Bladder cancer is a disease in which a malignant tumor forms in the mucous membrane or wall of the bladder. The first symptoms of such a formation: blood in the urine, pain above the pubis. In men, the disease occurs several times more often than women, which is associated with diseases of the prostate gland, leading to stagnation of urine. Symptoms may be absent for a long time, which leads to late diagnosis and difficult treatment.
Cancer treatment using advanced methods is carried out at the Yusupov Hospital. One of the leading areas of the clinic is oncourology, specializing in the treatment and diagnosis of malignant tumors of the genitourinary system.
Causes of Bladder Cancer
No specific cause has been identified that causes RMB. Metabolites found in high concentrations in urine are known to damage the urothelium and cause malignancy. Aromatic amines and their derivatives (benzidine, nitrosamines, aminobiphenyl, aniline), benzene, detergents and dyes have such properties. For a tumor to appear, it will take about 20 years of contact with the carcinogen. The tumor can develop quickly and affect the deeper layers.
Doctors consider the following risk factors for bladder cancer:
- Work in potentially hazardous enterprises: dyeing, rubber, textile, aluminum, plastic, rubber and oil;
- Living at a distance of less than 1 km from industrial facilities that pollute the environment with smoke, soot, and chemicals;
- Work in automobile and agricultural transport: truck drivers, tractor drivers, combine operators, drivers, gas station attendants;
- Smoking for more than 10 years. Smokers suffer from bladder cancer 3 times more often. Cigarettes and cigarettes without a filter and black tobacco are especially dangerous due to their high amine content;
- A permanent urinary catheter provokes inflammation of the mucous membrane and infection;
- Chromosomal mutations, inactivation of suppressor genes;
- Long-term use of large doses of alcohol;
- Inflammation of the pelvic organs: cystitis, bladder stones. An increase in the size of the prostate gland and its damage can lead to stagnation and impaired urine output.
The influence of drugs on the appearance of malignant tumors of the bladder has been proven. Analgesics containing phenacetin, with long-term use, have a toxic effect on the kidneys and epithelium of the urinary organ. According to the results of international studies, chemotherapy using cyclophosphamide increases the risk of bladder cancer.
The appearance of bladder cancer in women is facilitated by irradiation of the pelvic organs for cancer of the cervix, uterine body and ovaries. In men, the cause of pelvic radiation may be prostate cancer.
A connection has been established between bladder cancer and schistosomiasis. This parasitic infection is endemic in the Middle East, Southeast Asia and North Africa.
Bladder cancer: classification
Tumors of the urinary organ correspond to ICD-10 code C67. Classification of bladder tumors according to ICD-10. According to the location, the RMP is divided into:
- Cancer of the triangle MP;
- Cervical cancer MP;
- Cancer of the lateral wall of the bladder;
- Cancer of the posterior wall of the bladder;
- Cancer of the anterior wall of the bladder;
- MP dome cancer.
The spread of the tumor into the muscle layer divides patients into 2 groups:
- With muscle-invasive cancer;
- With non-muscle-invasive bladder cancer.
This division is important for choosing a treatment strategy for patients, since non-invasive (previously called superficial) neoplasms can be removed by transurethral resection of the bladder (TUR).
Morphological classification involves division according to the histological structure of the malignant formation:
- Epithelial (carcinoma);
- Nonepithelial (sarcoma).
Epithelial neoplasms of the bladder
Transitional cell carcinoma is the most commonly diagnosed cancer. Another name for the pathology is urothelial carcinoma. Based on the degree of malignancy, low-grade and high-grade carcinoma are distinguished. Poorly differentiated urothelioma is a more dangerous form, is less treatable and returns more often.
Transitional cell carcinoma of the bladder in situ (in situ - in place) is a non-invasive flat formation limited to one layer of the wall of the urinary storage organ - the epithelium. Malignant transformation does not always affect all layers. Sometimes pathological formations are found only in the superficial or basal layer in the form of groups located among normal epithelial cells. Carcinoma in situ is the primary stage of bladder cancer, does not cause symptoms for a long time and is often diagnosed accidentally during a medical examination. The prognosis for patients with carcinoma in situ after treatment is favorable - one hundred percent five-year survival rate.
Urothelial intermediate cell tumor of the urinary organ is usually an isolated small formation protruding into the lumen of the organ. It occurs more often in older males and recurs in 8% of cases.
A nephrogenic tumor often forms against the background of chronic cystitis, after injuries and operations of the urinary organ. May be mistaken for cancer as it grows as a polyp-like formation.
Non-epithelial tumors of the bladder include:
- Tumors of fibrous tissue: fibromas - mature and fibrosarcomas - immature;
- Tumors of muscle tissue.
TNM classification
To establish the stage of the disease in oncology, the TNM typology is used, which consists of three components:
- T (from Latin tumor - tumor). Additional numbers 1-2 determine the superficial tumor process. Numbers 3-4 indicate growth of the formation into the muscular and deep layers;
- N (from Latin nodus - node). Additionally, it is indicated by the number 0 if metastases do not form in the regional lymph nodes. N1 indicates a single affected lymph node, N2 metastasis in 2-5 lymph nodes;
- M (from the Greek metastasis - movement). Using the letter M, oncologists mark the presence or absence of distant metastases.
Stages of RMP:
Stage 1 is characterized by the presence of cancer cells only in the epithelial layer, there are no metastases. With timely treatment, the five-year survival rate can be more than 90%.
Stage 2. This degree is indicated by the spread of the formation into the muscle layer. Five-year survival rate 70%.
Stage 3 has a less favorable prognosis, with a five-year survival rate of 55%. At this stage of development, in addition to germination into the muscle layer, damage to regional lymph nodes is characteristic.
Stage 4 of bladder cancer is indicated by metastases to regional and distant lymph nodes; the tumor is inoperable.
Forecast
This cancer has a peculiarity - after any treatment (except for complete removal of the bladder), there is a high probability of a new tumor appearing. In case of relapse of the disease, it is recommended to immediately remove the organ.
The 5-year survival rate of patients with well-differentiated small tumors of stages I-II and after adequate treatment is 88-94%. As a rule, the death of patients is associated with postoperative complications (impaired urinary diversion, colitis, proctitis, and so on), and not with repeated cancer growth. Timely consultation with a doctor can prevent the death of such a patient.
With an advanced process (up to stage III-IV), survival for 5 years has a lower percentage and depends on the time of initiation of therapy and the “malignancy” (degree of differentiation) of the process.
| Stage | 5 year survival rate |
| III | 45% |
| IV (if metastases are only in the pelvic tissues) | 26% |
| IV (if metastases throughout the body) | No more than 7% |
Symptoms of bladder cancer
Signs of bladder cancer:
- Hematuria;
- Pain above the pubis;
- Dysuria.
At the initial stage, the disease is asymptomatic. The most characteristic early symptom of bladder cancer of all stages is blood in the urine. There are micro- and macrohematuria. Microhematuria is detected only by microscopic analysis; macrohematuria can be detected independently in the form of drops of blood in the urine. Doctors distinguish between terminal and total hematuria.
Terminal gross hematuria is detected at the end of urination and is observed in cervical cancer. Total gross hematuria is characterized by the release of blood clots throughout the entire act of urination. This type is determined by MP formations of any position. In this case, the color of the urine changes to bright red. In the final stages of formation of the neoplasm and its disintegration, urine takes the form of meat slop.
Bleeding often appears painlessly and suddenly, and can recur several times over several days. Blood clots can close the sphincter lumen and cause difficulty in the outflow of urine. Frequent hematuria leads to blood loss, anemia and weakness.
The course of bladder cancer is accompanied by urination disorders. Dysuria is the second most common symptom of bladder cancer. Patients complain of frequent, painful urination up to 10 times a day. As the volume of malignant growth increases, the capacity of the urinary organ and the number of bowel movements decreases, and the frequency of urge increases. When the lumen of the urethra is closed by a neoplasm or blood clots, urinary retention and an attack of renal colic are observed. Prolonged stagnation of urine causes the development of infections such as pyelonephritis and cystitis.
Pain in the first stages of the disease appears above the pubis and intensifies as the size of the tumor increases.
Pain from tumors in the bladder can radiate to:
- Crotch;
- Sacral area;
- glans penis;
- Anus;
- Lower limbs.
Common symptoms of bladder cancer:
- Persistent increase in temperature;
- Fast fatiguability;
- Exhaustion, weight loss;
- Sleep disturbance;
- The appearance of swelling of the legs, perineum, and scrotum in the later stages of the disease;
- Chronic pain in the suprapubic region;
- In the terminal stage, multiple organ failure syndrome occurs.
The following organs are affected by metastases in bladder cancer:
- Bone. Tumor cells lead to increased osteoclast activity;
- Lungs;
- Liver;
- Genital organs.
Prevention
In a ten-year study of nearly 49,000 people, it was found that those who drank at least one and a half liters of water (6-8 glasses) per day had a significantly lower incidence of cancer compared to those who drank less. They also found that the risk of bladder cancer decreased by 7% for every 240 milliliters of fluid added.
Prevention of bladder cancer consists of measures to eliminate occupational hazards from chemical production: first of all, direct contact of workers with chemicals is eliminated, and medical examination is also strictly carried out. All benign papillomas of the bladder are subject to radical treatment using electrocoagulation or surgical removal. Timely treatment of inflammatory diseases is also necessary.
Recent studies have revealed a direct connection between bladder cancer and smoking, so quitting smoking is often considered a necessary preventive measure to prevent various cancers, including bladder cancer.
Diagnosis of bladder cancer
The most important factor in the successful treatment of such diseases is early diagnosis. The earlier the tumor is detected, the lower the risk of complications. BC can recur in 50% of cases, so not only diagnosis is important, but also complete removal of foci of cancer cells. The diagnosis is made based on anamnesis, physical examination, and the results of laboratory and instrumental diagnostics.
Diagnosis of bladder cancer includes:
- Analysis of patient complaints and subsequent physical examination. During the examination of the patient, the doctor palpates the bladder and possible areas of metastasis.
- Laboratory tests of blood and urine. General and biochemical blood tests do not provide the necessary information to establish a diagnosis of bladder cancer. A specific method is the determination of the UBS protein, the bladder cancer antigen. If the result is positive, the amount of protein is increased 15 times. However, false-positive results are possible in inflammatory diseases of the urinary system. Among other urine tests, microexamination of urine sediment is used to detect the presence of pathological cells. In this case, a study of swabs from the walls of the affected organ is more informative. Cystoscopy does not always provide an opportunity to determine an unmistakable conclusion and is used in the presence of contraindications to cystoscopy or as a screening test to determine bladder cancer at an early stage;
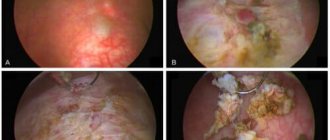
- Instrumental research. The most informative way to detect bladder cancer is cystoscopy. This invasive but highly informative method allows you to determine the size, location, shape and growth pattern of the pathological lesion. Cystoscopy provides the opportunity to take a biopsy - a piece of tissue for the differential diagnosis of cancer and a precancerous condition. If a biopsy is performed correctly, the procedure is not dangerous to the patient’s health and does not affect the rate of development of the tumor.
Using ultrasound of the pelvic organs, the shape, growth pattern, size of the pathological focus, as well as the presence of metastases in the lymph nodes are determined. The study is highly informative for tumor sizes greater than 5 mm.
Excretory urography displays the patency of the urinary tract, which may be impaired due to formation pressure or a blood clot.
CT and MRI for bladder cancer determines the presence of a tumor that has invaded nearby organs. CT helps determine the stage of bladder cancer formation according to TNM.
To detect the spread of MP formation to neighboring organs, pelvic arteriography is used (study of the pelvic vessels after administration of a contrast agent).
The Yusupov Hospital has everything necessary for testing and diagnosing bladder cancer. The advantage of the clinic is comfortable examination conditions, modern high-tech equipment at the disposal of specialists of various profiles, professionals in their field.
Bladder cancer treatment
Treatment of bladder cancer at the first stage, when cancerous tumors are located on the superficial layers of the urothelium, should begin with a TUR of the bladder. TUR - transurethral resection. Based on this operation, a decision is made as to whether or not the tumor has grown into the muscular layer of the bladder wall. Morphological analysis of the substance identified using TUR is an important step in determining the diagnosis of bladder cancer.
BCG therapy for bladder cancer is based on long-term observations of patients with tuberculosis. It turned out that they suffer from such neoplasms much less often than others. This period became the reason for in-depth research into the effectiveness of BCG. BCG is a vaccine against tuberculosis, which gets its name from the abbreviation: Bacillus Calmette - Guerin, BCG. When the cells of the urinary storage organ come into contact with an immunotherapy drug (BCG), the immune system enhances the synthesis of the body's protective cells and better fights atypical cells. They resort to BCG therapy if there is a high probability of recurrent disease.
MP removal or cystectomy is resorted to only in extreme cases, when no other method has helped get rid of the pathology. Such an operation requires careful preparation and diagnosis, as well as high professionalism of the specialist. But patients are often not interested in this, but in the question of survival after such an operation.
There are several types of operations - cystectomy, in which the bladder is removed. And radical cystectomy, but it is used only in extreme cases when it is necessary to additionally remove nearby organs.
Indications for MP removal:
- Stage T3, in case of damage to the fat capsule;
- Shriveled genitourinary organ;
- Stage T4—presence of formation beyond the boundaries of the MP;
- Multiple malignant papillomas.
Contraindications to cystectomy:
- Acute form of inflammatory diseases of the urinary system;
- Low blood clotting;
- People who may not be able to withstand prolonged anesthesia.
Preparation for MP removal. The patient must undergo a consultation with an anesthesiologist, since the operation lasts from 3 to 9 hours. The patient undergoes diagnostics, which includes various procedures. A week or two before surgery, the patient can take a course of probiotics (preparations with beneficial bacteria) to reduce the risk of infection after surgery. The evening before surgery you should not consume food, liquids, nicotine, etc. Before surgery, it is necessary to have a clean-shaven groin area.
Intravesical chemotherapy is a method of combating bladder cancer, when the drug is administered not intravenously, but into the cavity of the urinary organ for direct contact with the pathological focus. Before such chemotherapy, the patient is prohibited from any liquid. There are no side effects from such therapy, such as vomiting, brittle nails, tooth loss, hair loss, or memory impairment.
Embolization for bladder cancer is an innovative way to combat distant metastases when it is not possible to quickly remove the tumor.
Prognosis and survival rate for bladder cancer:
| Stage | Description | Treatment | Forecast | Survival percentage |
| 1 | At this stage, cancerous tumors are located in the superficial layers. | Shrink or completely remove cancerous tumors using a procedure called transurethral resection (TURP). Use of chemotherapy or immunotherapy. | Fast recovery. | More than 91% |
| 2 | Cancer cells enter the muscle wall of the bladder. | Transurethral resection of the bladder along with chemotherapy (less commonly radiation therapy). | Fast recovery. | More than 73% |
| 3 | Cancer cells have spread to nearby organs. | MPs are often removed and chemotherapy is used. | After surgery, the cancer may return. | 50% can live more than 5 years. |
| 4 | Metastases to regional and distant lymph nodes, the tumor is inoperable. | It is not possible to remove cancer surgically. Uses unverified clinical trials. | Restoration is not possible. Solution: help the patient cope with the manifestations of the disease. | Less than 7%. |
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 0.06 | 1.1 | 1.1 | 14.9 | 101.6 | 0 | 0 | 0.02 | 0.3 | 0.3 | 2.54 | 15.1 |