Nonspecific ulcerative colitis (UC, modern name “ulcerative colitis”) is a chronic disease that manifests itself as purulent hemorrhagic inflammation of the colon wall. The prevalence of the disease in different countries ranges from 50 to 230 people per 100 thousand population. People aged 20–40 years are most often affected, men and women with equal frequency[1]. Typically, several years pass from the appearance of the first symptoms to an accurate diagnosis. Late diagnosis and the resulting inadequacy of treatment often lead to the development of severe complications and relatively high mortality (in Russia - 17 cases per million population, in Europe - 6 cases per million [2]).
General information
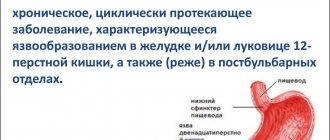
The first signs of the disease appear in the rectum, then the pathological process spreads to the entire large intestine.
According to statistics, the peak age of incidence occurs at the age of 20-40 years, while in older people the disease appears extremely rarely.
On a note! Not so long ago, ulcerative colitis of the intestine was known only to a narrow circle of medical specialists. Today, there is a multiple increase in the incidence of UC and its noticeable rejuvenation, even development in childhood.
Historical reference
A disease with similar symptoms was first described in England in 1859, and in 1885 another English doctor demonstrated a preparation of a colon with ulcers obtained at autopsy. In 1907, the domestic surgeon V.A. Oppel reported on chronic ulcerative colitis; the term UC was proposed by A.S. Kazachenko in 1913.
Prevalence and significance
The incidence is 35-100 cases per 100 thousand. The disease begins mainly in young people, from 20 to 40 years old. A later onset is not typical for colitis. It is predominantly the white population that suffers.
Risk factors
The mechanism of occurrence of UC is not fully developed, but certain risk factors for the development of this disease have been identified:
UC in close relatives;- infectious factors, presumably viruses and bacteria;
- smoking, which negatively affects the formation of protective mucus and blood supply to the intestines;
- antibacterial therapy that destroys beneficial intestinal microflora;
- Stress factors play a role in initiating exacerbation of the disease.
Causes of the disease
UC is a disease of unknown etiology, so there is no clear list of reasons for its development. However, the accumulated experience allows us to associate it with anthropogenic development factors:
- the influence of an unfavorable environment - poor ecology of the place of work and residence;
- poor nutrition;
- long-term use of medications;
- bad habits – primarily alcohol;
- high level of psychological stress.
Against their background, additional factors are activated, namely:
- bacterial or viral infection;
- dysbacteriosis;
- bad heredity;
- autoimmune processes.
All together, this forms a multifactorial set of causes for the development of ulcerative colitis.
On a note! In medicine, UC is often considered in parallel with Crohn's disease. Unlike ulcerative colitis, it has a pronounced autoimmune manifestation, but the similar influence of anthropogenic factors and general symptoms make it possible to consider the diseases together. Ulcerative colitis is often diagnosed due to Crohn's disease.
Symptoms
Symptoms of UC consist of manifestations of the local process and general symptoms. Local: abdominal pain, loose stools, difficulty passing stool, tenesmus. Common symptoms include weakness, nausea, fever, weight loss.
Tenesmus is a frequent urge to defecate without any effect and is accompanied by pain. Blood streaks and admixtures of pus and mucus are found in the stool. This is how proctitis begins - inflammation of the rectum.
Such manifestations go unnoticed by the patient for a long time, general symptoms are not yet expressed, there is no weakness, and performance does not suffer. This latent period allows inflammation to spread upward. Then constipation occurs, followed by diarrhea.
In severe cases that affect all parts of the large intestine, more severe abdominal pain is typical. It is manifested by contractions, unpleasant sensations in the lower abdomen, intensifying before going to the toilet. During defecation, a small amount of blood is lost, which eventually begins to come out in clots. This condition can cause anemia, which is accompanied by weakness, pallor, dry skin and nails.
Diarrhea that occurs with the development of intestinal inflammation can provoke dehydration and disruption of water-salt balance. The patient loses trace elements and electrolytes, which can cause manifestations in the cardiovascular, urinary, and musculoskeletal systems. The patient will be bothered by muscle cramps, weakness, cardiac dysfunction, and arrhythmias.
Symptoms not related to damage to the digestive tract include inflammation of the joints, intervertebral joints, eyelids and iris. Stomatitis and conjunctivitis may occur. Diseases of the liver and biliary organs are manifested by cirrhosis, cholecystitis, and the formation of stones in the bile ducts and kidneys. Diseases of the skin and subcutaneous fat, and damage to the superficial veins are also common.
Complications
A terrible complication is toxic megacolon (dilatation of the colon) that develops in ten percent of patients with UC.
This is an emergency condition that, without timely surgical intervention, leads to death. An actively expressed process and a large extent can provoke intestinal perforation. With this complication, the mortality rate is very high.
Strictures often occur and the intestinal lumen narrows. Massive bleeding is also a complication requiring emergency surgery. When the process is localized in the rectum, cracks, irritation of the anus, and the formation of fistulas may occur.
It has been proven that ulcerative colitis can be a background and predisposing factor for the occurrence of colon cancer.
Diagnostics
Initially, UC is diagnosed based on complaints made by patients and anamnesis. The disease often does not immediately manifest itself, so it is important to ask the patient in great detail about the occurrence of the first symptoms and their development.
During the examination, attention is paid to the condition of the skin, eyes, and abdominal pain. It is necessary to examine and digitally examine the rectum for thickening and changes in the structure of the mucosa.
The diagnosis is confirmed by fibrocolonoscopy . To do this, the doctor inserts a special flexible instrument with a camera through the anus, through which the intestinal mucosa is examined for the presence of defects, ulcers, and sources of bleeding. A biopsy may be performed. To increase the effectiveness of the study, it is recommended to cleanse the intestines of feces.
The typical endoscopic picture includes swelling, redness of the mucous membrane, and a large amount of mucus. The venous pattern and normal structure of the intestine are disrupted. A severe course is indicated by the presence of ulcers and erosions, which can be filled with pus. When the disease is long-standing, polyps and increased epithelization of the mucous membrane are often found.
X-ray examination can detect the presence of gas in the colon, changes in structure (disappearance of haustra), and large ulcers. Constant tension in the muscle layer of the intestine leads to its shortening. It is possible to detect polyps and mucosal outgrowths.
The blood test shows a picture of inflammation (many leukocytes, ESR increases). With a long-term severe course, a decrease in hemoglobin is detected - anemia. Biochemical examination reveals immune complexes and increased levels of inflammatory protein. Today, a method has emerged for detecting fecal calprotectin, which increases during an exacerbation.
Classification
Based on the localization of the pathogenic process, there are 4 basic types of colitis:
- proctitis – affecting only the rectum;
- proctosigmoiditis – involving the rectum and sigmoid colon;
- left-sided colitis - spreading to the left side of the colon;
- total – involving all parts of the large intestine.
On a note! In 20-30% of cases, the inflammatory process spreads to the appendix, while the total length of the colon is reduced by a third due to tissue swelling and thickening of the folds.
According to the clinical course:
- fulminant, or fulminant form - an acute form of colitis, especially dangerous for its complications, including tissue rupture;
- chronic relapsing – periods of stable remission are interspersed with exacerbations of the disease;
- chronic continuous - sluggish symptoms are observed in the background even during periods of general improvement.
Consequences and possible complications
A dangerous complication of ulcerative colitis can be intestinal cancer. The likelihood of death with such a pathology is inevitable. Drug therapy and surgery will prolong the patient's life, but its quality will be significantly reduced.
UC is a serious pathology that must be treated. In addition to bowel cancer, a number of other diseases can become complications of the disease.
Dangerous consequences of UC:
- colonic rupture (the colon expands with gases, resulting in rupture and peritonitis);
- formation of malignant tumors in places of inflammatory processes;
- blood loss (the consequence may be anemia or hypovolemic shock);
- the addition of intestinal infections (inflammatory processes reduce the local immunity of the digestive system).
Ulcerative colitis of the intestine: symptoms and signs
In the early stages, the disease can be diagnosed by the presence of arthritic changes in the joints, bloody diarrhea, temperature and pain in the abdominal cavity.
Otherwise, the clinical picture of the disease is very variable. Much depends on the intensity and localization of inflammation. In this case, all signs of the disease can be distinguished into intestinal and non-intestinal.
Intestinal symptoms:
- convulsions and pain syndrome are sharp pains of varying strength that do not respond to painkillers. Before bowel movement their intensity increases, after defecation it subsides;
- increased body temperature - indicators rarely go beyond subfebrile values;
- signs of intoxication with metabolites - lethargy, nausea, dizziness, lack of appetite, even anorexia;
- false urge to have a bowel movement - instead of feces, there may be a discharge of purulent mucous mass against the background of severe flatulence;
- diarrhea – the frequency of bowel movements reaches 20 times a day; periodically, impurities of blood, pus, and mucus appear in the stool, which give the discharge a fetid odor;
- constipation – periodically replaced by diarrhea.
Diagnosis reveals swelling of the mucous membrane, ulceration, and hyperemia.
Extraintestinal symptoms:
- skin pathologies caused by bacterial infection and autoimmune reactions - focal dermatitis, erythema nodosum, pyoderma gangrenosum;
- ulceration of the oropharyngeal cavity - glossitis, stomatitis, gingivitis;
- inflammatory eye diseases - conjunctivitis, uveitis, keratitis, as well as general inflammation of the eyeball (panophthalmitis);
- joint damage of varying severity - arthritis, spondylitis. Often arthritic inflammations are the first sign of future pathology;
- involvement of the digestive glands - hepatobiliary system, pancreas;
- disturbances in lung function;
Signs of ulcerative colitis of the intestine appear the same in women and men. In especially severe cases, the symptom complex is aggravated by damage to bone (osteoporosis, osteomalacia), muscle (myositis) tissue, autoimmune changes in renal structures (glomerulonephritis), thyroid gland, and blood cells.
With the long-term development of the disease, loss of weight and appetite is observed, and interest in life disappears.
Drug therapy
All patients are prescribed the following medications:
- Oral preparations of 5-Aminosalicylic acid. Mesalazine or Sulfsalazine have proven themselves well. They perfectly reduce the severity of inflammation and increase resistance to harmful factors. Relieves pain.
- Hormonal therapy. Corticosteroids (Prednisone or Prednisone) are used. Used to suppress the pathological activity of the immune system.
- Immunomodulators - to prevent exclusion from the activity of the immune system while taking corticosteroids. The use of cytostatics (Azathioprim or Methotrexate) is recommended.
- Use of biological drugs. They always act selectively, blocking the production of pro-inflammatory cytokines (tumor necrosis factor-a, IL-1, etc.) Indicated: Adalimumab, Golimumab.
- Broad-spectrum antibacterial agents are used in the presence or risk of infectious and inflammatory pathologies. The drug of choice is Metronidazole; if the effectiveness is low, it is Ciprofloxacin.
Drugs for treatment
| Name of the drug | Pharmacological group | Description of action | Instructions for use | Price |
| Mesalazine | 5-Aminosalicylic acid derivative | They block the production of prostaglandins, which are the main factor in the development of inflammation and pain. Has an antimicrobial effect against Escherichia coli. | During the period of exacerbation - up to 3.0 per day, during the period of remission - 0.24 per day. The maximum duration of therapy is 3-4 months. | Over 500 rubles |
| Sulfsalazine | 5-Aminosalicylic acid derivative | They block the production of prostaglandins, which are the main factor in the development of inflammation and pain. Has an antimicrobial effect against Escherichia coli. | During the period of exacerbation - up to 3.0 per day, during the period of remission - 0.24 per day. The maximum duration of therapy is 3-4 months. | 800-900 rubles |
| Prednisolone | Glucocorticosteroid | Inhibits phosphorylase A2, inhibits the synthesis of macrophages, neutrophils and inflammatory mediators. As a result, the severity of inflammation decreases. | During an exacerbation - up to 0.12 per day, during remission - 0.005-0.01 per day. The duration of the course is 120 days. | From 40 rubles |
| Azathioprim | Cytostatic | Suppresses pathological immune reactions. | 0.002 for every kilogram of body weight. For life. | About 300 rubles |
| Adalimumab | Biological drug | Blocks the action of the inflammatory mediator - tumor necrosis factor-alpha due to binding to the p55 and p75 receptors. | 0.08 subcutaneously 1 time every 2 weeks. For life. | About 66,000-70,000 rubles |
| Metronidazole | Broad-spectrum antibacterial agent | Inhibits the synthesis of bacterial cell walls, leading to their death. | 0.5 3 times a day - the entire period of exacerbation. | 100-120 rubles. |
| Ciprofloxacin | Broad-spectrum antibacterial agent | Inhibits the synthesis of bacterial cell walls, leading to their death. | 1.0 2 times a day - the entire period of exacerbation. | 200-250 rubles |
Diagnostics
After examining and interviewing the patient with the collection of objective and subjective symptoms, the doctor prescribes a set of instrumental and laboratory tests.
Instrumental diagnostics:
- Colonoscopy, rectosigmoidoscopy - visual examination of the walls of the colon using endoscopic equipment. The technique makes it possible to determine the boundaries of ulcerative lesions, the intensity of inflammation, check for the presence of polyps and narrowing of the intestinal lumen, and also take biomaterial for histology.
- Irrigoscopy is an x-ray of the large intestine with contrast to identify areas of inflammation, narrowing, and neoplasms.
- Hydro-MRI is a contrast tomography to assess the condition of the intestine itself and the tissues surrounding it. Allows you to note the presence of fistulas, infiltrates and other structural changes.
- Ultrasound makes it possible to assess the structure of the intestine (wall thickness, presence of dilatations) and monitor its work over time.
Laboratory methods:
- histological analysis - examination of a biopsy of the intestinal mucosa;
- general blood test - level of leukocytes and erythrocytes, ESR, hemoglobin;
- biochemical analysis - c-reactive protein, immunoglobulin;
- coprogram for occult blood, leukocytes, erythrocytes;
- stool analysis for calprotectin (intestinal inflammation detector);
- culture for bacterial infection.
Non-drug therapy
All patients are prescribed diet No. 4. And special attention is paid to replenishing the necessary vitamins (especially D and B12), as well as macro- and microelements (calcium, zinc, iron). In case of dehydration, the daily volume of fluid intake is corrected, intravenous infusion of 5% glucose and electrolyte solutions (NaCal 0.9%).
List of permitted and prohibited products
| Product group | Can | It is forbidden |
| Meat products and fish | Only low-fat varieties (perch, pike perch, chicken, beef). Cooking by boiling or steaming. | Any fatty varieties, leather, veins, tendons. |
| Soups and broths | Weak broths with the addition of boiled meat in the form of small pieces. Puree soups using vegetables. | Any strong and fatty decoctions. |
| Eggs | No more than 1 boiled chicken or 2 quail, it is advisable to consume only protein. | More than the quantity described. |
| Bakery products | Insipid cookies, white bread crackers. | All other products (especially fresh bread and butter cookies). |
| Beverages | Weak teas, cocoa. | Strong tea, coffee, carbonated drinks, alcoholic beverages. |
| Milk products | Whole milk and yoghurts in the form of cereals, puddings. | Kefir, cream, cheese, sour cream. |
| Cereals | Semolina, rice, buckwheat oatmeal. | Pearl barley, barley or millet porridge. |
Food should be at room temperature. It is better to drink 200 ml of water before each meal.
Expert opinion
Shoshorin Yuri
General practitioner, site expert
In case of moderate and severe ulcerative colitis, patients are transferred to parenteral nutrition to reduce the functional load on the affected intestinal segments and speed up regeneration.
Ulcerative colitis of the intestine: treatment
With early detection and moderate manifestation of symptoms, therapy is prescribed on an outpatient basis; in severe cases of the disease, hospitalization is indicated. Treatment is mainly symptomatic, its main goal is to achieve and maintain remission. For this purpose, a complex of conservative techniques is used.
Drug therapy:
- non-steroidal anti-inflammatory drugs (NSAIDs); in severe cases - corticosteroids;
- immunosuppressants - to suppress abnormal reactions of the immune system;
- antibiotics - to eliminate bacterial infection;
- antidiarrheal drugs;
- painkillers;
- antispasmodics;
- prokinetics – to eliminate nausea;
- hematopoietic - to replenish blood loss;
- sorbents – to eliminate intoxication;
- pro- and prebiotics – to restore healthy microflora;
- enzyme preparations.
To consolidate the result, physiotherapy is used - alternating current treatment, interference therapy, diadynamic therapy.
Attention! The result depends not only on the actions of the doctor and the prescribed procedures, but also on the personal efforts of the patient. A positive attitude, strict adherence to recommendations, and a strict diet allow many people to return to a full, active life.
What traditional methods of treating UC exist?
Alternative medicine prescriptions can only be used to treat colitis as an adjunct to drug therapy. Herbal components will improve the patient's condition, but in terms of their effectiveness they are inferior to pharmaceutical products. Before using traditional recipes, it is important to exclude allergic reactions to their ingredients.
Examples of folk remedies:
- baked apples (the introduction of such a product into the menu helps speed up the healing process of ulcers);
- bananas (the fruit contains a high concentration of vitamins, the product helps increase the body's resistance);
- decoction of watermelon rinds (take half a glass three times a day, course of therapy - two weeks);
- rice decoction (the product has the property of protecting the mucous membranes and accelerating the healing process, you should take the decoction daily, half a glass three times a day);
- turnip decoction (turnip leaves are used to prepare the decoction; the finished drink can be mixed with vegetable juice, taken one glass twice a day).
Operation
Surgical intervention is performed in exceptional cases, when the degree of damage to mucous tissues leaves no other option. Indications for surgery:
- perforations and fistulas of the intestinal wall;
- extensive blood loss (up to 100 ml per day);
- complication with the formation of megacolon;
- pronounced narrowing of the lumen and poor intestinal patency;
- purulent abscesses;
- cancerous degeneration of intestinal tissue.
Surgical options:
- complete or partial colectomy of the rectum, sigmoid, colon;
- partial excision of the rectum with ileoanal anastomosis - a section of the rectum is left and connected to the ileum for the natural removal of feces.
Diet
During treatment, patients may be transferred to parenteral nutrition.
When remission occurs, to maintain a normal state, you should follow a special diet:
- Eat fractionally, 6-8 times a day in small portions - this makes it possible, without overloading the intestines, to supply the body with the necessary nutrients.
- Eliminate from your diet all foods that can trigger the aggression of the immune system. These include hot spices, sweets, baked goods, nuts, seeds, fresh fruits, fibrous vegetables, whole grains, fried foods, coffee, strong tea, alcohol, carbonated drinks, legumes, milk (individually).
- List of allowed foods after an exacerbation: dried white bread, non-concentrated fish and meat broths, lean meat, fish, poultry, boiled semolina and rice porridge, butter, cottage cheese, eggs.
- During the period of remission, you can consume all types of dairy products, boiled vegetables, peeled fruits, crumbly cereals from any cereals (except for millet and barley), greens, non-flouring types of sweets (jelly, marmalade, marshmallows).
- Add foods and nutritional supplements high in OMEGA-3 fats to your diet - flaxseed and olive oils, fish oil, sea fish. They stabilize the reactions of the immune system and prevent the development of allergies.
- Drink as much water as possible – extensive loss of moisture due to diarrhea can cause dehydration. You should drink at least 2-3 liters of liquid in the form of pure still water, herbal teas, and compotes.
- To prevent bleeding ulcers from leading to anemia, take iron-containing foods and medications.
Important! It is believed that ulcerative colitis is a manifestation of the body’s individual sensitivity to gluten (a peculiar form of celiac disease). In this case, you should eliminate from your diet foods that may directly or indirectly contain this protein - wheat, barley, rye and their derivatives. A gluten-free diet does not cure ulcerative colitis, but it does significantly alleviate symptoms.
Treatment of UC
Nonspecific ulcerative colitis in most cases becomes a chronic disease. Pathology therapy is aimed at relieving symptoms of exacerbation and increasing periods of remission to the maximum possible period. Treatment includes taking special medications, following a diet and surgery (if there are certain indications).
Drug treatment
The goal of drug therapy is not only to stop attacks of exacerbation of the pathology, but also to increase periods of remission. The treatment schedule is drawn up individually. Some types of drugs must be taken in long courses with short breaks. If there is no result, the only way to alleviate the patient's condition is surgery.
Drug groups:
- antidiarrheals (Solutan, Platyfillin);
- iron supplements;
- aminosalicylates (Mesalazine, Sulfasalazine);
- anti-inflammatory drugs;
- immunosuppressants (Cyclosporine A, Azathioprine);
- corticosteroids (for exacerbation of the disease, Prednisolone, Budesonide);
- painkillers (Paracetamol, Ibuprofen);
- tranquilizers (Elenium, Seduxen);
- drugs from the group of antibiotics.
Surgical methods of treatment
The main disadvantage of surgical procedures for UC is their increased morbidity. A portion of the large intestine is removed. The edge of the small intestine is attached to an opening in the abdominal wall. Feces are removed from the body through a stoma. Special colostomy bags are used to collect feces.
In some cases, the ileostomy is sutured, and the process of bowel movement is resumed through the anus. This procedure involves a repeat operation.
How to treat UC with herbs?
Some types of medicinal herbs have a special effect on the digestive system. The use of decoctions helps not only to improve the functioning of the gastrointestinal tract, but also to create good prevention of complications of existing pathologies. For UC, herbs are used as an addition to the main therapy.
Examples of medicinal herbs:
- aloe juice (drink 50 g once or twice a day, the product helps heal ulcers and improve the condition of the intestinal mucous membranes);
- herbal mixture (mix chamomile, centaury and sage in equal parts, pour a tablespoon of the preparation into a glass of boiling water, take in small portions for one month);
- infusion of oak bark (a teaspoon of the preparation should be poured with a glass of boiling water, take the product once or twice a day, oak bark has a pronounced antimicrobial effect).
Prevention
Diseases induced by anthropogenic factors and associated with abnormal activity of the immune system are easier to prevent than to cure. Therefore, if you are at risk and especially if you have relatives diagnosed with UC, try to follow the following recommendations:
- Learn to relax - nervous stress and constant tension are one of the factors in the development of pathology.
- Take care of the healthy flora of your intestines - periodic intake of pro- and prebiotics will ensure the normal functioning of your immune system.
- Maintain proper diet.
- Stop drinking alcohol and smoking.
- Monitor the ecology of your place of residence and work - chemical production and periodic contact with toxic substances create a high risk of developing the disease.
And do not forget to undergo regular preventive examinations to identify intestinal pathologies - the earlier the disease is diagnosed, the higher the chances of maintaining health.
Sample menu for the week
Recommendations for creating a menu for a sick person must be given by a doctor. During the acute phase, a person is not recommended to eat food at all. Therefore, the proposed menu is suitable for the period of remission.
| Monday |
|
| Tuesday |
|
| Wednesday |
|
| Thursday |
|
| Friday |
|
| Saturday |
|
| Sunday |
|