Author
Prokopenko Mikhail Viktorovich
Head of Clinical Diagnostic Department
Doctor
Urologist
until February 28
We're giving away RUR 1,000 for all services per visit in February More details All promotions
Cystoscopy
- This is an examination of the bladder using special endoscopic equipment - a cystoscope.
A cystoscope
is a tubular instrument equipped with an optical system, illumination and special passages through which a catheter or instruments can be inserted for minor operations during the examination.
History of cystoscopy of the bladder
Even in ancient times, scientists dreamed of being able to see the internal structure of organs without cutting into the patient. The Italian physician Bozzini discovered in 1805 how the functioning of the urinary tract could be observed using a light source.
German urologist Maximillian Nitze in 1877-79. proposed to combine light and an optical device in one device. The device, which was a tube with a light bulb attached to the inner end, was passed into the bladder. The bladder was then filled with fluid.
This made it possible to examine the bladder much more conveniently and accurately.
Where is it held?
Endoscopic examination of the bladder walls is a technically difficult procedure to perform. Therefore, it can only be performed by a urologist who has a special certificate, that is, who has undergone training in this area.
It is best to register for cystoscopy at a public medical institution or a private clinic specializing in urological care.
Preparation for cystoscopy
Preparation for cystoscopy involves proper hygiene of the genital organs, which reduces the number of complications. Therefore, immediately before the bladder examination procedure, the doctor treats the patient’s genitals with an antiseptic.
Carrying out cystoscopy
Survey cystoscopy of the bladder is one of the most common examinations. This type of cystoscopy is used in cases where the information obtained through ultrasound of the bladder or CT scan of the bladder is not enough to make a diagnosis. Cystoscopy of the bladder in women is much easier than in men, since they have a shorter and wider urethra.
Cystoscopy of the bladder in men, due to the fact that their urethra is much longer, is performed under general anesthesia. In this case, local anesthesia is used for women.
Cystoscopy of the bladder is most often performed in the supine position on a urological chair or a special table with footrests. If the legs or pelvic bones are affected, cystoscopy is performed in the lateral position.
Before examining the bladder, a warm solution of novocaine or lidocaine gel or another anesthetic is injected into the urethra for pain relief. Sometimes it is allowed to take analgesics.
For better passage, the end of the cystoscope is treated with glycerin or petroleum jelly and carefully inserted through the urethra. As soon as the device reaches the bladder, residual urine is removed from the organ and its volume is measured. Then the capacity of the bladder is determined by filling its volume with furatsilin solution. Usually this is about 200 ml of solution. If there is blood or pus in the bladder, the bladder is washed before cystoscopy.
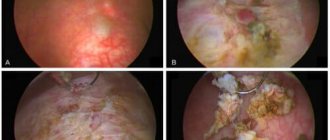
During cystoscopy, the wall and apex of the bladder are observed, then the left and right side walls, the back wall and the bottom. Cystoscopy is performed to determine the presence of ulcers, stones and foreign bodies in the bladder, and to assess the nature of the existing discharge.
Cystoscopy of the bladder in women is sometimes performed together with chromocystoscopy. For this type of study, a 0.4% solution of indigo carmine is injected intravenously and the time taken for it to be excreted in the urine is checked.
If necessary, a bladder biopsy is performed during cystoscopy.
During surgical cystoscopy of the bladder in women, urethromy is performed, bladder tumors are removed, and a catheter is installed in the ureter.
If a man has a urethral stricture, bougienage (dilation of the urethra) or urethromy is performed.
1 Cystoscopy in MedicCity
2 Cystoscopy in MedicCity
3 Consultation with a urologist
Anesthesia
Cystoscopy with a rigid (standard) cystoscope
This is a rather painful procedure, it all depends on individual sensitivity, but the use of anesthesia greatly facilitates the process.
local anesthesia
Local anesthetic drugs are injected into the urethra immediately before insertion of the device. A solution of novocaine 2%, about 10 ml, or more modern gels based on lidocaine (catedgel, instillagel) are used.
A few minutes are allotted for “freezing”, and then the doctor begins the procedure.
clamping
If we are talking about cystoscopy of men, then sometimes a gentle clamp is used just below the head of the penis. The duration of applying the clamp is no more than 10 minutes.
spinal anesthesia
Spinal (spinal, epidural) anesthesia is used in patients with high sensitivity, in the presence of somatic diseases (for example, arterial hypertension with crises) or when a therapeutic and diagnostic procedure is planned (removal of a stone or polyp).
general anesthesia
Given the short duration of the procedure, general anesthesia is performed very rarely: in children, psychiatric patients and in other rare individual cases.
As a rule, local anesthesia is quite sufficient. This is the most common type of pain relief during cystoscopy.
Cystoscopy with a flexible device
The flexible device brings less discomfort, so cystoscopy can be performed without anesthesia.
If a decision has been made about anesthesia, then the same drugs for local anesthesia are used as in the case of a rigid cystoscope.
Bladder diseases for which cystoscopy is indicated
Cystoscopy is indicated for the following diseases:
- cystitis;
- tuberculosis;
- urinary disorders;
- hematuria (using cystoscopy you can see in which area of the bladder the bleeding is located);
- suspicion of urolithiasis;
- fistulas in the vagina and bladder;
- presence of atypical cells in urine samples;
- BPH;
- malignant and benign formations of the bladder and urethra;
- bladder injuries (with the help of research, you can find out the area and nature of ruptures in the mucous membrane of the bladder);
- suspicion of the presence of a foreign body in the bladder (bladder cystoscopy) helps to accurately determine the size and location of the foreign body and determine a treatment regimen.
Contraindications for cystoscopy
Contraindications are divided into general and local.
Local contraindications
Cystoscopy is not performed in the presence of inflammatory processes and blood in the urine. In this case, cystoscopy of the bladder can lead to the development of even greater inflammation.
General contraindications:
- renal failure;
- myocardial infarction;
- pregnancy.
Complications after cystoscopy
If cystoscopy is not performed professionally, the following complications may occur:
- infections in the bladder cavity;
- the appearance of cystitis or bladder erosion;
- traumatic complications (urethral ruptures, which occur during cystoscopy in men);
- Bladder perforation (puncture of the bladder wall, accompanied by leakage of urine).
In order to avoid unpleasant bladder diseases, cystoscopy should be performed only in a well-established medical clinic!
When the procedure is contraindicated
In case of acute inflammation of the genitourinary system (cystitis, urethritis, prostatitis, orchitis), internal bleeding and obstruction of the urethra, the patient must undergo a course of treatment and wait for recovery. After which you can do cystoscopy. Otherwise, there is a high probability of causing microtrauma and aggravating the course of the disease.
The doctor will postpone the procedure if the patient:
- increased temperature or fever;
- poor blood clotting;
- signs of a viral or bacterial disease;
- injuries to the genital organs, urethral mucosa, bladder;
- chronic renal failure;
- heart attack;
- pathologies of the prostate gland and testicles.
After cystoscopy
After cystoscopy, the following unpleasant sensations may be observed (which disappear over time):
- pain and burning in the bladder (to reduce these symptoms, it is recommended to drink more fluids);
- frequent urination;
- urinary retention;
- lower back pain;
- chills, fever;
- bloody discharge in the urine (should disappear after a couple of days).
If the discharge does not disappear within 2 days after cystoscopy, then you should urgently seek advice from a urologist.
1 Consultation with a urologist after cystoscopy
2 Consultation with a urologist after cystoscopy
3 Consultation with a urologist after cystoscopy
Treatment
Often the diagnostic procedure turns into a therapeutic one. If the doctor has the technical capabilities and sufficient experience, the patient can avoid repeating such an unpleasant procedure and solve two problems in one visit.
- removal of foreign bodies and stones from the bladder and urethra. If stones or foreign bodies are small, accessible to grip, have rounded edges and are not welded to the inner wall, then there is a high probability of their safe removal. If there are large stones, you can try to split the stone and remove it piece by piece.
- removal of a small tumor or polyp
- taking a piece of tissue for histological examination. Any removed formation and biopsy material are in any case sent for histological examination to a pathologist. This allows you to diagnose cancer, determine its prevalence and type, or, conversely, confirm that the tumor/polyp is benign and there is nothing to worry about.
- dissection of strictures. When the urethra or openings are narrowed, urine does not pass properly, is retained and stretches the urethra. This is manifested by pain, difficulty urinating and requires treatment. In these cases, cystoscopy is a very gentle and effective method; the narrowing areas are stretched or incised and urine flow is restored.
- installation of stents. Stents are cylindrical devices that are inserted to widen a specific area. Stenting may be used if cutting the adhesions helps for a short time and narrowing and difficulty in passing urine occurs again.
In the multidisciplinary clinic “MedicCity”, paramount importance is attached to the treatment of urological diseases such as urethritis, cystitis, impotence, prostatitis, varicocele, etc. Professional doctors, high-quality diagnostics and modern treatment methods, an individual and delicate approach to each patient - that’s what we do We are rightfully proud.
If you read reviews about cystoscopy on the Internet, they are full of all sorts of stories about the unpleasantness of this type of examination. Thanks to reviews of cystoscopy, you can find medical institutions where procedures such as cystoscopy are performed at a high professional level. The cost of this service varies. However, the main selection criterion should still be the professionalism of urologists and good recommendations from the medical institution itself.
In our clinic, when performing cystoscopy, we use an anesthetic drug - Cathejell with Lidocaine. To ensure patient comfort, this type of examination is performed under sedation (sleep therapy).
If you are interested in the price of cystoscopy, you can see it here.
Preparatory stage
Preparation for cystoscopy begins with a consultation with a urologist. The doctor explains the purpose of the examination, the main nuances of the procedure, gives recommendations for preparation and selects the type of anesthesia together with the patient. The date of the test is determined after receiving the test results.
Laboratory diagnostics
The tests will include general urine and blood tests, and a clotting test. Additionally, FLG and ECG may be required. An electrocardiogram is usually prescribed if general anesthesia is planned or the patient has pathologies of the cardiovascular system.
Meals before the examination
There are no special instructions for changing nutrition. However, you may experience a slight feeling of nausea during the procedure. This probability can be reduced if you eat no later than 4 hours before the procedure.
When choosing general anesthesia, it is allowed to eat light food only in the evening before cystoscopy, no later than 21:00. In this case, you can drink 3-4 hours before the procedure.
Hygiene procedures
You need to take a shower in the evening or morning before cystoscopy. For adult patients, the doctor recommends removing vegetation from the perineal area, this will reduce the likelihood of pathogenic microorganisms entering the urethra and bladder.
At the initial consultation, the doctor must be informed if the patient is taking any medications.
To reduce the risk of inflammation before and after the procedure, prophylactic use of antibacterial drugs, such as Monural, is often prescribed.
Advantages and disadvantages of cystoscopy
The main advantages of the survey can be considered:
- High information content. Cystoscopy allows you to identify malignant tumors at the earliest stage of their development, which has a beneficial effect on treatment results.
- Possibility of performing treatment procedures during diagnostics.
- Get results quickly.
- Lack of specific training.
- Possibility of choosing the method of pain relief.
Procedures in government institutions are performed free of charge.
Its main disadvantage is the need to meet a number of conditions for a successful result:
- The urethra must be sufficiently patent for the endoscope.
- The bladder must be of sufficient volume.
- The liquid introduced into the cavity of the bladder should remain transparent. The presence of pus or blood in the organ makes visualization of the walls difficult.
- Severe pain and the urge to urinate should be absent, since the patient’s anxiety makes diagnosis difficult.
Cystoscopy is a technically difficult manipulation to perform. It should only be performed by a qualified doctor. In this regard, district clinics rarely have the opportunity to conduct it.
How to prepare for the examination
Preparation for cystoscopy largely depends on the nature of its implementation. The procedure can be observational, catheterization or therapeutic. But in any case, the woman must first undergo an examination by a gynecologist, do a general and biochemical blood test, and also donate blood for a coagulogram (clotting).
If anesthesia is used during the diagnosis, which is most often typical for therapeutic cystoscopy, then you should not eat anything for at least 6–8 hours to avoid vomiting. When using local anesthetics, the doctor will additionally explain whether you need to fast. In other cases, it is enough to limit yourself to light food. The attending physician must first adjust the medication intake if a woman is undergoing anti-inflammatory or anticoagulation therapy.
The same applies to regular intake of insulin and other vital medications. Doctors recommend preparing in advance for possible consequences, and on the eve of the study, take the drug “Monural” for preventive purposes. It has an antibacterial effect and will prevent the development of inflammatory complications after cystoscopy.
It is worth considering what clothes you wear for visiting a medical facility - it should be comfortable and not restrict movement. Although this may not be necessary, as private clinics usually provide specially designed clothing. Before going for an examination, it is necessary to carry out hygiene procedures for the genital organs and eliminate hair in this area.
It is very good if the woman is accompanied by someone close to her. After all, even without taking anesthetics, she may feel some weakness or minor pain, so the support of relatives will come in handy. And when using anesthesia, this is almost a mandatory condition.
Carrying out cystography
How is bladder cystography done? With the ascending method, the patient lies down on an X-ray machine and a catheter with contrast is inserted into his urethra. If necessary, local anesthesia is possible. The person is then asked to change their body position several times. For downward diagnosis, an intravenous injection of a contrast agent is performed. Vaccination cystography is also performed using a catheter, after which the patient is asked to empty the bladder.
Contraindications
Contraindications to ultrasound of the bladder depend on the method of diagnosis.
Transabdominal method (through the abdominal wall):
- urinary incontinence (ultrasound is performed only on a full bladder) - however, it is possible to catheterize the bladder immediately before the study;
- excess weight (a thick subcutaneous fat layer makes scanning difficult and reduces the diagnostic information);
- skin lesions in the lower abdomen (pyoderma, herpes, wounds, burns, infectious lesions due to syphilis and HIV);
- bladder defects (sutures and scars on the bladder wall).
Transrectal method (through the rectum):
- inflammatory bowel diseases in the acute stage (fissures, hemorrhoids, dysentery, Crohn's disease, etc.);
- absence of the rectum (as a result of surgery and replacement of this organ with an artificial anostomy to remove feces);
- narrowing (stricture) and obstruction of the rectum;
- intolerance, allergy to latex (medical rubber used to make gloves and condoms).
Transvaginal method (through the vagina):
- allergy to latex;
- the presence of a hymen;
- pregnancy more than 12 weeks;
- genital infections.
Transurethral method (through the urethra)
- intolerance to medicinal painkillers;
- inflammatory diseases of the urethra.
What diagnostic procedures is cystoscopy compatible with?
If it is necessary to determine kidney functionality, cystoscopy is often combined with chromocystoscopy.
A contrast agent is injected into a patient's vein, after which the rate of removal of colored urine from the ureter is determined.
If it begins to come out within 5 minutes, this indicates normal kidney function. A delay in the excretion of colored urine of up to 10 minutes or more indicates a malfunction of the kidneys, which requires a more extensive examination.
During cystoscopy, if indicated, biopsy material can also be taken.
Tissue samples are collected in several ways:
- Cold. A piece of tissue is cut off using forceps inserted through the endoscope.
- Transurethral resection (TUR). To cut off tissue, an electrocoagulator is used, which additionally seals the damaged vessels.
A TUR biopsy is more informative, since it allows for tissue sampling from the deep layers of the bladder walls for analysis.
Side effects
The above consequences of the procedure are observed to one degree or another in almost all subjects.
But there are a number of unwanted complications, some of which may require surgery:
- Damage to the mucous layer of the urethra. Caused by improper insertion of the endoscope or restless behavior of the patient during manipulation. Manifested by bleeding from the urethra. It usually goes away on its own, but in some cases it requires repeated endoscopic intervention for electrocoagulation of blood vessels.
- False move. Inaccurate insertion of the cystoscope leads to injury to the walls of the urethra - the tube makes a hole and enters the tissue surrounding the urethra. If the damage involves the prostate, severe bleeding may occur.
- Perforation of the bladder walls. The main reasons are the low qualifications of the urologist, the presence of adhesions, scars in the walls, and abnormal structure of the organ.
Cystitis can also be a complication of cystoscopy. Inflammation most often occurs as a consequence of insufficient compliance with the rules of asepsis and antisepsis.
With a number of diseases, such as diabetes, the risk of cystitis increases. To reduce the likelihood of inflammation, such patients need to take antibacterial agents several days before the examination and for 5-7 days after.
Serious complications are indicated by prolonged retention of urination with a normal volume of fluid consumed, fever, pain in the lumbar region, in the lower abdomen, the appearance of bloody discharge or blood clots.