Mucopolysaccharidosis is a hereditary connective tissue disease associated with a disorder of glycosaminoglycan metabolism, which is characterized by a specific facial appearance, abnormalities of the eyes, bones, spleen, and liver. In some cases, the disease may be accompanied by mental retardation.
There are different types of mucopolysaccharidosis, the development of each of which is caused by a specific genetic abnormality that affects the synthesis of a specific enzyme.
Existing treatments for mucopolysaccharidosis have a low level of effectiveness.
Causes of mucopolysaccharidosis
The cause of the development of mucopolysaccharidosis is a violation of the enzymatic catalysis of glycosaminoglycans in lysosomes. With mucopolysaccharidosis, the process of breakdown and preservation of mucopolysaccharides, which are the main components of connective tissue, is disrupted. Excess mucopolysaccharides penetrate into the blood and accumulate in tissues. Therefore, this disease is classified as a storage disease.
Currently, 10 genetic types of mucopolysaccharidosis have been identified, four of which arise from impaired glycosidase activity, five from sulfatases, and one develops from transferase deficiency.
The disease is inherited in autosomal recessive and X-linked recessive types.
What is mucopolysaccharidosis?
Mucopolysaccharidoses (abbr. MPS ) are a group of inherited metabolic diseases caused by the absence or malfunction of certain enzymes that the body needs to break down molecules called glycosaminoglycans, long chains of sugars (carbohydrates) in each of our cells. These cells help build bones, cartilage, tendons, corneas, skin and connective tissue. Glycosaminoglycans (formerly called mucopolysaccharides) are also found in the fluid that lubricates joints.
People with mucopolysaccharidosis either don't make enough of one of the 11 enzymes needed to break down these sugar chains into proteins and simpler molecules, or they make enzymes that don't work properly. Over time, these glycosaminoglycans accumulate in blood cells, the brain and spinal cord, and connective tissues. The result is irreversible, progressive cellular damage that affects a person's appearance, physical abilities, organ and system function and, in most cases, mental development. Symptoms may be similar or different for different types of disorder.
Mucopolysaccharidoses are classified within a broader group of diseases called lysosomal storage diseases . These are diseases in which large numbers of molecules that are normally broken down into smaller pieces in intracellular compartments called lysosomes accumulate in harmful quantities in the body's cells and tissues, especially lysosomes. The main function of lysosomes is to digest dysfunctional cells and other materials (including bacteria and cellular debris).
Another lysosomal storage disease that is often confused with mucopolysaccharidosis is mucolipidosis. In this disease, in addition to smaller carbohydrates called sugars, excessive amounts of fatty substances known as lipids (another major component of living cells) accumulate. Patients with mucolipidosis may share clinical features associated with mucopolysaccharidoses (certain facial features, abnormal bone structure, and brain damage), but the diseases are different.
Types and symptoms of mucopolysaccharidosis
The following types of mucopolysaccharidosis are distinguished:
- Type I or Hurler syndrome;
- Type II or Gunther's syndrome;
- Type III or Sanfilippo syndrome;
- Type IV or Morquio syndrome;
- Type V or Scheie's syndrome;
- Type VI or Maroteaux-Lamy syndrome;
- VII type or Sly syndrome;
- Type VIII or Di Ferrante syndrome.
Symptoms of mucopolysaccharidosis are detected in a child in the first year of life and by 12-24 months they become quite pronounced.
These children experience:
- Skull in the shape of a boat keel;
- Noisy mouth breathing;
- Rough facial features;
- Stunted growth;
- Skeletal deformities;
- Gradual development of flexion contractures;
- Increase in abdominal size;
- Umbilical and inguinal hernias;
- Hydrocele;
- Changes in the eyes: clouding and enlargement of the cornea, congenital glaucoma, atrophy of the optic nerves, congestion in the fundus, pigmentary degeneration of the retina;
- Hearing loss;
- Changes in the heart;
- Mental retardation;
- Increased muscle tone, poor coordination of movements, paralysis.
In type I disease, there are no symptoms of mucopolysaccharidosis at birth. The first symptoms of mucopolysaccharidosis in the form of limited extension of the fingers are observed only at 3-6 years of age. Over time, the range of motion in other joints of the hands decreases. By puberty, all symptoms become especially pronounced.
Type II mucopolysaccharidosis is more common in boys. Patients are characterized by: scaphocephaly, rough facial features, low rough voice, noisy breathing, frequent ARVI. At 3-4 years of age, movement coordination problems occur. Progressive hearing loss, osteoarthritis, and nodular lesions of the skin of the back are observed.
In the presence of Sanfilippo syndrome (type III), the child develops normally within 3-5 years, although difficulty swallowing and awkward gait may sometimes be observed. After three years, the child begins to develop apathy, psychomotor development is delayed, speech is impaired, facial features become coarser, fecal and urinary incontinence occurs, and the child ceases to recognize others. Such children die at the age of 10-20 years due to intercurrent infections.
Type IV mucopolysaccharidosis is characterized by the appearance of the first symptoms at 1-3 years. Observed: severe growth retardation, disproportionate physique, rough facial features, kyphosis or scoliosis, chest deformation; contractures in the shoulder, elbow, knee joints; flat feet; decreased muscle strength; hearing loss; corneal dystrophy. Patients do not live to the age of 20 due to cardiopulmonary failure.
Scheie syndrome (type V) is characterized by short stature, a flattened bridge of the nose, a short neck, joint contractures, hypotonia of the muscles of the limbs, autonomic lability, decreased tendon reflexes, and significant clouding of the corneas.
Maroteaux-Lamy syndrome (type VI) first appears after 2 years. It is characterized by stunted growth, coarse facial features, a barrel-shaped chest, small upper jaw, short neck, and flexion contractures of the arm joints. The intelligence of patients does not suffer.
Mucopolysaccharidosis type VII is diagnosed only with a detailed biochemical study.
Di Ferrante syndrome (type VIII) is similar to Morquio syndrome, but is distinguished by a pronounced delay in intellectual and psychomotor development.
Orphan diseases in pediatric practice: mucopolysaccharidosis
On January 1, 2012, a new Federal Law dated November 21, 2011 No. 323-FZ “On the fundamentals of protecting the health of citizens in the Russian Federation” came into force, which for the first time introduced the concept of rare (orphan) diseases at the state level. To date, 230 items have been included in the list of orphan diseases, but if new diseases are identified, it will be replenished. According to the Formulary Committee of the Russian Academy of Medical Sciences (RAMS), there are about 300 thousand Russians with these diseases.
Rare (orphan) diseases are life-threatening or chronic progressive diseases that occur with a certain frequency and, if untreated, lead to death or lifelong disability of patients.
In different countries, the definition and list of orphan diseases are adopted at the state level; there is no single definition for them, just as there is no single criterion for classifying diseases into this group.
In our country, orphan diseases include diseases that have a prevalence of no more than 10 cases per 100,000 population.
There are about 7,000 rare diseases in the world today. About half of them are due to genetic abnormalities. Symptoms may be obvious from birth or appear during childhood.
One of the diseases included in the orphan group is mucopolysaccharidosis (MPS) (ICD-10 code E76.1 - “disorder of glycosaminoglycan metabolism”, Government Decree No. 403 of April 26, 2012).
Mucopolysaccharidosis is a group of hereditary connective tissue diseases caused by impaired metabolism of glycosaminoglycans (GAGs) (acid mucopolysaccharides) as a result of genetically determined inferiority of 1 of the 11 known enzymes involved in their breakdown. Refers to lysosomal storage diseases (table).
MPS is characterized by multisystem damage: progressive neuropsychiatric disorders, hepatosplenomegaly, cardiopulmonary disorders, bone deformities [1–3].
In the Moscow region, 3 children with MPS have been registered and are receiving treatment: 1 girl with MPS type I (Hurler-Scheie syndrome) and 2 boys with MPS type II (Hunter syndrome). Two more children are currently under examination; the type of MPS is being determined.
We present the clinical and laboratory characteristics of the disease using the example of MPS type II.
Mucopolysaccharidosis type II (synonyms: deficiency of the enzyme lysosomal iduronate-2-sulfatase (aL-iduronosulfate sulfatase), Gunter syndrome (Hunter) is an X-linked recessive disease resulting from a decrease in the activity of lysosomal iduronate-2-sulfatase, which is involved in the metabolism of GAGs . Occurs almost exclusively in boys (XY). In heterozygous women, clinical manifestations of Hunter syndrome are usually not observed (“carriers”). To date, only 2 cases of the disease have been described in girls associated with inactivation of the second, normal, X chromosome .
This is a pan-ethnic disease, the incidence in the world is about 1 in 75,000 living newborn boys. The incidence of the disease in the population varies from 1 in 165,000 (Australia) to 1 in 34,000 (Israel). The development of type II MPS is caused by mutations in the structural gene of lysosomal iduronate-2-sulfatase - IDS, located on the long arm of the X chromosome at the Xq28 locus. Currently, more than 300 different mutations in the IDS gene have been described. More than 50% of mutations are point mutations, about 26% are small deletions and insertions, and 11% are large deletions and rearrangements of the IDS gene. For Russian patients, DNA analysis of the IDS gene showed that large deletions and rearrangements of the IDS gene account for only 5.4% of the number of mutations found.
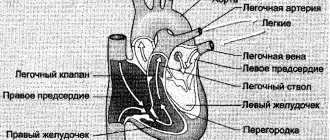
The clinical phenotype is heterogeneous and is rather conventionally divided into severe and mild forms, differing in the severity of clinical phenotypes. In patients with a severe form, clinical symptoms similar to MPS type I (Hurler syndrome) are observed, but the disease progresses more slowly (Fig.).
The disease manifests itself between the ages of 1 and 3 years. There is a change in facial features like gargoilism, growth retardation, signs of multiple bone dysostosis, coarsening and thickening of the skin, and a progressive decline in intelligence. Specific to this type of MPS are changes on the ivory-colored skin of the back, chest, neck, and “Mongoloid spots” in the lumbosacral region. Dysfunction of the digestive organs manifests itself in the form of hepatomegaly and chronic diarrhea. Neurological disorders are dominated by symptoms of progressive communicating hydrocephalus, spastic paraplegia due to spinal cord compression, and progressive hearing loss. Children with Hunter syndrome experience stiffness in large and small joints. Cardiopulmonary disorders progress. Death usually occurs in the second decade of life.
To confirm MPS type II, the level of GAG excretion in urine and the activity of lysosomal iduronate-2-sulfatase in leukocytes or a culture of skin fibroblasts are determined. In case of illness, the total excretion of GAGs in the urine increases.
DNA testing is a lengthy and complex diagnostic procedure that allows one to identify the molecular defects that lead to Hunter disease and is most often used to determine carrier status and prenatal diagnosis in families with an affected child. Indirect DNA diagnostic methods are used, based on the study of X chromosome loci located close to the IDS gene.
In addition, prenatal diagnosis is carried out by measuring iduronate-2-sulfatase activity in chorionic villus sampling at 9–11 weeks of gestation or determining the GAG spectrum in amniotic fluid at 20–22 weeks of gestation.
Most often, differential diagnosis is carried out within the MPS group, as well as with other lysosomal storage diseases (mucolipidoses, galactosialidosis, gangliosidosis, etc.).
The main approach to treating patients with MPS is lifelong enzyme replacement therapy. For MPS type II, the drug idursulfase (Elaprase) manufactured in the USA is used, registered in Europe, the USA, and Russia for the treatment of mucopolysaccharidosis type II (Hunter disease). The drug is administered weekly, intravenously, drip, slowly at a dose of 2 mg/kg.
As a clinical example, we present an extract from the medical history.
Nikita B., date of birth 12/11/2011.
Anamnesis of life. The child is from the second pregnancy (the first pregnancy ended in early miscarriage), which occurred against the background of oligohydramnios, fetal hypoxia, threat of miscarriage, and edema. Childbirth is urgent, independent. Birth weight 4040 g, height 58 cm. Breastfed from birth.
Development formula: holds head from 2 months, rolls over from 5 months, sits from 9 months, walks from 1 year to 1 month. By the year - 5 words. Previous illnesses: acute respiratory viral infection 2 times, tracheitis.
History of the disease. From birth - hydrocele of the testicular membranes, from 5 months - inguinal-scrotal hernia, at 7 months kyphosis of the lumbar spine was diagnosed, at 12 months according to electrocardiography (ECG) - early ventricular repolarization syndrome, incomplete right bundle branch block (RBBB), At 1 year 3 months, echocardiography (Echo-CG) was performed and an aneurysm of the interatrial septum (AS) was detected.
At 1 year 4 months, the child was examined at the Moscow State Research Center of the Russian Academy of Medical Sciences, MPS type II was suspected and confirmed by biochemical and molecular genetic methods.
Upon admission to the clinic, the child’s condition was moderate. Weight 15 kg. Height 93 cm. Hair is coarse, dull, macrostomia, macroglossia, short neck, mild features of gargoilism, campodactyly 4.5 fingers on the right, wide umbilical ring, kyphosis of the lumbar spine, carinatum deformity of the chest, inguinal-scrotal hernia on the left, skin - dense to the touch. Hypertrophy of the tonsils, grade 2–3. Breathing through the nose is not difficult. Vesicular breathing. Heart sounds are rhythmic, accent of the second tone. Heart rate (HR) 120 beats/min. The abdomen is increased in volume, the liver is +3.5 cm, the upper third is +4 cm. The spleen is not palpable. The chair is decorated. There are no dysuric phenomena.
Neurological status: conscious, hyperactive, easily excitable, speaks isolated words. There are no cerebral or meningeal signs. Head circumference = 50 cm. Palpebral fissures OD = OS. Pupils OD = OS. Full movement of the eyeballs. Low timbre of voice. Rapidly exhausted, walks independently, mild ataxia. Muscular hypotonia. Tendon reflexes are alive.
General blood and urine analysis without pathological changes.
Biochemical blood test - moderate increase in the level of alanine aminotransferase (ALT) (42 U/l), aspartate aminotransferase (AST) (49 U/l).
ECG: vertical position of the electrical axis of the heart (EOS), pronounced sinus tachycardia 182–200 against a background of anxiety. In orthostasis, heart rate is 111–166 beats/min.
Ultrasound examination (ultrasound) of the abdominal cavity: the liver is enlarged, the right lobe is 100 mm, the left lobe is 45 mm. The structure is homogeneous, the walls of vessels and ducts are compacted. Echogenicity is increased. The pancreas is 14 × 8 × 15 mm, the structure is heterogeneous, the echogenicity is not changed. The gallbladder has a normal shape, the lumen is clear, the walls are not thickened. The spleen is not enlarged, 62 × 32 mm. The structure is homogeneous. Kidneys without pathological changes. The testicles are in the scrotum, the vaginal process of the peritoneum is expanded on both sides to 3 mm.
Electroencephalography (EEG): diffuse cerebral changes in bioelectrical activity of an organic type in the form of dominance of delta activity with a frequency of 3–4 Hz in all parts of the convex, without a gradient, in combination with separate groups of low-frequency theta oscillations. Epileptiform activity and photoparoxysmal reaction were not detected.
Based on a comprehensive study, a diagnosis was made: “Mucopolysaccharidosis type II (Hunter syndrome). Degenerative disease of the nervous system. Delayed speech development. Hyperexcitability syndrome. Multiple bone dysostosis. Developmental defect of L1-L2 vertebrae, congenital kyphosis. 2-sided hydrocele. Umbilical hernia".
For health reasons, the child was prescribed intravenous administration of Elaprase at a dose of 0.5 mg/kg weekly (15 kg × 0.5 = 7.5 mg per administration).
Since July 2013, the child (age 1 year 7 months) has been receiving enzyme replacement therapy in the children's department of the State Budgetary Healthcare Institution MONIKI. Complex therapy includes classes with a speech therapist, speech pathologist, physiotherapy courses, physical therapy, L-carnitine (Elcar), Kudesan, glycine, Cerebrolysin, Magne B6.
Literature
- Meikle PJ et al. Prevalence of lysosomal storage disorders // JAMA. 1999. 281: 249–254.
- Neufeld EF, Muenzer J. The mucopolysaccharidoses. In: Scriver CR, Beaudet AL, Sly WS, et al (eds). The Metabolic and Molecular Bases of Inherited Disease. New York: McGraw-Hill; 2001: 3421–3452.
- Fenton CL, Rogers W. Mucopolysaccharidosis type II. eMedicine Journal. 2006. www.emedicine.com/ped/topic1029.htm. Accessed on April 3, 2006.
T. A. Bokova1, Candidate of Medical Sciences E. V. Lukina N. V. Shesterikov
GBOU MO MONIKA im. M. F. Vladimirsky, Moscow
1 Contact information
Diagnosis of mucopolysaccharidosis
Diagnosis of mucopolysaccharidosis is based on its characteristic manifestations, the results of x-ray examination, the determination of the excretion of glycosaminoglycans in the urine, and the study of enzyme activity in skin fibroblasts.
Mucopolysaccharidosis can be diagnosed before the baby is born, using amniotic fluid or chorionic villi for analysis.
Affected Populations
The prevalence of all forms of mucopolysaccharidosis is estimated at 1 case in 25,000 births. However, because mucopolysaccharidoses, especially mild forms of the disease, often go unrecognized, these diseases are underdiagnosed or misdiagnosed, making it difficult to determine their true incidence in the general population.
Estimates for specific types of mucopolysaccharidosis range from: 1 in 100,000 for Hurler syndrome; 1 in 500,000 for Scheie syndrome; 1 in 115,000 suffers from Hurler-Scheie syndrome; 1 in 70,000 with Sanfilippo syndrome; 1 in 200,000 with Morquio syndrome; and less than 1 in 250,000 people have Sly syndrome. Hunter syndrome occurs predominantly in men. In extremely rare cases, the disease has been reported in women. The incidence of Hunter syndrome is estimated at 1 in 100,000–150,000 male births.
More than 40 different lysosomal storage diseases have been identified.
Mucopolysaccharidosis type 1. Diagnostics
Laboratory research
The following studies are indicated for patients with suspected mucopolysaccharidosis type 1:
- Lymphocytes in blood smears can be examined for the presence of abnormal cytoplasmic structures.
- Urinary levels of mucopolysaccharides, dermatan sulfate and heparan sulfate increase.
- Levels of L-iduronidase can be determined in cultured fibroblasts and in leukocytes.
- Prenatal diagnosis of enzyme levels can also be performed by analyzing amniotic cells and chorionic villi.
Visualization
- In severe cases of mucopolysaccharidosis type 1, skeletal x-rays (especially the spine) may be helpful in detecting spinal bone deformities.
- Echocardiography is useful in determining the nature of cardiac complications.
Notes
- OMIM 607014 (English)
- OMIM 607016 (English)
- OMIM 607015 (English)
- OMIM 309900 (English)
- OMIM 252900 (English)
- OMIM 252920 (English)
- OMIM 252930 (English)
- OMIM 252940 (English)
- OMIM 253000 (English)
- OMIM 253010 (English)
- OMIM 253200 (English)
- OMIM 253220 (English)
- ↑ 1 2 3
T. R. Harrison.
Internal diseases in 10 books. Book 8. Trans. from English M., Medicine, 1996, 320 pp.: ill. Chapter 316. Lysosomal storage diseases (pp. 250-273)
. med-books.info. Retrieved November 30, 2014. - ↑ 1 2
Internal diseases: textbook: in 2 volumes / ed.
V. S. Moiseeva, A. I. Martynova, N. A. Mukhina. — 3rd ed., rev. and additional - 2013. - T.2. — 896 p.: ill.. Part XIII.
Hereditary storage diseases . vmede.org. Retrieved January 26, 2015.
Standard Treatments
There is currently no cure for these disorders. Medical care is aimed at treating systemic diseases and improving a person's quality of life. Dietary changes will not prevent the disease from progressing.
Surgery can help drain excess cerebrospinal fluid from the brain and free nerves and nerve roots compressed by skeletal and other abnormalities. Corneal transplantation can improve vision in people with significant corneal clouding. Removing the tonsils and adenoids can improve breathing in people with obstructive airway disorders and sleep apnea. Some people may need to have an endotracheal tube surgically inserted to help them breathe.
Enzyme replacement therapy is currently used to treat MPS I, MPS II, MPS IVA, MPS VI and MPS VII types, and is also being tested for other mucopolysaccharidose disorders. Enzyme replacement therapy involves intravenous administration of a solution containing an enzyme that is not present in the body. It does not treat the neurological manifestations of the disease, but has been shown to be effective in reducing non-neurological symptoms and pain.
Bone marrow transplantation (BMT) and cord blood transplantation (UCT) have had limited success in the treatment of mucopolysaccharidosis. Abnormal physical signs other than those affecting the skeleton and eyes may be improved, but neurological outcomes may vary. BMT and TPC are high-risk procedures and are usually performed only after careful evaluation and family consultation.
Physical therapy and daily exercise can delay joint problems and improve mobility.
Treatment of mucopolysaccharidosis
Early diagnosis with determination of the clinical and laboratory type of this pathology is important in the treatment of a child with mucopolysaccharidosis, since each variant of the course of the disease requires an individual approach to the use of an appropriate treatment method. A group of specialists, including a pediatric neonatologist, a plastic surgery specialist, an orthopedist, a neurosurgeon, an ophthalmologist and an otolaryngologist, takes part in determining the tactics for the management and treatment of a patient suffering from mucopolysaccharidosis of one type or another.
Hormonal drugs such as glucocorticoids, corticotropin and thyroidin are used for treatment. These drugs contribute only to a temporary improvement in the patient’s condition. Vitamin A, administration of dextran-70, as well as transfusion of plasma blood products are also used to treat mucopolysaccharidosis, however, like hormonal drugs, they only provide a temporary improvement in the condition.
In world medical practice, there are several treatment methods used for mucopolysaccharidosis:
- symptomatic:
- medicinal;
- surgical;
- physiotherapeutic - electrophoresis of lidase on the area of the affected joints, magnetic therapy, paraffin applications, laser puncture, exercise therapy with effects on the spine and joints, general massage, sanitation of chronic foci of infection of the nasopharynx and oral cavity.
- replacement therapy;
- stem cell transplantation;
- antiglaucomatous operations;
- hernia repair;
- adenotonsillectomy;
- tracheostomy;
- shunting for hydrocephalus;
- surgery for carpal tunnel syndrome;
- heart valve replacement.
Treatment consists of prescribing hormonal drugs such as:
- ACTH - to reduce the synthesis of mucopolysaccharides;
- thyroidin;
- glucocorticoids;
- corticotropin;
- prednisolone.
However, the use of hormonal drugs gives only temporary results.
Types
There are main symptoms of this disease, which include:
- severe skeletal deformities;
- deformations of the skull bones, ears, curvature of teeth;
- coarsening of facial features;
- growth retardation;
- mental retardation is often observed;
- decreased or complete limitation of joint mobility;
- frequent development of hernias (of different localization);
- decreased hearing and vision;
- damage to internal organs and predisposition to frequent infectious diseases.
Depending on how severe the physical and psychological disorders are, there are seven types of the disease mucopolysaccharidosis. In this case, the main ones, which are found more often than others, are four types.
Mucopolysaccharidosis type 1
Mucopolysaccharidosis type 1 (Hurler's disease). This pathology is the most rapidly progressive, occurring with severe symptoms. A characteristic symptom for it is deformation of the skull with the development of coarse facial features. By the age of two, the clinical picture is already fully expressed and is represented by serious skeletal deformations, disruption of the heart, liver and spleen, as well as the identification of multiple hernias. The prognosis of the disease is extremely unfavorable.
Mucopolysaccharidosis type 2
What it is? This type of mucopolysaccharidosis is also called Hunter's disease. The pathology most often affects boys aged 2-3 years. Clinical manifestations of the disease are similar to mucopolysaccharidosis type IH - the following are observed:
- skarocephaly;
- rough facial features;
- low timbre of voice;
- difficulty breathing - appears due to deformation of the bones of the facial skeleton.
With further progression of the disease, the following signs appear:
- intelligence decreases;
- coordination of movements is impaired;
- The mood of such a patient is unstable - so-called emotional lability is noted - from bouts of laughter to crying. Such sudden mood swings can occur at any time.
A physical examination reveals the following:
- a slight enlargement of the spleen and liver is detected;
- Specific nodules are identified on the skin of the back.
An instrumental examination reveals:
- corneal clouding that progresses;
- increasing hearing loss.
Of all the instrumental diagnostic methods, the most informative is radiography of various fragments of the musculoskeletal system - the skull, ore cell, pelvis, and so on. In this case, the radiological signs are the same as for mucopolysaccharidosis type IS.
Patients with this diagnosis are prone to developing diseases of the respiratory system:
- tracheitis;
- bronchitis;
- pneumonia.
It should be noted that mucopolysaccharidosis type II can develop in two ways:
- unfavorable (option A);
- favorable (option B).
Type 3
Mucopolysaccharidosis type III (Sanfilippo syndrome) is characterized by severe neurological symptoms. These include progressive dementia, aggressive behavior, hyperactivity, seizures, some deafness and vision loss, and an inability to sleep more than a few hours at a time. Mucopolysaccharidosis type 3 affects patients differently. Development of mental and motor skills may be somewhat slow. Patients experience:
- a marked decline in learning ability from ages 2 to 6, followed by eventual loss of language skills and some hearing loss.
- Some children may never learn to speak.
- Aggressive behavior, hyperactivity, advanced dementia and irregular sleep can make it difficult to supervise children, especially those who have normal physical strength.
- As the disease progresses, children become increasingly unsteady and most are unable to walk by the age of 10 years.
With age, skin folds and changes in facial features, bone and skeletal structures become noticeable. Growth usually stops by age 10. Other problems may include a narrowing of the airway in the throat and enlargement of the tonsils and adenoids, making swallowing difficult.
Life expectancy in type III mucopolysaccharidosis is extremely variable. Most sufferers live into their teens, and some live longer, into their twenties or thirties. The incidence of mucopolysaccharidosis type 3 (for all four subtypes combined) is about one in 70,000 births.
Mucopolysaccharidosis type 4
Mucopolysaccharidosis type IV (Morquio syndrome, Morquio disease). The disease was first described independently by the Uruguayan pediatrician L. Morquio and the English radiologist JF Braiisford in 1929. Frequency up to 1: 40,000. Children are born without signs of the disease.
The first symptoms appear at the age of 1-3 years, and by 7-8 years the clinical picture is already fully expressed:
- There is a sharp growth retardation (the height of an adult patient is about 100 cm),
- disproportionate physique (relatively short torso, microcephaly, short neck),
- rough facial features
- chest deformation (chicken-shaped, barrel-shaped, keel-shaped),
- kyphosis or scoliosis of the thoracic and lumbar spine.
- Nutrition reduced.
- Contractures occur in the elbow, shoulder, and knee joints, valgus deformity of the lower extremities and flat feet are noted. Muscle strength is reduced.
In the case of compression of the spinal cord, in addition to muscle hypotonia, damage to the pyramidal system is noted, and the development of paraplegia and respiratory paralysis is possible. The skin is thickened, its turgor and elasticity are reduced. Umbilical and inguinal hernias and separation of the rectus abdominis muscles are often detected. Hearing loss and degenerative processes in the cornea are often observed. Almost all patients who live to age 20 develop deafness. Intelligence is not reduced.
Type IS
Mucopolysaccharidosis type IS or Scheie's disease (described in 1962 by the American ophthalmologist Scheie) is a later, relatively benign variant of mucopolysaccharidosis type IH (Hurler syndrome). Until 3-6 years of age, children's development corresponds to the norm. The first sign is Dupuytren's flexion contractures of the fingers. Subsequently, extension in the wrist, elbow and shoulder joints is limited. Contractures of the lower extremities are usually mild. The full clinical picture of mucopolysaccharidosis is formed by the beginning of adolescence.
Patients with mucopolysaccharidosis are stocky, short, with coarse facial features and well-developed muscles. There is increased hair growth (hypertrichosis). Inguinal or umbilical hernias often occur. The skin on the fingers is stretched and thickened. Due to compression of the median nerve, the development of carpal tunnel syndrome is possible, accompanied by atrophy of the muscles of the thenar region and paresthesia in the area of the third-fourth fingers.
Some patients have aortic stenosis, aortic valve insufficiency, retinal pigmentary dystrophy, glaucoma and corneal opacities. Intelligence is normal, enlargement of the spleen and liver is uncharacteristic. Radiographs show a picture similar to mucopolysaccharidosis type IH, but the pathological changes are less pronounced.
Mucopolysaccharidosis type 6
What kind of disease is this? Mucopolysaccharidosis type VI (otherwise called Maroteaux-Lamy syndrome or Moroto-Lamy disease) - the first symptoms of this form begin to appear in children after the age of 2 years. Typical features are growth retardation, coarsening of facial features (the same as in Guler syndrome, but not as pronounced), small upper jaw, barrel-shaped chest, excessively short neck, shortened clavicles.
One can note the appearance of flexion contractures of the joints of the arms (patients are not able to independently raise their arms up); with the passage of time, contractures also appear in the joints of the lower extremities, and gait disturbances are characteristic. Quite often, frequent acute respiratory infections are also included here.
Hernias and hepatosplenomegaly can often be detected. In some cases, hydrocephalus and spastic paralysis may develop. The intellectual abilities of the patient with this form of mucopolysaccharidosis do not suffer. According to the severity of the symptoms of mucopolysaccharidosis, Maroteaux-Lamy disease can be divided into a typical classical form (form A) or a milder form (form B), in which the clinical manifestations are not so pronounced.
Other types of mucopolysaccharidosis
Mucopolysaccharidosis type 7 proceeds like type 3, differences are revealed only during biochemical studies. Mucopolysaccharidosis type 8 is similar in symptoms to mucopolysaccharidosis type IV, but, unlike it, is accompanied by mental retardation.
Clinical picture
In clinical practice, all 12 known mucopolysaccharidoses are divided into two groups according to phenotype: Hurler-like (10) and Morquio-like phenotype (2: Morquio syndrome A and B) [14]:
| Phenotypes of mucopolysaccharidosis[14]: | |
| Hurler-like phenotype: | Morquio-like phenotype: |
| short stature with a disproportionate skeletal structure (relatively long limbs, short torso and neck); | disproportionate dwarfism; |
| coarse facial features (sunken nose bridge, often exophthalmos, thick fused eyebrows, full lips, large tongue that often does not fit in the oral cavity); | rough facial features; |
| bone deformities (kyphoscoliosis, funnel chest deformity); | keeled chest deformity; |
| contractures of large and small joints; | hypermobility of the interphalangeal joints and stiffness of large joints; |
| muscle hypotension; | “bracelets”, “rosary beads”, increased volume of the knee joints and their valgus deformity; |
| the presence of an umbilical and inguinal-scrotal hernia; | |
| hypertrophy of the lymphatic pharyngeal ring; | |
| hypertrichosis; | |
| hepatosplenomegaly. | |
| Typical pathology: | |
| central nervous system (decreased intelligence, usually quite severe); | normal intelligence. |
| organs of vision (corneal clouding, glaucoma); | The pathology of other organs and systems is identical to the changes in patients with the Hurler-like phenotype of mucopolysaccharidosis. |
| hearing (hearing loss of varying severity); | |
| cardiovascular system (heart valve insufficiency, myocardial hypertrophy, heart rhythm disturbances); | |
| bronchopulmonary system (sinus bronchopathies with the formation of copious amounts of mucopurulent discharge, decreased respiratory function, apnea). | |
Symptoms
All patients suffering from mucopolysaccharidosis have characteristic distinctive phenotypic features in the form of the development of ugly facial features with an enlarged tongue and a large head. Patients with any type of mucopolysaccharidosis have:
- signs of retardation in physicalometric development, namely the discrepancy between bone age and passport age,
- development of a pronounced degree of scoliosis and disfiguring contractures of large joints.
- Despite the predominant damage to the nervous and/or musculoskeletal system, some types of mucopolysaccharidosis cause damage to internal organs.
- The characteristic distinctive symptoms are damage to the neurons of the cortical structures of the brain, as a result of which the child develops signs of impaired intellectual ability of varying degrees of intensity.
- With the progressive course of the disease, in almost 100% of cases of mucopolysaccharidosis, there is damage to the optic nerve, as well as the cornea of one/both eyes, accompanied by a pronounced impairment of visual function.
Diagnostics
The diagnosis of MPS is rarely made during the first year of life, since its first symptoms are nonspecific. A pathognomonic laboratory sign of the disease is the detection of increased urinary excretion of heparanium dermatan sulfate and confirmation of enzyme deficiency in leukocytes or fibroblasts.
Genetic testing is also available, which reveals mutations in the IDUA gene (4p16.3), resulting in complete deficiency of the α-L-iduronidase enzyme. X-rays reveal premature ossification of the occipital-parietal suture and pronounced elongation of the sella turcica.
Characteristic features include deformation of the vertebral bodies (“fish vertebrae”), curvature of the radius, deformations in the area of the ossification nuclei of the metaphyses and epiphyses of long tubular bones, short metacarpal bones, phalanges in the shape of a sugarloaf with normal development of the ossification nuclei of bones (differential diagnostic feature).
Treatment
Therapy should include symptomatic correction of impaired functions of internal organs (surgical, orthopedic treatment). Observation by an ophthalmologist, speech therapist, or psychiatrist is necessary.
In recent years, a method of hematopoietic stem cell transplantation has been developed, which is preferable in patients under 2.5 years of age. This method helps to increase the length and quality of life and preserves neurocognition.
Lifelong enzyme replacement therapy with laronidase is recommended for all patients with Hurler syndrome to relieve non-neurological symptoms.
Despite treatment, patients often die in the first decade of life from complications of the cardiac and respiratory systems.
Mucopolysaccharidosis type 1. Treatment
Since mucopolysaccharidosis type 1 is a genetic disorder, the prescribed therapies will contain both curative and palliative elements. Enzyme replacement therapy with loranidase may provide clinically important benefits such as improved pulmonary function and reduction of excess carbohydrates stored in organs.
Surgical assistance
Corrective surgery may be necessary for patients with mucopolysaccharidosis type 1 who have joint contractures and hand and foot deformities. Some patients may need a cornea transplant if their vision problems are severe.