Pathogenesis
Clostridia are widely distributed in the external environment. When they penetrate a wound, they quickly multiply in the absence of oxygen, which occurs when muscle tissue is crushed, where many “blind pockets” and areas with sharply reduced blood supply are formed.
Conditions under which clostridial infection develops:
- The presence of extensive lacerations with massive destruction of muscle tissue, which often occurs with gunshot wounds.
- In peacetime, the disease develops with car injuries, surgical interventions (often during laparotomies), injections, intestinal obstruction, bedsores, and even with cuts and scratches.
- Prolonged wearing of a hemostatic tourniquet applied for injuries to the great vessels contributes to the development of the disease.
- Gas gangrene develops more often in people of certain specialties. Thus, in case of mine injuries, injuries are often recorded in the thighs and buttocks. Livestock caregivers' wounds become contaminated with manure.
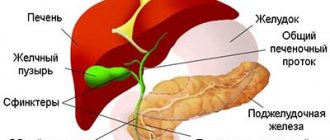
In non-traumatic (spontaneous) myonecrosis, the infection spreads hematogenously and is associated with gastrointestinal pathology, oncological processes, peripheral vascular diseases and diabetes mellitus.
Pathogenic clostridia secrete many toxins and enzymes that have necrotic, hemolytic and lethal effects. They contribute to the rapid destruction of muscle tissue and the development of toxicosis. There is no specific inflammatory reaction in the damaged area, swelling quickly develops, and gas forms in the tissues. Due to poor blood supply, antibodies do not reach the affected areas.
Gas formation, necrosis and toxicosis are the main pathogenetic mechanisms for the development of gas gangrene.
- Under the influence of toxins and enzymes in the affected areas, muscle tissue rich in glycogen is destroyed. Myonecrosis spreads very quickly, capturing more and more new areas.
- Muscle tissue destroyed by toxins is an excellent food for bacteria. Fermentation of muscle tissue glycogen leads to the accumulation of gas (hydrogen and carbon dioxide) and lactic acid. On palpation, crepitus (creaking) is detected in the affected area, and the affected area increases in size.
- When the vessels are destroyed, edema (malignant edema) occurs, which, together with gas formation, leads to an increase in interstitial pressure, aggravating ischemia and tissue anaerobiosis.
- The disease is accompanied by severe toxicosis, leading in a matter of hours to multiple organ failure and the development of septic shock.
Rice. 2. Gas gangrene of the toes and hands.
4.Treatment
Stopping the progression of gas gangrene is possible only by intensive surgical treatment of the wound with excision and removal of dead tissue (including healthy tissue). Powerful antibiotics are prescribed, hyperbaric oxygenation of the wound, drainage is applied, and the wound is left open. If, despite all efforts, the progression of gangrene cannot be stopped, the limb is urgently amputated. It is also necessary to take the most serious aseptic measures to avoid further spread of the pathogen (in particular, infection of medical personnel). Existing anti-gangrenosis serums, in general, do not yet live up to the hopes placed on them and, in addition, such vaccination is fraught with serious complications.
Incubation period
Gas gangrene develops rapidly after injury. The first symptoms appear already on days 1–3 after infection, less often on the 7th day. Fluctuations range from several hours to 3 weeks. The shorter the incubation period, the more severe the disease.
When a clostridial infection develops against the background of purulent or putrefactive inflammation, the incubation period is several weeks. Isolated cases of “dormant” infection have been described, when gas gangrene develops months and even years after complete healing. This usually occurs when there is a foreign body in the lesion.
Rice. 3. Swelling and discoloration of the horse's coat are the first signs of clostridial infection.
Forecast
In the absence of surgical care, all patients with wet gangrene die from sepsis. The main approach to treatment is still emergency high amputation. Therefore, we can say that for most patients with wet gangrene, the latter ends in the loss of a leg. To prevent the development of the disease, a diabetic needs to change his lifestyle, lose excess weight, carefully approach the treatment of the foot, and monitor minor finger injuries and abrasions. It is necessary to promptly, at the first signs of changes in the feet and nails, seek help from diabetic foot specialists - podiatrists.
Local signs and symptoms
Clostridial infection most often develops on the lower extremities, less often on the upper extremities and trunk. The presence of fractures increases the likelihood of developing the disease. Clostridial infection is characterized by local symptoms such as swelling, gas formation in tissues and muscle breakdown. There are no symptoms characteristic of banal inflammation. The nature of the wound during the disease changes very quickly.
Edema
Tissue swelling is the first sign of microbial aggression. It spreads rapidly and even with lightning speed. The swelling is aggravated by developing emphysema.
Gas accumulation
Carbon dioxide and hydrogen released by clostridia move through fatty and connective tissue layers, tissue planes of muscle tissue, causing their stratification (linear fragmentation), which is clearly visible on an x-ray. Bacteria quickly spread through “gas channels”. Signs characteristic of emphysema appear - crepitus (crunching) on palpation, and the release of gas bubbles from the edges of the wound. The purple-bronze skin becomes discolored, and bullae appear filled with a dirty-colored liquid with a putrid odor. Under pressure, the skin turns black.
Rice. 4. The appearance of blisters on the skin during gas gangrene,
Condition of muscles and fiber
When the disease occurs, protrusion of muscles from the wound is noted. They have a dull color (the appearance of boiled meat), are bloodless, lack elasticity, fall apart when grasped with tweezers, and there is no discharge from the wound. Over time, the muscles darken and acquire a greenish tint, and the fiber acquires a dirty gray color.
Rice. 5. Gas gangrene of the limb. Opening the wound with a stripe incision. The muscles are dull with areas of necrosis and protrude from the wound.
Leather
With clostridial infection, the tissues take on a lifeless appearance and are covered with a dirty gray coating. At the beginning of the disease, the skin becomes pale, then brown, purple and bluish spots appear on it. Fabrics become cold to the touch. The bottom of the wound becomes dry over time.
Rice. 6. Skin with clostridial infection.
Pain
With gas gangrene, one of the leading symptoms is severe pain, disproportionate to the damage. The pain is bursting, squeezing. Occurs as a result of swelling and gas formation.
Rice. 7. On an x-ray, the accumulation of gas in the intermuscular space has a “herringbone” appearance (Krause’s symptom).
How is gas gangrene diagnosed?
The most accurate diagnostic method is microbiological analysis of a tissue biopsy of the lesion, wound aspirate, and blood culture. Since the study takes a lot of time, and the patient needs immediate medical care, laboratory diagnostics are inferior in importance to assessing the clinical picture of the disease. When performing an ultrasound and x-ray, you can see gas bubbles in the affected tissues.
When diagnosing, a doctor takes into account the rate of increase in tissue swelling and necrosis, the presence of crunching (crepitus), and the color of the skin and muscles.
General signs and symptoms
The first signs and symptoms of gas gangrene are recorded within 6 hours after infection. Fever, impaired cardiovascular activity, changes in the patient’s mental state are the main signs of the disease.
Body temperature
In patients with severe toxicosis, body temperature rises significantly - up to 39 - 400C, in localized forms of the disease - to low-grade levels, in severe toxic shock - decreases. There are no critical changes in body temperature.
Cardiovascular activity
In patients with clostridial infection, hypotension (up to 80 mm Hg) and tachycardia (120 - 160 beats/min) are recorded. Breathing quickens and becomes shallow.
Mental state of the patient
Poisoning the patient’s body with pathogen toxins significantly changes the patient’s mental state. In the early period, patients are excited, restless and talkative. As toxemia deepens, patients become sluggish and adynamic, inadequately assess time, and do not orient themselves in space.
Toxicosis
Bacterial toxins and tissue breakdown products cause anemia, hemolytic jaundice, hemoglobinuria and renal failure. Initially, there is a decrease in the amount of urine excreted (oliguria), followed by its absence (anuria). If the outcome is unfavorable, the patient’s body temperature drops, multiple organ failure and septic shock develop. Severe toxicosis leads to loss of consciousness. If specialized care is not provided, death occurs within a few days from the moment of illness.
Rice. 8. Gas gangrene in the area of the postoperative suture.
Complications
The main complication of wet gangrene is the development of general infection of the body. This condition is observed in 85% of patients who have not undergone active surgical treatment. Sepsis inevitably leads to death. Gangrene of the legs in diabetes leads to death in 60% of patients who do not receive qualified and timely assistance.
Deep vein thrombosis is one of the very common complications that worsens the circulatory situation. Thrombotic masses can be infected and carry the infection throughout the body through the bloodstream. Deep venous thrombosis of the legs often contributes to pulmonary embolism and leads to sudden death.
Features of disease symptoms for different types of pathogens
Each of the pathogenic species of clostridia gives the course of the disease its own characteristics:
- Clostridium perfringens have fibrinolytic, toxic-hemolytic and necrotic effects.
- When infected with Clostridium septicum, hemolysis of red blood cells comes to the fore. Tissue swelling is serous-bloody in nature.
- When infected with Clostridium novyi (oedematiens), increased gas formation and hemolysis of red blood cells are observed.
- Clostridium histoliticum is particularly aggressive. Within 10 - 12 hours they are able to destroy muscle and connective tissue so much that bones become visible.
Rice. 9. Clostridium histoliticum is particularly aggressive among all types of clostridia.
PREVENTION
Here are some tips to help you reduce your risk of developing gangrene:
If you have diabetes, inspect your hands and feet daily for cuts, sores, and signs of infection such as redness, swelling, or discharge. Ask your doctor to examine your hands and feet at least once a year.
Carrying extra pounds not only increases your risk of developing diabetes, but it also puts pressure on your arteries, reducing blood flow and increasing the possibility of infection and slow wound healing.
Chronic use of tobacco products can damage blood vessels.
Wash open wounds with mild soap and water and try to keep them clean and dry while they heal.
Frostbite on the skin can lead to gangrene; frostbite reduces blood circulation in the affected area. If you notice that any area of your skin is pale, hard, cold, or numb after prolonged exposure to cold temperatures, consult your doctor.
Forms of the disease
Gas gangrene can occur with predominant damage to the muscles (clostridial myositis), or with predominant damage to the subcutaneous tissue (clostridial cellulitis). There are mixed forms of clostridial infection.
- With clostridial myositis and myonecrosis, local muscle damage is recorded. Swelling and damage to the subcutaneous tissue are uncharacteristic.
- With clostridial cellulitis, damage to the skin and subcutaneous tissue, as well as damage to the perivascular and perineural tissue sheaths, comes to the fore. In the clinic, sharp swelling affecting the skin and subcutaneous tissue comes to the fore. The color of the skin changes significantly - from pale, anemic to deep brown. Gas formation leads to the formation of blisters with brown exudate and detachment of the epidermis. The exudate has no odor.
- The classic form of gas gangrene is a mixed form, which affects the skin, subcutaneous tissue and muscle tissue. This form accounts for up to 60% of all cases of clostridial infection.
Based on the nature of tissue damage, there are 5 forms of gas gangrene:
- Emphysematous (classical).
- Edema-toxic.
- Phlegmonous.
- Putrid or putrid.
- Mixed.
Rice. 10. The photo shows clostridial post-traumatic cellulitis of the upper limb. Extensive damage. Spontaneously opened epidermal blisters are represented by fragments of the epidermis.
Classic form (emphysematous)
When infected with clostridia, swelling of the limb appears very quickly. Emphysema is growing. The gas released in large quantities quickly moves through the tissues, causing muscle separation. When pressed, a crunching sound (crepitation) is felt, and when gas escapes, a putrid odor appears. The skin is initially pale, and then becomes covered with brown, purple and bluish spots; bullae appear on them (sometimes up to 10 cm in diameter), filled with a dirty-colored liquid with the smell of rotting meat. The muscles are dull and protrude from the wound. There is no discharge from the wound. Gradually, the muscles darken and acquire a dirty green tint. Toxicosis is increasing. The pulse in the peripheral arteries disappears.
Edema-toxic form
The rapidly growing swelling comes to the fore not only in and around the wound itself, but also in areas remote from the wound. When pressed, a red-brown liquid is released. Gas formation is insignificant. No pus is formed. The fiber takes on a dirty gray color and a jelly-like structure. Necrosis develops rapidly. Single small blisters form on the skin. Intoxication is pronounced.
Phlegmonous form
The lightest of all forms. Characterized by the proliferation of coccal flora. The affected area is limited. Pus with gas bubbles is released from the wound. The muscles are of normal color with small areas of necrosis. The swelling is minor. No spots form on the skin. The pulse in the peripheral arteries is preserved.
Putrid form
It occurs when clostridial infection interacts with putrefactive flora, which leads to rapid breakdown of muscle tissue and fascia. A fetid, putrid odor emanates from the wound. Destruction of the vascular wall leads to erosive bleeding. Swelling and gas formation are present. Intoxication is significant.
Rice. 11. Clostridium bacterium under a microscope (photo on the left) and the formation of spores (photo on the right).
CAUSES
Gangrene can develop for one or more reasons:
- Lack of blood supply.
Blood provides oxygen and nutrients to cells, as well as components of the immune system and antibodies that prevent infections. Without proper blood supply, cells cannot survive and tissues are destroyed. - Infection.
If bacteria multiply unchecked for a long time, the infection itself can lead to tissue necrosis, causing gangrene.
In children
Gas gangrene in children is quite rare. There are cases of morbidity among the youthful age category. The usual causes of gas gangrene in children are:
- extensive injuries;
- extensive wounds;
- lack of proper assistance.
Children are rarely susceptible to gas gangrene. Usually at school age when injured. If you do not help the child, gas gangrene occurs. Treatment for children includes general measures. In particular, primary surgical treatment.
Gangrene in children has common symptoms. Most often, the clinical signs of gangrene in children are as follows:
- pain;
- blackening of the wound;
- chills;
- headache;
- tachycardia;
- increase in body temperature.
In addition, it should be noted that gangrene in children leads to irreversible phenomena. Most often this is fatal if proper assistance is not provided. In addition, the child’s body has not developed immunity. Clostridia easily penetrates the child's body.
go to top
Diagnosis
The diagnosis of developed G. of the limb or skin in most cases is not difficult. However, with G. of the limb in the early stages of acute obstruction of the main arteries, it can be difficult to clarify the nature and level of the lesion and assess the severity of ischemia distal to the occlusion based only on the wedge; this requires special research methods: arteriography (see), rheovasography (see Rheography), sphygmography (see), thermography (see), thermometry, capillaroscopy (see), angioscopy (see), study of microcirculation using radioisotope indication. G. of the abdominal organs is usually diagnosed during surgery, and G. of the lung - on the basis of clinical roentgenol. signs (see Lungs).