform the functions of lymphocytes. While ALL most often affects children and young adults, CLL usually occurs after age 60 and is a not-so-rare cause of elevated lymphocytes in the blood of an adult. This type of leukemia is the only one for which risk factors have not been established.
Symptoms of CLL:
- Enlarged lymph nodes (painless, mobile, dense)
- Weakness, pallor
- Frequent infections
- Increased bleeding
- If the condition worsens: fever, night sweats, weight loss, enlarged liver and spleen
Quite often, CLL is an incidental finding during a routine blood test, since this disease is asymptomatic for a long time. Results are considered suspicious if the number of leukocytes exceeds 20*109/l in adults, and the number of platelets and red blood cells is sharply reduced.
A feature of the treatment of CLL is its resistance to chemotherapy. Therefore, therapy is often delayed until obvious symptoms appear. In this condition, a person can live without treatment for several years. If the condition worsens (or leukocytes double in six months), cytostatics can slightly increase life expectancy, but more often they do not affect it.
Additional examinations
Among the auxiliary diagnostic methods, in addition to the standard general blood test, are:
- Biochemistry.
- Chest X-ray.
- MRI or CT. If there are suspicions of lung function disorders or oncological processes.
- Ultrasound of the abdominal organs.
- Thyroid examination.
- Hormone tests.
Everything else can be prescribed at the discretion of the treating specialist.
The functions of lymphocytes are to protect the body from harmful external influences and provide lifelong immunity from certain diseases. All deviations are interpreted as pathology, a sign of a disorder.
Thyrotoxicosis
One of the important functions of lymphocytes is the formation of delayed allergic reactions. That is why an increase in such cells may indicate an autoimmune process. A striking example is diffuse toxic goiter (Graves-Bazedow disease). For unknown reasons, the body begins to attack its own receptor cells, as a result of which the thyroid gland is in constant activity. Such patients are fussy, restless, and find it difficult to concentrate. There are often complaints of interruptions in heart function, shortness of breath, fever, and hand tremors. The eyes of patients with toxic goiter are wide open and sometimes seem to be coming out of their sockets.
The main laboratory sign of DTG is high values of the hormones T3 and T4 with low TSH. There is often relative and sometimes absolute lymphocytosis in the blood. The reason for the increase in lymphocytes is the excessive activity of the immune system.
Treatment of thyrotoxicosis is carried out with thyreostatics, followed by surgery or radioactive iodine therapy.
Other autoimmune diseases (rheumatoid arthritis, Crohn's disease, etc.) are also combined with lymphocytosis.
Indications for analysis
Lymphocyte analysis is carried out as part of a clinical (general) blood test with a leukocyte formula. It is prescribed for the diagnosis of the following pathologies:
- general inflammatory processes in acute and chronic form;
- autoimmune diseases;
- infectious, viral or fungal infections;
- suppuration and sepsis;
- internal bleeding;
- oncology;
- allergic reaction;
- pathological course of pregnancy;
- diseases of the hematopoietic and circulatory system;
- pathologies of the lymphatic system;
- radiation sickness;
- typhus;
- monitoring the effectiveness of treatment.
Diseases of bone marrow with its depletion
Some diseases cause pancytopenia - the depletion of all blood cells in the bone marrow. In such cases, not only the number of lymphocytes is reduced, but also other types of leukocytes, red blood cells and platelets.
Fanconi anemia
Congenital Fanconi anemia is named after its most striking syndrome: anemic. But the basis of the disease is depletion of the bone marrow and inhibition of all hematopoiesis. In the analysis of patients, a decrease in the number of red blood cells, platelets and all types of white cells (including lymphocytes) is observed. Congenital pancytopenia is often accompanied by developmental anomalies (absence of thumbs, short stature, hearing loss). The main danger and the main cause of death is a decrease in the number of neutrophils and platelets, resulting in severe infections and massive bleeding. In addition, such patients have an increased risk of cancer.
Treatment of congenital pancytopenia is carried out with hormonal agents. They can delay complications for some time. The only chance for a complete cure is a bone marrow transplant. But due to frequent cancer diseases, the average life expectancy of such people is 30 years.
Exposure to radiation
Exposure to various types of radiation (accidental or for treatment purposes) can lead to bone marrow dysfunction. As a result, it is replaced by connective tissue, and the supply of cells in it becomes poor. In blood tests in such cases, all indicators decrease: red blood cells, white blood cells and platelets. Lymphocytes are also usually low.
Danger of Low Lymphocyte Count
A recent study by American scientists from the Cleveland Clinic and Cleveland University Hospital showed that there is a clear and consistent relationship between lymphocyte levels and mortality. () An increase in the risk of mortality was observed already at 2,000 lymphocytes/μl, at 1,500 cells/μl this risk increased by 50%, and with a lymphocyte count of less than 1,000, the risk increased by 3.9 times.
lymphocytopenia was found from heart disease, cancer, and respiratory infections (eg, influenza and pneumonia). a particularly negative effect on mortality while increasing red blood cell distribution width (RDW) and the amount of inflammatory C-reactive protein in the blood.
People with low lymphocyte counts, elevated inflammatory C-reactive protein and a red blood cell disorder (RDW) live about 10 years less than people with the same lifestyle but without these disorders. ()
SCHEME OF AN IMMUNE RESPONSE TO A PATHOGEN WITH THE PARTICIPATION OF DIFFERENT TYPES OF LYMPHOCYTES AND THE POSSIBILITY OF ITS REGULATION
Hodgkin's lymphoma (lymphogranulomatosis)
The main difference between lymphoma and lymphocytic leukemia is the initial site of its occurrence. Tumor cells in lymphomas are located locally, most often in the lymph nodes. In leukemia, the same malignant cells are formed in the bone marrow and are immediately carried into the general bloodstream.
Symptoms of Hodgkin's lymphoma:
- Enlargement of one or more lymph nodes
- Anemia, increased bleeding and susceptibility to infections (if the process is advanced)
- Intoxication (fever, night sweats, weight loss)
- Symptoms of compression of organs by a tumor: suffocation, vomiting, irregular heartbeat, pain
The main diagnostic method is a biopsy of the affected lymph node or organ. In this case, a piece of tissue is sent for histological examination, based on the results of which a diagnosis is made. To determine the stage of the disease, a bone marrow puncture is taken and a computed tomography scan of the main groups of lymph nodes is performed. Blood tests may be normal in the early stages of lymphoma. Deviations, including lymphopenia, occur as the disease progresses.
Treatment of the disease is carried out with cytostatic drugs followed by irradiation of the lymph nodes. For relapses, more aggressive chemotherapy and bone marrow transplantation are used.
The prognosis for such a tumor is usually favorable, with a 5-year survival rate of 85% or higher. There are several factors that worsen the prognosis: age over 45 years, stage 4, lymphopenia less than 0.6 * 109.
Immunodeficiencies
Immune deficiency is divided into congenital and acquired. In both cases, the level of lymphocytes in the general blood test may change due to a deficiency of T cells. If the B-link is affected, then a routine blood test often does not reveal abnormalities, so additional research methods are required.
DiGeorge syndrome
This variant of immunodeficiency is also called hypoplasia (underdevelopment) of the thymus. The chromosome defect in this syndrome also causes heart defects, facial abnormalities, cleft palate, and low blood calcium levels.
If a child has an incomplete syndrome, when part of the thymus is still preserved, then he may not suffer too much from this disease. The main symptom is a slightly higher frequency of infectious lesions and a slight decrease in lymphocytes in the blood.
The full syndrome is much more dangerous, manifests itself with severe viral and fungal infections in very early childhood, and therefore requires a thymus or bone marrow transplant for treatment.
Severe combined immunodeficiency (SCID)
Mutations of certain genes can lead to severe damage to cellular and humoral immunity - SCID (severe combined immunodeficiency). The disease manifests itself already in the first months after birth. Diarrhea, pneumonia, skin and ear infections, sepsis are the main manifestations of the disease. The causative agents of fatal diseases are microorganisms that are harmless to most people (adenovirus, CMV, Epstein-Barr, herpes zoster).
A general blood test reveals an extremely low content of lymphocytes (less than 2 * 109 cells per liter), the thymus and lymph nodes are extremely small.
The only possible treatment for SCID is a donor bone marrow transplant. If it is carried out in the first three months of the baby’s life, then there is a chance of a complete cure. Without therapy, children with combined immunodeficiency do not survive beyond 2 years of age. Therefore, if a child has low lymphocytes in his blood and is constantly suffering from severe infectious diseases, then it is urgently necessary to conduct additional examination and begin treatment.
AIDS
Acquired immunodeficiency syndrome is associated with the damaging effects of HIV on T lymphocytes. Penetration of this virus is possible through biological fluids: mainly blood and sperm, as well as from mother to child. A significant decrease in lymphocytes does not occur immediately. Sometimes several years pass between infection and the onset of AIDS. As the disease progresses and lymphopenia increases, a person loses the ability to resist infections, which can lead to sepsis and death. The risk of tumors increases for the same reason: the disappearance of T cells. Treatment of HIV infection with special antiretroviral drugs helps control the disease, maintains the necessary level of immunity and prolongs life.
Abnormal lymphocyte levels in various diseases
The body conditions we discuss in this article are usually associated with abnormal lymphocyte levels, but this symptom alone is not enough to make a diagnosis. Work with your doctor to determine exactly what underlying condition may be causing your lymphocyte count to be unusually high or low.
Lymphoma
Lymphoma can be the result of uncontrolled growth of lymphocytes in the body. Mutations in genes or disturbances in molecular pathways involved in tumor suppression can cause uncontrolled growth of B and T cells. ()
B-lymphocyte hyperactivity, associated with autoimmune diseases and impaired T-cell function, can also lead to the development of lymphoma. ()
HIV AIDS
A feature of HIV/AIDS is a decrease in the number and functions of CD4+ T-lymphocytes in the body. Most HIV-infected cells are also resistant (indifferent) to natural killer cells. ()
In studies conducted in HIV-infected patients, CD4+ T cells were most depleted in the intestine. () The HIV virus, when infected, causes dysfunction and death of CD4+ T lymphocytes.
HIV also causes T-cell apoptosis (programmed cell death), which leads to a weakened immune system and an inability to fight infections. ()
Multiple sclerosis
Patients with multiple sclerosis have higher numbers of T cells. CD4+, CD8+, Th17 lymphocytes and interferon-gamma play a major role in the formation of multiple sclerosis lesions in the brain. In addition, CD8+ T lymphocytes can initiate damage to the nervous system. ()
Type 1 diabetes
Cytotoxic T lymphocytes can destroy pancreatic cells that produce insulin, leading to increased blood glucose and the development of type 1 diabetes. In addition, with this disease, the interaction between Th17 and T-regulating lymphocytes is disrupted, with an increase in the number of Th17 in the lymph nodes. ()
Allergies and asthma
An imbalance of two types of immune cells – Th1 / Th2 (predominance of Th2) leads to the manifestation of asthma and allergies . Th2-type cytokines help support the inflammatory response in allergic diseases. ()
Dermatitis
Dermatitis is a chronic inflammatory skin disease. Th2 lymphocytes and their cytokines play an important role in the inflammatory response and may contribute to the development of dermatitis. ()
The information on this site has not been evaluated by any medical organization. We do not seek to diagnose or treat any disease. The information on the site is provided for educational purposes only. You should consult your physician before acting on information from this site, especially if you are pregnant, nursing, taking medications, or have any medical condition.
Rate this article
Average 3.9 Total votes (10)
Features of lymphocytosis in children
- Immediately after birth, neutrophils predominate among all leukocytes in children. But by the 10th day of life, the number of lymphocytes increases, occupying 60% of all white cells. This picture persists up to 5-7 years, after which the ratio of lymphocytes and neutrophils reaches adult norms. Therefore, lymphocytosis in young children is a normal physiological phenomenon if it is not accompanied by additional symptoms and changes in tests.
- The body of young children often responds to infections very violently, producing a leukemoid reaction. It got its name because of its resemblance to blood tumors - leukemia. With such a reaction, the number of leukocytes significantly exceeds the norm and even the level of normal inflammation. Sometimes immature forms (blasts) appear in the blood in an amount of 1-2%. Other hematopoietic germs (platelets, erythrocytes) remain within normal limits. Therefore, extremely high values of white blood (including lymphocytes) do not always mean cancer. Often the cause is common mononucleosis, chickenpox, measles or rubella.
The conclusion from the above is this: lymphocytes are extremely important cells in the human body. Their meaning can be a marker of very dangerous conditions, or it can indicate a common runny nose. The level of these cells should be assessed only in conjunction with other blood elements, taking into account complaints and symptoms. Therefore, it is better to entrust the assessment of the test results to your attending physician.
Author:
Evtushenko Anna Aleksandrovna obstetrician-gynecologist
Diagnostics
An increase in the level of white blood cells in the blood is quite difficult to detect: the symptoms do not relate to an increase, but to diseases of infectious, viral and bacterial types. First of all, it is important to go to a therapist or pediatrician. Doctors issue referrals for important urine and blood tests based on patient complaints. It is possible to prescribe tests for STDs, tuberculosis and hepatitis. Additional examinations may include ultrasound, CT, MRI, and x-rays.
In difficult cases, doctors have the right to take a second blood collection for double-checking, a biopsy or puncture of the lymph node and brain located in the spinal region.
Diseases that can be recognized by lymphocyte analysis
Increased and decreased levels of white cells in the blood indicate many pathological conditions of the body. It is generally accepted that a low blood cell count is more dangerous than an elevated one. Doctors suspect oncological pathologies and malignant tumors in patients with a low level of lymphocytes, because with this diagnosis the immune system loses its ability to resist. An increased level of white blood cells in the blood indicates the body's ability to resist and fight pathologies and inflammation occurring in the body.
Diseases that can be diagnosed by analyzing the level of lymphocytes:
- diseased or healthy state of the immune system;
- exhaustion of the patient's body;
- the presence and development of anemia;
- intoxication of the human body;
- bone marrow problems;
- the presence and development of tumors of different types;
- viral, bacterial and infectious pathologies occurring in the body;
- assessment of the performance of the heart and vascular system.
Two types of immune system cells
Immune cells, their number, play a big role in the correct diagnosis. Their number is determined by the UAC.
Atypical cells are cells with different dimensions and functionality from others. Often occur with the following pathologies:
- pneumonia, pneumonia;
- herpes;
- mononucleosis caused by an infectious agent;
- toxoplasmosis;
- hepatitis;
- chickenpox, or chickenpox;
- lymphocytic leukemia
In popular and widespread diseases, the appearance of such cells cannot be seen:
- autoimmune pathologies;
- malaria;
- adenovirus;
- HIV;
- mumps;
- measles;
- rubella;
- flu.
Immunophenotyping
Immunophenotyping is the clinical process of characterizing cells by probing to identify a specific set of cellular markers.
Phenotyping of leukocytes involves the formation of special and unique markers on the surface and the collection of their samples for further study and identification of the causes and characteristics of the developing pathology. The process takes place in a clinical setting under the supervision of doctors and using professional equipment.
The immunophenotyping method helps doctors recognize the nature and nature of the disease, predict the further development of the pathology and stop such development.
Use of other methods and parameters for blood diagnostics
An important factor for the ESR blood test is the erythrocyte sedimentation rate. In the presence of many diseases in the human body, the parameter does not become smaller, on the contrary, it increases. These factors and dynamics attract the attention of doctors:
- increase or decrease in the number of red blood cells.
- increase or decrease in platelet count.
- production of leukocytes with changes.
Changes in the number of leukocytes, as a rule, indicate the presence of lymphoproliferative pathologies in the human body:
- lymphoma;
- lymphogranulomatosis;
- lymphocytic leukemia
The condition of an increased number of leukocytes is characteristic of:
- bronchial asthma;
- toxoplasmosis;
- brucellosis;
- cytomegalovirus;
- surgery to remove the spleen;
- problems with the thyroid gland;
- tuberculosis;
- whooping cough;
- hepatitis A;
- viruses in acute form.
Lymph node examination
The relative form of lymphocytosis, when leukocytes are constantly present in unchanged numbers, is characterized by pathology associated with a severe form of bacterial pathologies of the body, for example, typhus.
Often appears in pathologies:
- splenomegaly - an increase in the size of the spleen;
- Addison's disease;
- hyperthyroidism;
- rheumatism and similar pathologies.
A common cause of an increase in the number of blood cells is associated with a recent infection. The fact is that the resource of fast cells of the immune system is depleted over the course of the disease, they are replaced by lymphocytes - cells with a long life span. After a period of time after the disease, the level of both types of cells returns to normal. A similar condition is possible with vaccination and taking certain types of medications. If the condition of white blood cells does not improve after illness, it is important to consult a doctor to take tests again and identify the true causes of pathologies in the body. You can’t delay your examinations. It is important to identify the root cause in the early stages and undergo appropriate treatment.
A decrease in the level of red blood cells, when compared with the level of white blood cells, is characteristic of leukemia and bone marrow pathologies. Also, oncological pathologies are accompanied by an increase in the level of corpuscles, approximately five to six times higher than the normal content.
A one-time excess of the normal content of red blood cells and lymphocytes is typical for experienced smokers.
Different types of white cells increase in number with different diagnoses. Thus, with the diagnosis of myeloma, the number of B cells increases, and with mononucleosis, the number of T and B cells increases.