Hypothyroidism as a disease was first described in 1873, and the term “myxedema” (mucous swelling of the skin), denoting severe forms of hypothyroidism, came into use in 1878.
According to statistics, thyroid hypothyroidism is the most common disease of the endocrine system in regions depleted of iodine, affecting mainly women over 65 years of age. Insufficient intake of iodine into the body and damage to the thyroid gland cause hypothyroidism in 99% of cases; in only 1% it develops as a result of damage to the pituitary gland or hypothalamus.
Disturbances in the functioning of the thyroid gland are observed in almost a third of the world's population, while most diseases of this organ can be prevented and cured with timely diagnosis and treatment.
In children and adolescents of puberty, an increase in the size of the thyroid gland (goiter) without disruption of hormone secretion often occurs. In such cases, taking iodine preparations and observation by an endocrinologist solves the problem. Severe forms of hypothyroidism, the signs of which are difficult to determine independently, are rare in adolescents.
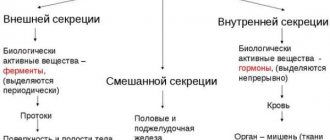
Classification by origin
Primary hypothyroidism
Primary hypothyroidism is a process that leads to the development of hypothyroidism and is localized directly in the thyroid gland. Primary hypothyroidism accounts for the vast majority of cases of this syndrome. Its prevalence affects about 2% of all people, among whom 10% are women and 3% are men. Primary congenital hypothyroidism of newborns is usually recorded in 1 child in 4-5 thousand newborns.
Primary hypothyroidism occurs as a result of autoimmune thyroiditis, during the treatment of thyrotoxicosis, as a result of the spontaneous transition of diffuse toxic goiter into this disease. Congenital hypothyroidism occurs due to dysplasia and aplasia of the thyroid gland and as a result of congenital enzymopathies.
Quite rarely, primary hypothyroidism can occur as a result of replacement of thyroid tissue with pathology in amyloidosis, sarcoidosis, Riedel's thyroiditis or cystinosis.
Secondary form
The secondary form of the disease is directly related to the hypothalamus and pituitary gland, which control the production of thyroid hormones by the thyroid gland. In this case, a completely healthy thyroid gland may produce an insufficient amount of hormones due to the lack or absence of the stimulating effect of thyroid-stimulating hormone (TSH), which will be explained by the dysfunction of three glands at once - the thyroid, pituitary gland and hypothalamus.
There may be several reasons for this failure:
- brain injuries;
- neoplasms in the brain;
- hemorrhages in the brain in the hypothalamus or pituitary gland;
- undergone chemotherapy;
- infections of the hypothalamus or pituitary gland;
- necrosis of the pituitary gland due to blood loss during surgery or trauma.
The secondary form of the disease can occur at any age and in people of both sexes with equal probability, since the above reasons do not depend on gender or age characteristics.
Tertiary hypothyroidism
The pathological process in the hypothalamus, together with reduced synthesis of releasing hormone (TSH-RH) and the lack of stimulation by it of pituitary thyrotrophs, as well as a decrease in the synthesis of thyroid-stimulating hormone and stimulation of TSH thyroid function leads to the occurrence of tertiary hypothyroidism.
It is difficult to differentiate this pathology from the secondary form of the disease, since the content of TSH-RH in the blood is very low and cannot be examined. When identifying this pathology, the TSH-RG test method comes to the rescue, in which, with the introduction of TSH-RG intravenously, a TSH test is taken in parallel, which begins to increase in tertiary hypothyroidism, and behaves calmly in secondary hypothyroidism.
Peripheral hypothyroidism
Hypothyroidism due to impaired transport, metabolism and action of thyroid hormones, that is, the emergence of resistance of the body to the action of thyroid hormones. If the patient's endocrine status is normal, then there will be no symptoms of the disease. As it develops and pathologies increase in the hormonal background, clinical symptoms of the disease will appear.
This form of hypothyroidism is dangerous due to various complications.
Patients with this diagnosis do not have pathology in the hypothalamic-pituitary system and the thyroid gland. The mechanism of occurrence of this form of the disease has not yet been fully studied.
Hypothyroid coma
This is an unconscious state characterized by:
- A pronounced decrease in all types of metabolism.
- Loss of consciousness.
- Persistent hypothermia (decrease in body temperature below 35 degrees).
- Decreased or loss of reflexes.
- Bradycardia (heart rate less than 60 beats/min.)
A decisive role in the development of a coma is played by a sharp decrease in the flow of thyroid hormones into the blood. Most often, such a complication appears against the background of a long, severe course of the disease, especially in elderly patients.
There are no specific key factors leading to the development of coma. We can only note that such a condition develops against the background of:
- Acute infections (pneumonia, sepsis).
- Diseases of the cardiovascular system (heart failure, myocardial infarction).
- Surgical interventions.
- Food intoxication and many other factors.
Causes
Provoking factors
It is known that women are more likely to suffer from hypothyroidism. A severe life-threatening condition is hypothyroid coma, which develops in elderly people who do not receive replacement therapy for long-term severe hypothyroidism when exposed to a number of provoking factors. These factors include:
- severe somatic diseases (heart attacks, strokes);
- hypothermia of the body;
- infectious diseases;
- heart failure;
- injuries of various locations;
- the occurrence of gastrointestinal bleeding;
- taking alcohol or drugs that depress the function of the central nervous system (anaesthetics, tranquilizers, antipsychotics, opioids).
At the same time, in the process of physiological aging of the human body, all metabolic processes slowly fade away, which leads to the formation of various pathologies. Hypothyroidism is one of the most common pathologies of older people, occurring in 2% of cases of examination of such patients and 6 times more often if it were possible to further examine everyone who does not seek medical help.
The disease in older people occurs due to dysfunction of the thyroid gland or regulatory systems - the pituitary gland or hypothalamus. With the disease, the metabolic rate decreases, cells begin to consume significantly less oxygen, the connective tissue elements of internal organs accumulate glycosaminoglycans, and the normal production of energy-dependent cell enzymes, which help organs to function fully, is disrupted.
Congenital hypothyroidism
The disease is based on a complete or partial deficiency of thyroid hormones produced by the thyroid gland, which leads to a delay in the development of all organs and systems. First of all, the central nervous system suffers from a lack of thyroid hormones. A direct connection has been established between the age at which treatment was started and the index of the child’s intellectual development in the future. As well as the manifestation of trophic disorders of the skin, depression of cardiac function, and a reduced level of metabolic processes.
Most often, congenital hypothyroidism is primary. It occurs as a result of abnormal development of the fetal thyroid gland - dystopia, athyroidism, hypoplasia.
The causes of such anomalies can be infectious and autoimmune diseases of the mother, taking toxic medications during pregnancy, contact with chemicals, radiation, iodine deficiency during pregnancy. Sometimes, no more than 2% of all cases of congenital hypothyroidism, the disease can be inherited due to gene mutations. Hereditary forms are most often accompanied by other pathologies - cleft palate, cleft lip, congenital heart defects, kidney defects and others.
Up to 10% of all children with this pathology experience a violation of the synthesis, secretion or interaction of thyroid hormones with each other. Up to 5% of all cases of congenital hypothyroidism have secondary and tertiary forms. They arise due to abnormalities in the formation of the fetal brain, due to cysts, tumors, birth injuries, asphyxia or pituitary aplasia.
Acquired hypothyroidism
Acquired hypothyroidism can occur for the following reasons:
- radiation or radiation irradiation of the neck;
- thyroid surgery (removal of this organ);
- inflammation in the thyroid gland;
- use of radioactive iodine as a medicine;
- use of certain medications.
In this case, the secondary form of hypothyroidism can occur with diseases of the hypothalamus or pituitary gland, which provoke a decrease in the functionality of the endocrine glands.
Medicines as a cause of disease
As noted above, acquired hypothyroidism can also occur when certain medications are used to treat any pathologies. Such drugs include drugs based on adrenal hormones, lithium-containing drugs, iodides, beta-blockers, some antiarrhythmic drugs, drugs with large dosages of vitamin A. All these drugs can cause hypothyroidism, so their prescription and monitoring of use is always in the field of management of specialized doctors.
Psychosomatic causes of the disease
Medical psychology has its own explanation for the occurrence of each disease in the body. These reasons are based on psychological factors and problems of a particular patient.
Experts associate the development of hypothyroidism with the fact that the thyroid gland itself has the shape of a shield and is located in the human neck.
This indicates the key protective role of both the gland itself and the hormones it produces. In the case of hypothyroidism, psychologists say that the patient strives to express and perform more actions, but suppresses his own desires and tries not to demonstrate increasing needs.
Fear of action is caused by lack of confidence in one's own abilities. A person is only sure that all his endeavors will fail, and he does not have enough strength and agility to achieve success. A patient with hypothyroidism is distinguished by the fact that psychologically he completely loses the relationship with his own creativity.
Diet for hypothyroidism of the thyroid gland
- Fatty, spicy foods and easily digestible carbohydrates are excluded from the menu.
- The diet must be diversified with protein foods, as they serve as a source of energy and vitality.
- The menu for thyroid hypothyroidism should be supplemented with vitamins, fresh vegetables and fruits that do not contain large amounts of sugar.
- Products that should not be consumed include: mushrooms, legumes, honey, jam, tea, coffee, cocoa, carbonated drinks, smoked foods.
Products for thyroid hypothyroidism that are recommended to be eaten: eggs, low-fat cheeses and dairy products, crackers, dried bread, dry cookies, cereals, seafood, low-fat fish, fresh vegetables and fruits.
If you follow all the specialist’s recommendations and follow a diet, a disease that was detected in a timely manner can be almost completely cured. In this case, the prognosis is favorable, the presence of complications is excluded. In some cases, the prescribed treatment must be taken for the rest of life. The congenital form often has an unfavorable prognosis due to impaired formation of the musculoskeletal system and disruption of the central nervous system and brain.
To prevent the development of severe thyroid disease, it is necessary to follow preventive recommendations.
Symptoms of pathology
Experts include the main symptoms of hypothyroidism:
- depressive and apathetic states, fatigue, weakness, insomnia, loss of concentration;
- complete intolerance to cold by the body, increased dry skin, hyperkeratosis of the knees and elbows, hair loss and brittle nail plates;
- arthralgia, muscle weakness, paresthesia, excessive weight gain;
- severe swelling of the limbs and face due to water-salt imbalance, anemia, bleeding;
- prerequisites for the occurrence of atherosclerosis (high cholesterol levels), interruptions in lipid metabolism;
- development of secondary diabetes mellitus, impaired glucose tolerance, decreased appetite, constipation, gas;
- disruption of the menstrual cycle in women, including infertility and amenorrhea;
- bradycardia, arrhythmia, angina pectoris.
All symptoms can be either single or widespread. Their occurrence may indicate the development of the disease, therefore, with the complex of the above characteristics, it is extremely important to seek medical help.
Degrees of severity and development of the primary type
Subclinical form or compensated hypothyroidism
Subclinical hypothyroidism (the same as the compensated form of hypothyroidism) characterizes a condition when the disease is hidden and does not manifest itself in any way. A similar diagnosis can be made based on the results of blood tests for thyroid hormones and the pituitary hormone thyrotropin, the level of which should be elevated in the case of this form of the disease. Reduced activity of the thyroid gland leads to a similar hormonal surge of thyroid-stimulating hormone, with which the pituitary gland signals it about the lack of iodine concentration in the body.
A subclinical form of the disease affects 8% of the entire population of the planet, mainly women during menopause, that is, after 50 years.
A subclinical form can also occur during frequent stressful conditions in the body, when the concentration of cortisol in the blood increases, which suppresses the production of iodine-containing hormones. Also in women, this disease can be the result of the use of oral contraceptives, which contain a lot of estrogen. The subclinical form can occur in the presence of chronic diseases of the patient and the patient is taking medications, which, together with the existing comorbid background, led to the development of subclinical hypothyroidism.
In the initial stages, the subclinical form can not be treated, but the concentration of hormones can be adjusted with proper nutrition and lifestyle. However, most often this pathology is diagnosed in patients only when it has already become manifest and requires immediate hormone replacement therapy.
Decompensated hypothyroidism
Decompensated hypothyroidism is understood as that form of the disease in which all the clinical symptoms of the disease are clearly expressed and the examination clearly shows a lack of thyroid hormones. To treat this disease, hormone therapy is used with a dosage of active ingredients depending on the stage of decompensation. The stage of decompensation is determined by the patient’s well-being, the severity of symptoms and hormonal levels.
In parallel with the decompensated form of hypothyroidism, it is often necessary to treat concomitant diseases that arise due to a lack of thyroid hormones. Most often this is manifested by anemia, cholesterol metabolism disorders are present, and liver and heart function are impaired.
Those patients suffer from a decompensated form in whom the subclinical form of the disease was not identified in a timely manner, or with serious complications due to infectious, oncological and other processes in the body.
Manifest form
With this form of hypothyroidism, timely early diagnosis is important, since this pathology can lead to severe degrees of hypothyroidism and heart disease, which are a consequence of hypofunction of the thyroid gland.
Manifest hypothyroidism is divided into two stages of the disease. During the compensation stage, the body is able to cope with the lack of hormones on its own, and its symptoms are extremely rare and mildly expressed. The decompensated stage of manifest hypothyroidism has clear manifestations in the form of severe symptoms; it can constantly progress, leading to serious health consequences and even death.
Complicated course
Complicated hypothyroidism is quite severe and is usually accompanied by pathologies such as cretinism, secondary pituitary adenoma, serious heart rhythm disturbances, myxedema coma and death.
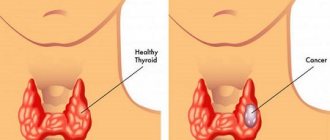
Female and male complications of severe hypothyroidism may vary slightly; in women, this pathology is most often accompanied by constant galactorrhea, changes in the structure of the mammary gland, infertility, severe heart failure, and hypothyroid coma with a fatal outcome in 80% of cases. In men, as complications of severe hypothyroidism, the thyroid gland may grow in volume and form a secondary adenoma. People of both sexes are often diagnosed with thyroid cancer, patients often lose consciousness, and death is not excluded for anyone, but it happens more often in women.
Stages
The clinical picture depends on the severity of the patient's hypothyroidism. The symptoms listed above do not occur all at once. At the initial stages, damage to the body and its organ systems is moderate and quite easy to treat. In advanced forms, irreversible and dangerous complications can occur.
There are 3 degrees of severity of hypothyroidism:
- Mild (the patient becomes sluggish, thinking is impaired, intellectual potential is reduced, heart rate is reduced; performance remains within normal limits);
- Moderate (bradycardia is noted, the patient’s skin is dry, he complains of constipation, drowsiness, irritability for no reason; women experience uterine bleeding; performance is moderately reduced; a general blood test reveals anemia);
- Heavy. Severe damage to organ systems occurs. Often the consequences cannot be treated. Kidney and heart failure, infertility, polycystic ovary syndrome, myxedematous coma develop, and deaths are known.
The disease may not manifest itself for a long time. This is due to the fact that the process develops gradually. In mild to moderate degrees of the disease, the patient’s well-being may be satisfactory, and erased symptoms are considered to be depression, overwork, or pregnancy (if present).
Diagnostic methods
Thyroid-stimulating hormone (TSH) analysis
The main test to suspect the presence of hypothyroidism is to determine the level of thyroid-stimulating hormone in the blood serum. The TSH norm is 0.4-4.0 µU/ml. When TSH rises, the synthesis of thyroid hormones decreases, and the pituitary gland is forced to produce more hormones to stimulate thyroid function.
If the TSH level is low, this indicates that the pituitary gland is not producing an additional dose of its hormones, since the thyroid gland is already actively functioning. This situation can, however, be observed in a number of cases - during pregnancy, in the case of pathologies of the pituitary gland, in certain diseases. It is important to understand that there is a feedback relationship between TSH and thyroid hormones, which is designed to maintain the body’s basic metabolism.
In the case of newborns and the possibility of asymptomatic hypothyroidism, each infant is examined for congenital hypothyroidism on days 5-7 of life. If the TSH value is elevated, babies undergo a routine ultrasound, since in this situation the presence of pathology is already suspected.
Ultrasound diagnostics
If a doctor suspects that a patient has hypothyroidism, a routine ultrasound examination is recommended as an additional study to determine the possible cause of hypothyroidism or to assess the total mass of the thyroid gland. The data do not always reflect hypothyroidism in the presence of altered levels of thyroid hormones. However, ultrasound is always part of the diagnostic procedures when making this diagnosis. Ultrasound for hypothyroidism can detect signs of autoimmune thyroiditis, which is often what causes it. Local or extensive thickening of the thyroid gland is observed. It can be either increased - with hypertrophy, or decreased - with atrophy. If the patient shows only nodularity on ultrasound, and there are no other symptoms of hypothyroidism, then the diagnosis is not made. An assessment of the clinical picture and laboratory data of thyroid hormones is required.
Differential diagnosis
Making such a complex diagnosis as hypothyroidism requires differential diagnosis, since the symptoms of the disease are also characteristic of many other pathologies in the body. In this case, it is important to pay attention to the leading clinical symptom inherent in a particular disease. Based on these symptoms, it is important to differentiate hypothyroidism from the following pathologies with a similar clinical picture:
- chronic ischemic heart disease, complicated by circulatory failure, in which, as with hypothyroidism, swelling of the subcutaneous tissue, shortness of breath, inversion of the T wave, hypercholesterolemia may be observed, but unlike the pathology under consideration, a rapid heart rate will be observed here, and not bradycardia, on in edema there will be a trace of pressure due to poor blood circulation;
- chronic kidney disease, which arises from various kidney diseases, in which, by analogy with hypothyroidism, swelling of the limbs and puffiness of the face, anemia, pale skin, but there will be no amyia and lethargy, arterial hypotension, and there will be signs of uremia in the blood;
- anemia, which is similar to hypothyroidism in pallor, lack of red blood cells and hemoglobin in a blood test, but differs from it in the absence of psychomotor retardation, rigidity to antianemic drugs, and bradycardia;
- differential diagnosis is also carried out with the following diseases: hepatitis, polyserositis, polyarthritis, depression, dyskinesia of the gastrointestinal tract.
Hypothyroidism Treatment Methods
Medical products (drugs, medicines, vitamins, medicines) are mentioned for informational purposes. We do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
Traditional methods
The goal of hypothyroidism therapy is clinical remission and laboratory compensation of hypothyroidism. Hormone replacement therapy is used to treat hypothyroidism of any etiology.
Replacement therapy is usually carried out using the drug Levothyroxine. This remedy is excellent for subclinical hypothyroidism for pregnant women or those women who are planning a future pregnancy. If hypothyroidism is secondary, there is a need to monitor thyroxine levels. Depending on its level, hormonal therapy is prescribed in the appropriate dosage.
In complex pathologies, hypothyroid coma can develop, which is often a consequence of improper treatment. Also, such a coma occurs due to injuries, hypothermia, intoxication processes, acute viral and infectious diseases. In this case, in addition to thyroid hormones, glucocorticoids and medications are prescribed to correct electrolyte and hemodynamic disorders.
ethnoscience
There is no non-drug treatment for hypothyroidism. As an auxiliary therapy, some methods of alternative treatment for hypothyroidism can be used. For example, given that this pathology reduces digestive function, you should choose a low-calorie diet, completely eliminate fatty meats, and introduce fresh fruits, vegetables, and a lot of seafood into your diet.
Traditional recipes can also be used to correct the functioning of the thyroid gland.
For this purpose, special recipes are used:
- A drink is prepared from vegetables. For it, potato, beet and carrot juices are mixed in equal proportions, and then this mixture is taken 50 milliliters three times a day before meals.
- As a natural source of iodine, you can eat 1 kilogram of cucumbers every day.
- To replenish Omega-3 fatty acids in the body, you need to consume fish oil.
- To adjust the functioning of the gastrointestinal tract, you can take 1 teaspoon per day of flaxseed oil on an empty stomach.
- To normalize the level of thyroxine and the entire complex of thyroid hormones, it is recommended to eat white cinquefoil.
- To overcome hypothyroidism, you need to use a decoction of elecampane root, birch buds, St. John's wort and rowan fruits, which are taken in equal proportions, poured with a liter of boiling water and brewed over low heat for 5 minutes. Then the decoction is infused for 12 hours and consumed three times a day before meals.
- Beetroot tincture also works effectively, for which freshly squeezed juice of this root vegetable is mixed with a glass of vodka and infused for 2 weeks in a closed container. The finished infusion is taken 2 tablespoons, which must be washed down with clean water, 3 times a day.
Folk remedies
The use of folk remedies for hypothyroidism is possible only after consulting an endocrinologist.
- 1. white cinquefoil root (100 grams)
thoroughly. Pour 0.5 liters of vodka, seal tightly and leave in a dark, warm place for 10 days. Then strain the infused root through cheesecloth. Take as follows: three times a day, 1 tbsp. 30 minutes before meals for 30 days. - 2. Pour the zest of 1 lemon
into a liter of boiling water. Add 1 tbsp. honey and linseed oil. Soak for 10 minutes in a water bath. Cool, strain, dilute with water until the original volume is obtained. Drink during the day. - 3. Angelica root, licorice, Rhodiola rosea, rose hips, celandine, St. John's wort and fucus leaves
should be crushed and mixed. Each ingredient must be taken in the same quantity. Three tablespoons of the herbal mixture must be brewed in 0.5 liters of hot water, put on fire and brought to a boil. Leave for four hours, then strain using cheesecloth or a sieve. 4 times a day after meals you need to drink a teaspoon of decoction.
Prevention of hypothyroidism
Preventive measures in case of the threat of acquired hypothyroidism involve early diagnosis, timely initiation of replacement therapy, as well as the use of iodine as additional medications for the prevention of iodine deficiency or nutrition with sufficient iodine intake.
It is impossible to completely prevent the development of hypothyroidism, however, knowing the possible causes and risk factors for secondary hypothyroidism, as well as endocrinological heredity, this disease can be identified at an early stage and timely therapy can begin.
When considering family history, diseases of immediate family members deserve special attention, such as adrenal disease, diabetes mellitus, pernicious anemia, and diseases and conditions of the thyroid gland.
The patient’s laboratory tests deserve close attention from the endocrinologist to prevent the development of hypothyroidism if they reveal:
- hyponatremia (low sodium levels);
- dyslipidemia (impaired fat metabolism);
- increased levels of lactate dehydrogenase, creatine phosphokinase, prolactin.
An ultrasound examination of the thyroid gland will help to see structural changes in this organ and inflammatory processes in it, which can serve as prerequisites for the development of hypothyroidism.
Non-specific measures to prevent the disease include a balance of work and rest regimes, combating physical inactivity, maintaining an active lifestyle, long and sound sleep at night, maximizing positive emotions, which will stabilize higher nervous activity. It is also very important to eat right, not to go on starvation diets, and to consume large amounts of various microelements necessary for stable thyroid function.
You'll have to get used to it, or a little about prevention
If you have hypothyroidism, you need to reconsider the rhythm of your life, improve your sleep at night, and avoid stressful situations. Light physical exercise, being in the fresh air, and the ability to relax will help.
Far from the last place is now given to the menu. Food should only be easily digestible and fortified.
Try to live completely without eating animal fat and light carbohydrates - limit sweets and flour products to a minimum.
Eat spinach, beets, lettuce, and seaweed. In general, everything related to the sea is rich in essential microelements - fish, algae, etc.
We should not forget about preventive iodine intake, especially for people at risk for hypothyroidism.
Food supplements with a high iodine content will help with this. If possible, replace regular salt with iodized salt. But remember, when stored, its iodine does not lose its properties for 9 - 12 months.
Duration of illness
Temporary or transient (reversible) forms of hypothyroidism are observed in cases of prematurity, intrauterine growth retardation, functional immaturity, intrauterine infections, and in children from mothers with thyroid pathology. With age, the function of the thyroid gland in such children is restored, hormones begin to be produced in sufficient quantities and there is no need for treatment. To confirm this, a special analysis is carried out. To implement this, L-thyroxine is no longer administered to the patient for up to a month and a half, and after that a test for hormonal concentrations is done. If the test results are good, a conclusion is drawn about the transitional nature of the pathology. In this case, the child is stopped taking hormones. If the tests do not confirm the transitory form of the disease, then L-thyroxine must be used by the patient for life.
Hypothyroidism, which occurs during pregnancy in women, can also be completely cured. After giving birth for 6 months, there is a high probability that the thyroid gland will completely resume its functions on its own.
Other forms of hypothyroidism cannot be completely cured; they can only be brought to the stage of compensation and try to maintain in this form for a long time. When the disease passes into a decompensated form, treatment should be reviewed to prevent complications.
Clinical manifestations of the disease
The disease is characterized by the presence of two forms, or periods. The first one is hidden. It can be asymptomatic or with general symptoms. These include weakness, malaise, lethargy, sleep disturbance, memory loss, and sudden mood swings. During this period, body temperature may rise for no reason. Such manifestations are often associated with a common cold or overwork.
The obvious period is distinguished by clearer manifestations. One of the first symptoms to occur is weakness and brittleness of hair and nails. The skin becomes pale and dry, and painful cracks may appear. Immunity decreases, colds become more frequent, and hemoglobin may drop. Disturbances in the functioning of the cardiovascular system are observed: decreased blood pressure, noticeable interruptions in heart rate, shortness of breath, swelling, pain during exercise. A disorder of the gastrointestinal tract occurs: appetite decreases, nausea appears, the liver enlarges, and there is a tendency to constipation. Signs of thyroid hypothyroidism in women - the menstrual cycle is disrupted or disappears, and the inability to get pregnant. In males, there is no sexual desire and potency decreases.
The severity of the course and the degree of obviousness of the manifestations depend on the reasons that caused the development of the pathology and the body’s defenses. There are three classes of disease severity.
| Gravity class | Characteristic |
| Lightweight | Fatigue and decreased mental activity appear. Bradycardia and decreased blood pressure may be observed. The patient is able to work and is still active. |
| Average | Bradycardia, pallor, dry skin. There is a sharp change in mood, constipation. Efficiency decreases, hemoglobin drops. |
| Heavy | Symptoms increase, damage to body systems appears, and can often be irreversible. Kidney, heart, and liver failure appears. In extreme cases, death. |
To avoid irreversible consequences, it is necessary to consult an endocrinologist when the first tangible signs of a change in well-being appear. To identify pathological conditions of the thyroid gland, a specialist prescribes a series of examinations.
Pregnancy and breastfeeding
Hypothyroidism is a relatively common pathology among women of reproductive age and pregnant women, which is often diagnosed accidentally due to nonspecific clinical signs of the syndrome and the lack of strict recommendations for screening hypothyroidism and women of reproductive age and pregnant women. Often in the case of manifest and subclinical hypothyroidism, women experience menstrual irregularities and even infertility. This is due to the fact that increased thyroid-stimulating hormone also entails an increase in prolactin, which can inhibit the maturation of oocytes in the ovarian region. In this case, ovulation does not occur during the menstrual cycle and the woman cannot become pregnant.
With hormonal imbalance, the formation of the endometrium, the tone of the fallopian tubes and the components of the cervical secretion are disrupted. A mature egg under such conditions becomes unable to carry out fertilization and does not attach to the fallopian tubes.
In order to understand whether pregnancy with hypothyroidism is possible in each specific case, it is important to promptly seek medical help and undergo a course of effective treatment. If a woman does not know about her own pathology, this can also negatively affect sudden pregnancy, which can still occur even with hypothyroidism. Therefore, before planning a conception, it is better to be fully examined so that you do not have to sacrifice your own health and the life of the unborn child when treating hormonal changes.
Effect on the fetus
Hypothyroidism of any severity can cause a number of severe complications in both the mother and the fetus, manifested in miscarriage, early termination of pregnancy, intrauterine fetal death, and frozen pregnancy.
A woman who does not know her diagnosis can discover the presence of problems with the endocrine system if she systematically experiences involuntary abortions. Miscarriage serves as a signal of even the mildest stage of subclinical hypothyroidism.
At the end of pregnancy, with this diagnosis, a new danger arises for the fetus and mother - post-term pregnancy up to 42 weeks. For a child, this is fraught with all sorts of birth injuries and disruptions in the functioning of the nervous system. Thus, the presence of hypothyroidism in a pregnant woman is an absolute indication for the immediate initiation of replacement therapy, which is prescribed immediately and in full dose, without the preliminary gradual increase adopted in some cases of treatment of hypothyroidism outside pregnancy
Is it possible to give birth
Childbirth with compensated hypothyroidism is usually carried out naturally, but preliminary preparation for it is necessary. Indications for delivery by cesarean section usually arise in the presence of serious obstetric complications. Hypothyroidism itself does not complicate childbirth if hormone levels are stabilized.
Is it possible to breastfeed
Hypothyroidism also negatively affects the condition and health of the mammary glands in women. However, when treating this pathology with medications, breastfeeding is quite acceptable. Breastfeeding is also acceptable if there is a frequent complication of the pathological condition in the postpartum period - diffuse enlargement of the thyroid gland (goiter) and its drug therapy.
To reduce the likelihood of endocrine disorders in the body during pregnancy and the lactation period, it is necessary to carry out iodine prophylaxis of the body. Only pathological hypothyroidism does not accept iodine prophylaxis, so it cannot be carried out in this case.
If thyroid pathology is detected in a timely manner, then you can become pregnant and breastfeed a child, since this pathological process may have a physiological basis that will not negatively affect pregnancy and breastfeeding.
How dangerous is this disease?
The negative consequences in patients with hypothyroidism are very different. All of them are dangerous, so their occurrence should be prevented. The consequences of hypothyroidism vary depending on the age of the patient. So, in children the main consequences of pathology can be:
- slow mental and physical development, development of cretinism, infantilism;
- absence of secondary sexual characteristics for a long period;
- heart diseases;
- low immune resistance of the body, frequent colds, the likelihood of numerous chronic diseases;
- increased weakness, inability to perform physical labor.
Among the consequences of hypothyroidism that adult patients often experience are:
- decreased cognitive abilities;
- cardiovascular diseases;
- long-term, often chronic, infectious diseases;
- menstruation disorders;
- ovarian atrophy, dysfunction of the mammary glands, infertility;
- change in the appearance of the external genitalia;
- impotence, sexual impotence.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
Also, in adult patients, such a severe consequence of the pathology in question may occur as hypothyroid coma, during the period of which the hormonal level of the body reaches a critical state. In this case, metabolism is disrupted, cardiac arrest and brain dysfunction are possible.
Recommendations for patients
If you experience complaints such as weakness, drowsiness, fatigue, memory loss, depressed mood, dry skin, brittle nails, active hair loss, moderate weight gain, chilliness, infertility, decreased potency, immediately contact an endocrinologist.
Children with developmental delays must be observed by an endocrinologist to study the function of the thyroid gland. Pregnant women should contact an endocrinologist to study thyroid function in the 1st and 3rd trimesters of pregnancy and after childbirth.
FAQ
Joining the army with hypothyroidism
The clinical picture of hypothyroidism can be hidden or obvious, however, in any form and stage of the disease, conscription into the army is not carried out if the hormonal balance is disturbed.
To obtain a military ID, a conscript must confirm his own illness. To do this, it is necessary to undergo an additional examination at the military commissariat, having previously submitted to the therapist at the military medical commission the documents accompanying the current disease, confirming the diagnosis. During an additional examination, the conscript will be prescribed an ultrasound examination and may be given a referral for a thyroid biopsy, blood tests for hormones, and other diagnostic procedures.
After such an examination, a doctor from the commission fills out a report and submits it to a meeting of the military commission. A conscript whose diagnosis is confirmed receives a military ID and is not called up for military service. Only a conscript whose diagnosis of hypothyroidism has been previously removed by the treating endocrinologist can be called up for service.