Experts from the World Health Organization believe that a stroke is a rapidly developing total or focal impairment of brain function that lasts more than 24 hours or leads to death. Stroke in women occurs between the ages of 18 and 65. The disease affects the patient’s quality of life and can lead to disability or death. The main reason is that women present with strokes a few days after the onset of the disease, when doctors have to deal with the consequences of the disease, and not with the disease. Neurologists at the Yusupov Hospital quickly diagnose stroke using modern examination methods:
- computer and magnetic resonance imaging;
- Dopplerography of cerebral vessels;
- video electroecephalogram;
- electromyography.
Symptoms of stroke in women are most often atypical. The patient may accidentally confuse the first sign with a simple malaise or another disease. Signs of a stroke in a woman have the following characteristics:
- age. In women, stroke develops mainly between the ages of 18 and 65;
- type of disease. Most often, women develop a hemorrhagic stroke due to a rupture of a cerebral artery against the background of high blood pressure. This is facilitated by emotional shock, sudden changes in hormonal levels, increased sensitivity to stress;
- hormonal background. Pregnancy, childbirth, taking contraceptives leads to changes in blood clotting and increases the susceptibility to stroke by 20-22%;
- course of the disease. Women are more likely than men to develop stroke complications and have a higher mortality rate. The disease is characterized by a severe course; warning signs of a stroke in a woman occur suddenly;
- ignoring the disease. The first symptoms of a stroke in women do not cause alarm.
Often, the precursors of stroke in women are vegetative-vascular dysfunction and transient cerebrovascular accidents.
How does this happen?
Many women know their individual characteristics and guess the conditions that precede defects in the blood supply to the brain. It can be:
- sharply worsening headache;
- the appearance of painful dizziness;
- failures in memory, exclusion of a whole series of events from it;
- stabbing sensations in the limbs, up to loss of sensitivity;
- inability to express your thoughts due to speech problems;
- inexplicable fear and anxiety;
- darkening before the eyes, at first passing quickly, later lasting several minutes;
- difficulty swallowing and chewing food;
- mild problems in coordination of movements - “disobedience of arms and legs.”
There may be several symptoms at the same time, or they transform into each other gradually. For example, defects in the functioning of the speech apparatus are often accompanied by a decrease in visual acuity. Darkening of the eyes may be accompanied by numbness of the limbs and memory problems .
This happens because certain areas of the brain do not receive enough oxygen from the blood. Their neurons (nervous tissue cells) cease to conduct normal physiological activities and, over time, atrophic processes occur in them.
If the affected area extends to vital centers (vision, hearing, coordination of movements) or the conduction of nerve impulses along centrifugal neurons is affected, primary signs of a stroke arise, which can still be corrected.
Defects in visual function can also manifest themselves in ambiguous ways. Against the background of a general decrease in visual acuity, entire sections of the visual field may completely disappear. Complete blindness may occur in one of the eyes.
It is noteworthy that blood pressure levels at such moments differ from those that a given patient has in a normal state: they can be significantly higher or, on the contrary, greatly reduced.
Focal symptoms of the disease
One or another part of the brain is responsible for specific processes occurring in the body. When normal blood flow ceases to be provided in one of them, specific symptoms are observed. This is what the doctor relies on when making a diagnosis. You can find out which area is affected by the nature of the clinical manifestations. Frontal cortex:
- convulsions;
- slurred speech;
- inability to make voluntary movements;
- a sudden change in habitual behavior.
Parietal lobe cortex:
- tactile sensitivity is lost;
- skills in basic arithmetic, writing and reading are lost.
Temporal lobe cortex:
- deafness develops, tinnitus is recorded, and certain hallucinations appear;
- Memory is impaired and a feeling of déjà vu develops.
Symptoms are nonspecific. Rather, for the doctor, these are additional signs that help make a diagnosis.
How else can you identify an incipient stroke?
There is a simple and accessible test: a smile. Standing in front of a mirror, a woman should try to smile naturally. If the symmetry of the face is seriously disturbed (or one half practically stops moving), this is a signal to call an ambulance.
There are several more opportunities to differentiate the deterioration of your well-being:
- raise your arms up and try to hold them in this position for several seconds. Due to the onset of weakness, the arms will spontaneously drop down and hang like whips.
- stick out your tongue and try to keep it parallel to the floor strictly in the middle of your open mouth. In a pre-stroke state, this will be difficult to do: muscle tone in the tongue area will not allow maintaining symmetry.
- isolate a sentence from a conversation and say it several times in a row. Speech problems make it difficult to perform such an action: pronunciation will be confused and speech will be inconsistent. Even saying the simplest words can be difficult at times.
Frontal lobe of the brain
Responsible for mental activity, the ability to make logical constructs, synthesis of new information from existing data, behavior, muscle tone and some other functions.
- Infantilism. The patient relapses into childhood. Primary reflexes, such as grasping and sucking, return. Behavior is inappropriate for age; this is a temporary phenomenon. Recovery after the end of the pre-stroke state is spontaneous. The intervention of doctors contributes to rapid correction.
- Thinking disorders. By type of productivity decline. The patient is unable to solve basic logical problems. Inferences are impossible, judgments do not have an adequate basis. Formally, intelligence is preserved. But the woman is unable to use the resources because the conduction of nerve impulses is disrupted.
- Unsteadiness of gait. The victim cannot walk in a straight line. This is due not so much to a violation of orientation in space, but to insufficient muscle tone, a partial loss of control over the muscles.
- Behavioral disorders. The woman becomes inappropriately cheerful, whiny, and aggressive. Accented personality traits are sharpened. Therefore, the pattern (model) of the disorder is determined by the individual properties of a particular person. His character.
- Paralysis, paresis. On the one hand, opposite to the localization of the lesion. The upper and lower limbs and face are affected. The notorious distortion of facial muscles occurs, which is inherent in a classic stroke.
- Epileptic seizures. Total or large with loss of consciousness and tonic-clonic convulsions. They cover all muscle groups and the body as a whole. It is necessary to distinguish the pathological process from classic true epilepsy. This can be done both due to accompanying symptoms, clinical picture, and based on the results of instrumental diagnostics.
Lack of smell on one side. A specific sign of damage to the frontal lobes. When subcortical structures and the limbic system are involved in ischemia, the absence of odor perception is complete.
Do the symptoms of strokes differ depending on their type?
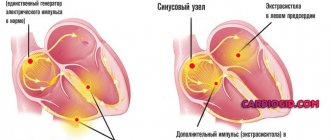
The nature of stroke in women can be ischemic, hemorrhagic, TIA (transient ischemic attack). In the first case, the first signs will be: pallor on the face and numbness, asymmetrical features, problems with speech and vision. Pain may appear in the area of the heart, and the pulse weakens.
Hemorrhagic pre-stroke status has two characteristics.
- Hyperarousal and a sharp increase in activity, periodically turning into despondency;
- A sharp drop in vitality, fainting, significant general weakness.
Against the background of both conditions, the patient can make small, frequently repeated movements: fiddling with something with her hands, tapping her fingers on hard objects, touching her ears, nose and other parts of the body. It is not uncommon to clap hands without a reason, waving them with a wide amplitude. Many people note increased sweating, facial flushing and even interruptions in breathing.
The term "transient ischemic attack" was introduced to refer to temporary dysfunctions in the blood supply to the brain. Moreover, the changes are reversible, and the main complaints last no more than a day. Their nature can be different: it all depends on which part of the brain is deprived of blood supply and how extensive the lesion is.
Despite the apparent ease of overcoming this condition, you should not ignore it. Transient ischemic attack is classified as a pre-stroke condition, which is often followed by serious pathological processes. Such a stroke has the most negative consequences, including post-stroke complications and death.
Possible complications
In the absence of therapy, the disease will certainly provoke various complications that can significantly affect the patient’s quality of life. It is believed that about 18% of patients after a stroke lose speech, or it becomes incoherent and unintelligible. More than 40% of patients remain paralyzed.
The most common complications:
- Partial or complete loss of mobility.
- Decreased intellectual capabilities.
- Deterioration of memory and concentration.
- Loss of sensation in the lower torso.
- Changes in the patient's character and behavior.
Emotional disorders occur in patients after a stroke much more often. However, the most dangerous complication is considered to be death, which occurs in approximately 30-35% of cases if assistance is not provided. It is worth noting that approximately 20% of patients recover completely.
Precursors of a stroke can appear not only in elderly women. Symptoms of the disease affect patients over 30 years of age, so you should not ignore them. When the first signs appear, you must immediately call a doctor who will conduct an examination and prescribe the correct treatment.
Article design: Vladimir the Great
What should a person who suspects he has a pre-stroke condition do?
Having noticed the symptoms of pre-stroke, a woman has no time to hesitate. Calling an ambulance must be prompt, and the description of complaints must be formulated clearly and specifically.
Before the specialists arrive, the patient must be ensured complete rest and relaxation: she must be laid down with a medium-height pillow under her head; loosen the collar, remove jewelry from the neck, open the window for fresh air. If there is an urge to vomit, it is recommended to lie on your side so that the vomit does not enter the respiratory system.
Typically, such patients know the need to measure blood pressure and take previously prescribed medications for blood pressure surges. If there are no previous appointments, it is better to wait for the doctor to arrive before treatment . The final differential diagnosis is carried out in a specialized hospital.
The main diagnostic criteria are the results of tomographic examinations, laboratory blood tests, ultrasound methods for studying the condition of the vascular bed (Dopplerography of the vessels of the brain and neck). Timely diagnosis and rational treatment are necessary conditions for alleviating the post-stroke condition.
Diagnostics
Reliable confirmation of the diagnosis of stroke is obtained by neuroimaging - CT or MRI. During instrumental examination, a single focus or multiple areas of cerebral infarction are revealed. Diagnostic methods:
- Echoencephaloscopy.
- Lumbar puncture (cerebrospinal fluid analysis). If it is impossible to do a CT scan, MRI, it is prescribed to exclude meningitis and other infections of the central nervous system, to identify signs of intracranial hemorrhage.
- Blood test to study rheological properties.
Echocardiography is performed to identify the functional characteristics of cardiac activity. A blood test is performed to determine the prothrombin index, glucose concentration, and electrolyte levels (study of kidney function).
What are the differences between the warning signs of stroke in men and women?
One of the main differences is the age of the patient. According to medical statistics, the most commonly affected female population is people over 60 years of age, while for men the cutoff age is 40 years.
Due to the heavy load on the female body during gestation, as well as a host of chronic diseases in expectant mothers, there is a possibility of developing stroke lesions and post-stroke conditions in pregnant women .
Analyzing the complex of symptoms that precede stroke problems among representatives of different sexes, we can conclude that the female body is more inclined to exhibit “nonspecific” reactions during such a period. In men, the manifestations are more classical in nature, which facilitates preliminary diagnosis and makes emergency prevention possible.
This may be why the percentage of complete recovery of the body after a stroke is higher among men than among women. Post-stroke consequences have a less negative impact on the condition of organs and systems.
Extraneurological disorders
Hormonal disorders associated with abnormalities in the central nervous system take first place in this group of pre-stroke abnormalities in women:
- violation of menstruation in terms of duration and intensity of blood loss (relevant before menopause);
- infertility, decreased fertility;
- amenorrhea.
In addition, patients are worried about: depression, apathy, complete loss of interest in everything that happens around, suicidal thoughts, severe headaches, often migraine-type, weakness, malaise, chronic fatigue syndrome, pre-syncope and short-term loss of consciousness, dyspeptic disorders.
Such symptoms can only be relieved in a hospital setting.
What can be classified as atypical signs?
Additional complaints to the general picture of pre-stroke among women include problems of consciousness. The patient notes a lack of understanding of where she is and how much time has passed since the onset of this condition. She is disoriented in space and thinks very confusedly.
Neurological symptoms are accompanied by problems in the gastrointestinal tract: a feeling of heaviness in the abdominal cavity, hiccups, nausea, sometimes turning into vomiting, significant dry mouth. Pain sensations may appear in one half of the body (as a rule, this is the side opposite to the one in the brain on which the changes occurred).
Symptoms of hemorrhagic pre-stroke condition
The clinical manifestation of hemorrhagic stroke has very clear symptoms. The woman experiences a severe headache to the point of loss of consciousness, vomiting and convulsions begin, and wheezing is clearly audible when inhaling. If, during a stoppage of blood supply to the brain, a hematoma forms in it, the face begins to rapidly turn red, and consciousness begins to become confused. The main symptoms of hemorrhagic pre-stroke are:
- loss of balance, limb spasms;
- short-term loss of consciousness;
- severe dizziness, which may cause loss of consciousness;
- intense headache;
- severe weakness in all muscles of the body;
- a sharp deterioration in vision up to its loss in one eye;
- inability to manage emotions;
- paralysis of one side of the body;
- food flows out of the mouth due to numbness of the cheeks;
If symptoms of a pre-stroke condition occur, a woman should immediately call an ambulance. In the absence of competent and effective treatment, she may remain disabled or simply say goodbye to her life. Pay attention to the condition of your loved ones; perhaps you can identify their first symptoms and signs of a pre-stroke, which will save them.
What are the risk factors for the disease?
Common stroke risk factors for men and women can be summarized as a list:
- vascular diseases;
- tendency to form atherosclerotic plaques on the inner walls of blood vessels and blood clots;
- smoking;
- frequent neuro-emotional outbursts and stress;
- excessive physical activity for a long time;
- sudden changes in blood pressure;
- overweight;
- diabetes;
- violations of such clinical characteristics of blood as increased coagulability;
- eating foods rich in “bad” cholesterol and metabolic problems;
- exposure to climatic conditions with unphysiologically low or high temperatures;
- weather dependence;
- hereditary predisposition.
At the same time, for women there is an additional number of provoking moments, including:
- Aggravated pregnancy;
- Long-term and uncontrolled use of hormonal contraceptives;
- Hereditary predisposition to thrombosis, venous pathologies, vascular anomalies.
Psychotherapists make additions to this list by indicating a higher degree of susceptibility to strokes for those women who cannot control their emotions: prone to sudden mood swings, unbalanced, with an unstable nervous system and a tendency to deep emotional experiences.
Treatment options
Treatment of a pre-stroke condition involves eliminating provoking factors - therapy for heart disease, hypercholesterolemia and other metabolic disorders, weight correction. Medical care for a stroke in a hospital setting involves immediate thrombolytic therapy - the patient is given drugs that thin the blood and dissolve blood clots. To treat the disease, pharmaceuticals are used:
- To normalize respiratory function.
- To regulate blood pressure values.
- To regulate homeostasis (self-regulation, the ability of the system to maintain a constant internal state).
- To relieve swelling of brain tissue.
- Anticonvulsant action.
Anticoagulant therapy, surgery, and neuroprotection are performed according to indications. The post-stroke condition is characterized by brain dysfunction, including cognitive impairment and dementia of varying severity, which requires appropriate treatment.
How to protect yourself from the appearance of warning signs of a stroke?
When we often talk about the dangers of individual habits and addictions, we mean the potential danger of a particular fact. In the case of pre- and post-stroke conditions, all negative aspects have a direct impact on physiological problems.
Thus, as a result of smoking, the blood vessels of the brain narrow, preventing a complete exchange between brain tissue and blood. Eating food rich in cholesterol leads to its deposition on the inner walls of blood vessels in the form of atherosclerotic plaques and clogging the lumen necessary for the movement of blood.
Constant consumption of salty and smoked foods leads to water retention in the body and increased blood pressure. Constant experiences of stressful situations are a guarantee of overstrain of the nervous system and failures in the coordination of its blood supply functions.
The list can be continued by short exposure to fresh air, a sedentary lifestyle, uncontrolled use of a number of medications, poor diet in vitamins and microelements, consumption of carbonated drinks and large amounts of coffee, and other factors.
In general, it is important to avoid all risk factors. However, with regular preventive medical examinations, the likelihood of early detection of a predisposition to stroke will greatly facilitate its diagnosis and prevent post-stroke conditions.
Temporal lobe
The work of this area ensures normal memory, internal speech and mental activity, and hearing in general.
- Epileptic seizures. As is the case with those with lesions of the frontal lobes, they develop suddenly. But they last less time. Otherwise, it is not possible to notice the difference without instrumental techniques. The difference is in the localization of the pathological impulse.
- Lack of hearing. The so-called cortical deafness. The patient completely loses the ability to navigate sounds. This is a temporary phenomenon; treatment as such does not make sense.
- Lack of speech perception. Formally, there is a noise stimulus, but it is impossible to evaluate the logic of the statements, the meaning of them, and even recognize the words.
- Verbal hallucinations of the mental type. So-called pseudohallucinations in outdated terminology. The proverbial voices in my head. Associated with disruption of Wernicke's area.
It is responsible for the production of inner speech. As a result of the anomaly, the signal moves to Broca's center.
He, in turn, identifies external stimuli and perceives them as such, as outside speech. A paradoxical reaction arises.
- Memory impairments of various types. Amnesia, failures. The feeling of a repetition of something that once happened (déjà vu).
Consequences of a mini-stroke
TIA does not go away without a trace. The symptoms will disappear, but the attack will happen again and again. In 300 people out of a thousand, TIA will lead to the development of a stroke - its most severe and most dangerous consequence.
There are two types of stroke development:
- Ischemic (the most common consequence of a microstroke), when blood flow to a certain area of the brain stops. It is the result of either a blood clot that has closed the vessel or prolonged vascular spasm.
- Hemorrhagic (rarely develops after TIA, considered only as a special case) - a severe brain catastrophe, the result of a breakthrough of large vessels and hemorrhage in the brain.
During a stroke, cells in large areas of the brain die, the patient develops paresis and plegia with complete or partial loss of sensitivity, the person ceases to adequately assess the situation, memory loss occurs, and in some cases, swallowing dysfunction occurs.
In addition to the risk of stroke, recurrent TIAs threaten:
- decline in intelligence;
- memory impairment;
- changes in mental state, lack of control over emotions and their frequent changes, when from tears to aggression, from irritability to apathy and depression - one step.
Today TIA is “getting younger.” Micro-strokes are diagnosed in women who have barely crossed the 30-year mark. Neither self-medication nor letting the disease “go on its own” is permissible, because the consequences can lead to irreversible changes.
Prevention
To avoid negative consequences, you need to engage in stroke prevention. People suffering from hypertension or other vascular diseases need to avoid physical and emotional stress, adhere to a healthy diet, and lead an active lifestyle. Medicines should be taken only as prescribed by a doctor. Be sure to undergo regular examinations in the hospital, measure blood pressure and blood glucose levels.
If a person has suffered a stroke, he will need to undergo rehabilitation. For this purpose, the patient is prescribed physiotherapeutic procedures, therapeutic exercises, and special exercises to restore facial expressions and eliminate its asymmetry. To return to the patient’s previous speech, classes with a speech therapist or speech pathologist are necessary. Impaired intellect and memory are treated using special techniques (micropolarization, Tomatis).
Limbic system
The key symptom of damage to subcortical structures (in particular the cerebellum) is a violation of orientation in space.
The patient loses understanding of the spatial structure and her position in it. A painful manifestation. If during dizziness the sense of place is formally preserved, in this case it is also lost.
At the same time, there may be a loss of the ability to learn, absorb new information and use it.
Pre-stroke, transient ischemia of the limbic system is rare: 3-5% of the total number of cases.
Symptoms and warning signs that should prompt you to see a doctor
Symptoms of microstroke in women quickly disappear; often the disease can be diagnosed only in a medical institution.
There are several “ifs”, the combination of which makes it necessary to see a doctor:
- If severe and persistent headaches begin.
- If you see black or colored circles, spots, lightning before your eyes.
- If your heart rate and pulse rate are abnormal.
- If the limbs lose sensation.
- If control over facial expressions is lost.
- If one eye is in normal condition, and the other is half-closed.
- If speech is impaired and it is impossible to pronounce a logically completed phrase.
- If coordination is impaired and movements become uncoordinated.