© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
The superior and inferior vena cava are among the largest vessels of the human body, without which the proper functioning of the vascular system and heart is impossible. Compression and thrombosis of these vessels are fraught not only with unpleasant subjective symptoms, but also with serious disturbances in blood flow and cardiac activity, and therefore deserve the close attention of specialists.
The causes of compression or thrombosis of the vena cava are very different, so specialists of various profiles deal with the pathology - oncologists, phthisiopulmonologists, hematologists, obstetricians-gynecologists, cardiologists. They treat not only the consequence, that is, a vascular problem, but also the cause - diseases of other organs, tumors.
Among patients with lesions of the superior vena cava (SVC), there are more men, while the inferior vena cava (IVC) is more often affected in women due to pregnancy and childbirth, obstetric and gynecological pathology.
Doctors offer conservative treatment to improve venous outflow, but they often have to resort to surgery, in particular for thrombosis.
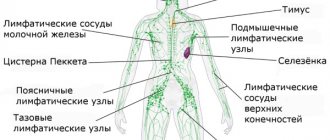
Topography of the inferior and superior vena cava
The superior vena cava (SVC) is a short trunk located in the chest to the right of the ascending aorta. It is 5-8 cm long, 21-28 mm in diameter. This is a thin-walled vessel that has no valves and is located in the upper part of the anterior mediastinum. It is formed from the confluence of two brachiocephalic veins behind the first sternocostal joint on the right.
Further, descending, at the level of the cartilage of the third rib, the vein flows into the right atrium. Topographically, the pleural layer with the phrenic nerve is adjacent to the superior vena cava on the right, the ascending aorta is on the left, the thymus is in front, and the root of the right lung is behind. The lower part of the SVC is located in the pericardial cavity. The only tributary vessel is the azygos vein.
Tributaries of the ERW:
- brachiocephalic veins;
- steam room and nameless;
- intercostal;
- veins of the spinal column;
- internal jugular;
- plexuses of the head and neck;
- sinuses of the dura mater of the brain;
- emissary vessels;
- veins of the brain.
The SVC system collects blood from the head, neck, upper extremities, organs, and chest walls.
The inferior vena cava (IVC) is the largest venous vessel in the human body (18-20 cm long and 2-3.3 cm in diameter), which collects blood from the lower extremities, pelvic organs and abdominal cavity. It also does not have a valve system and is located extraperitoneally.
The IVC begins at the level of the IV-V lumbar vertebrae and is formed by the confluence of the left and right common iliac veins. Then it follows upward, frontally in relation to the right psoas major muscle, the lateral part of the vertebral bodies, and above, in front of the right leg of the diaphragm, it lies next to the abdominal aorta. The vessel enters the chest cavity through the tendon opening of the diaphragm into the posterior, then upper mediastinum and flows into the right atrium.
The IVC system is one of the most powerful collectors in the human body (it provides 70% of the total venous blood flow).
Tributaries of the inferior vena cava:
- Parietal: Lumbar veins.
- Lower diaphragmatic.
- Two ovarian veins.
Anatomy of the venous apparatus of the heart: how does it all work?
Veins carry blood from organs to the right atrium (the exception is the pulmonary veins, which transport it to the left atrium).
Histological structure of the wall of a venous vessel:
- internal (intima) with venous valves;
- elastic membrane (media), which consists of circular bundles of smooth muscle fibers;
- external (adventitia).
The IVC refers to veins of the muscular type, in which the outer membrane contains well-developed bundles of longitudinally arranged smooth muscle cells.
In the SVC, the degree of development of muscular elements is moderate (sparse groups of longitudinally located fibers in the adventitia).
Veins have many anastomoses and form plexuses in organs, which ensures their greater capacity compared to arteries. They have high stretchability and relatively low elasticity. The blood moves through them against the force of gravity. Most veins have valves on their inner surfaces that prevent backflow.
The movement of blood through the vena cava into the heart is ensured by:
- negative pressure in the chest cavity and its fluctuation during breathing;
- suction ability of the heart;
- the work of the diaphragmatic pump (its pressure on the internal organs during inhalation pushes blood into the portal vein);
- peristaltic contractions of their walls (with a frequency of 2-3 per minute).
Comparative anatomy
For the first time, the posterior (lower) P. v. in phylogeny it appears in lobe-finned ganoids and double-breeding fishes in the form of an unpaired venous trunk flowing into the right atrium. In mammals, the renal portal system completely disappears, and the posterior (lower) renal v. acquires predominant importance compared to the posterior cardinal veins. The common cardinal veins (ducts of Cuvier) therefore carry blood from the anterior half of the body, head, neck and forelimbs. The large trunk, formed as a result of the fusion of the veins of the head, neck and forelimbs and flowing into the heart, is called the anterior (upper) P. v.
Vascular function
Veins, together with arteries, capillaries and the heart, form a single circulatory system. Unidirectional continuous movement through the vessels is ensured by the pressure difference in each segment of the channel.
Main functions of veins:
- deposition (reserve) of circulating blood (2/3 of the total volume);
- return of oxygen-depleted blood to the heart;
- saturation of tissues with carbon dioxide;
- regulation of peripheral circulation (arteriovenous anastomoses).
What symptoms bother the patient when blood flow through the vena cava is disrupted?
The main pathology of the caval veins is their complete or partial obstruction (occlusion). Violation of the outflow of blood through these vessels leads to an increase in pressure in the vessels, then in the organs from which adequate outflow is not produced, their expansion, transudation (release) of fluid into the surrounding tissues and a decrease in the return of blood to the heart.
The main signs of impaired outflow through the vena cava:
- swelling;
- change in skin color;
- expansion of subcutaneous anastomoses;
- decreased blood pressure;
- dysfunction of organs from which there is no outflow.
Superior vena cava syndrome in men
This pathology is more common between the ages of 30 and 60 years (3-4 times more often in men).
Factors that provoke the formation of cava syndrome:
- extravasal compression (squeezing from the outside);
- tumor growth;
- thrombosis.
Causes of impaired patency of the SVC:
- Oncological diseases (lymphoma, lung cancer, breast cancer with metastasis, melanoma, sarcoma, lymphogranulomatosis).
- Aortic aneurysm.
- Enlarged thyroid gland.
- Infectious lesions of the vessel - syphilis, tuberculosis, histioplasmosis.
- Idiopathic fibrous mediastinitis.
- Constrictive endocarditis.
- Complication of radiation therapy (adhesions).
- Silicosis.
- Iatrogenic damage - blockage due to prolonged catheterization or a pacemaker.
Symptoms of SVC occlusion:
- severe shortness of breath;
- chest pain;
- cough;
- attacks of suffocation;
- hoarseness of voice;
- swelling of the veins of the chest, upper limbs and neck;
- puffiness, pastiness of the face, swelling of the upper extremities;
- cyanosis or congestion of the upper half of the chest and face;
- difficulty swallowing, swelling of the larynx;
- nosebleeds;
- headache, tinnitus;
- decreased vision, exophthalmos, increased intraocular pressure, drowsiness, convulsions.
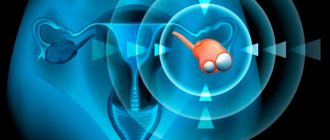
Inferior vena cava syndrome in pregnant women
During the period of bearing a child, the constantly enlarging uterus in the supine position puts pressure on the inferior vena cava and abdominal aorta, which can lead to a number of unpleasant symptoms and complications.
The situation is further aggravated by an increase in the volume of circulating blood necessary to nourish the fetus.
Hidden manifestations of IVC syndrome are observed in more than 50% of pregnant women, and clinically in every tenth (severe cases occur with a frequency of 1:100).
As a result of compression of blood vessels, the following is observed:
- decreased venous return of blood to the heart;
- deterioration of blood oxygen saturation;
- decreased cardiac output;
- venous congestion in the veins of the lower extremities;
- high risk of thrombosis, embolism.
Symptoms of aortocaval compression (occur in the supine position, more often in the third trimester):
- dizziness, general weakness and fainting (due to a drop in blood pressure below 80 mm Hg);
- feeling of lack of oxygen, darkening of the eyes, tinnitus;
- severe pallor;
- heartbeat;
- nausea;
- cold clammy sweat;
- swelling of the lower extremities, manifestation of the vascular network;
- haemorrhoids.
This condition does not require drug treatment. A pregnant woman must follow a number of rules:
- do not lie on your back after 25 weeks of pregnancy;
- do not perform exercises in a lying position;
- rest on your left side or half-sitting;
- use special pillows for pregnant women during sleep;
- walk, swim in the pool;
- during childbirth, choose a position on your side or squatting.
Thrombosis
Blockage of the superior vena cava by a thrombus is often a secondary process caused by tumor growth in the lungs and mediastinum, a consequence of mastectomy, catheterization of the subclavian or jugular veins (with the exception of Paget-Schrötter syndrome).
In the case of complete occlusion of the lumen, the following rapidly occurs:
- cyanosis and swelling of the upper body, head and neck;
- inability to assume a horizontal position;
- severe headache and chest pain, aggravated by bending the body forward.
Causes of thrombosis of the inferior vena cava:
- Primary: Tumor process.
- Birth defects.
- Mechanical damage.
- Invasion of the vessel wall by a tumor.
Clinically, the following types of IVC thrombosis are distinguished:
- Distal segment (most common location). Symptoms are less pronounced due to the good compensatory capabilities of collateral blood flow. The patient develops signs of ileofemoral thrombosis - increasing swelling of the ankles, spreading to the entire limb, lower abdomen and lower back, cyanosis, bursting sensations in the legs.
- Renal segment. It is severe, has a high mortality rate and requires surgical correction. Clinically manifested as severe pain in the lower back, oliguria, the presence of protein in the urine, microhematuria, vomiting, and increasing renal failure.
- Liver segment. The clinic of suprahepatic portal hypertension is developing: an increase in the size of the organ, jaundice, ascites, the manifestation of venous plexuses on the anterior surface of the abdomen, varicose veins of the lower third of the esophagus (with the risk of gastrointestinal bleeding), splenomegaly.
Pathologies
The IVC is characterized by the same diseases as other parts of the venous system. Blood clots may form in the lumen of the tube. Such pathologies account for about 11% of all diseases. They are conventionally divided into two groups:
- Primary thrombosis that occurs against the background of congenital anomalies of this part of the circulatory system or trauma to the vessel.
- Secondary thrombosis that occurs due to prolonged compression of the tube and tumor growth into it. Experts also include the spread of thrombosis from the lower extremities here.
Symptoms for primary and secondary IVC thrombosis are similar, but heterogeneous. The set of clinical manifestations depends on the area where the thrombus is localized. When located in the lower parts of the IVC, the pathology provokes cyanosis and swelling of the legs, buttocks and lower back, sometimes the abdomen up to the chest. If the thrombus is located near the renal branches, symptoms similar to hypertension may occur. When a tube at the level of the liver is blocked by a blood clot, the patient quickly falls into an extremely serious condition that threatens death.
The IVC syndrome, which is diagnosed only in women during pregnancy, is included in a separate category of pathologies of this vessel. It is observed in patients carrying a large fetus or multiple pregnancies. Excessive enlargement of the uterus leads to compression of the lumen of the tube and venous congestion in the pelvis and legs. The pathology is accompanied by swelling, hypotension, and disruption of the uteroplacental blood supply.
Diagnostics and clarification
To establish the cause of obstruction of blood flow through the vena cava system and select further tactics, a number of diagnostic procedures are shown:
- History taking and physical examination.
- General blood test, biochemistry, coagulogram.
- Doppler ultrasound and duplex scanning of veins.
- Plain radiography of the chest and abdominal organs.
- CT, MRI with contrast.
- Magnetic resonance phlebography.
- Measurement of central venous pressure (CVP).
Treatment methods
The choice of patient management tactics depends on the cause of blood flow disturbance in the portal veins.
Today, almost all cases of thrombosis are treated conservatively. Studies have shown that after thrombectomy, clot fragments remain on the vessel wall, which subsequently serve as a source of re-occlusion or the development of a dangerous complication of the BODY (pulmonary embolism).
Compression of a vessel by a space-occupying lesion or tumor invasion of the vein walls requires surgical intervention. The prognosis for conservative management of the disease is unfavorable.
Surgical methods
Types of surgical interventions for vena cava thrombosis:
- endovascular thrombectomy with Fogarty catheter;
- open clot removal;
- palliative plication of the vena cava (artificial formation of the lumen with U-shaped staples);
- installation of a vena cava filter.
In case of external compression of the vessel or metastatic lesion, palliative interventions are performed:
- stenting the narrowing area;
- radical decompression (removal or excision of tumor formation);
- resection of the affected area and replacement with a venous homograft;
- shunting of the obliterated area.
Drug treatment
The most effective method of conservative treatment for blockage of deep veins by a clot is thrombolytic therapy (Alteplase, Streptokinase, Actilyse).
Criteria for choosing this treatment method:
- age of thrombotic masses up to 7 days;
- no history of acute cerebral blood flow disorders in the last 3 months;
- the patient did not undergo surgical procedures for 14 days.
Additional drug support regimen:
- Anticoagulant therapy: “Heparin”, “Fraxiparin” intravenous drip with further transition to subcutaneous administration.
- Improving the rheological qualities of blood: “Reosorbilact”, “Nicotinic acid”, “Trental”, “Curantil”.
- Venotonics: Detralex, Troxevasin.
- Nonsteroidal anti-inflammatory drugs: Indomethacin, Ibuprofen.
conclusions
Impaired blood flow through the vena cava system is a pathological condition that is difficult to treat and has a high mortality rate. Also, in 70% of cases, re-occlusion or rethrombosis of the affected segment is observed within a year. The most common fatal complications are: BODY, major ischemic stroke, acute renal failure, bleeding from esophageal varices and cerebral hemorrhage.
In the case of tumor damage to blood vessels, the prognosis is unfavorable. Treatment is palliative in nature and is aimed only at alleviating existing symptoms and some continuation of the patient’s life.
Possible diseases
A common pathology is inferior vena cava syndrome. Appears as a result of various deviations. Pregnant women are at risk.
A dangerous pathology is IVC thrombosis. It often occurs in patients of different age categories. Develops under the influence of many predisposing factors:
- malignant neoplasms;
- infectious diseases;
- genetic predisposition;
- bad habits;
- chronic diseases.
People who frequently experience limb injuries are at risk. There is danger in the postoperative period. There is also a risk in women who experience complications after childbirth.
Doctors will highlight risk factors for thrombosis:
- varicose veins;
- allergic reactions;
- hormonal disorders;
- pathological structure of the vascular system;
- long bed rest.
Pathology common among children. But it mainly occurs in old age against the background of chronic diseases and insufficient immunity. The reasons for the enlargement of the inferior genital vein are associated with excessive pressure on it.