Cerebral edema is a disease in which the outflow of cerebrospinal fluid is obstructed. This leads to increased intracranial pressure and difficulty in supplying blood to the brain tissue. Necrosis develops. In the absence of timely treatment, the pathology causes death.
Causes of cerebral edema
Cerebral edema occurs against the background of various neurological and other pathological conditions:
- Encephalitis due to tick bites, as complications after influenza.
- Infectious factors: neurocysticercosis (parasitic brain damage), cerebral malaria or meningitis .
- Ischemic, hemorrhagic and embolic strokes.
- Hydrocephalus as a consequence of meningitis or trauma.
- Ischemic encephalopathy due to birth injuries, high blood pressure, atherosclerosis.
- Venous thrombosis of intracranial sinuses.
- Brain tumors.
Diseases that provoke cerebral edema include diabetic ketoacidosis, liver failure, and electrolyte imbalance. Symptoms of cerebral edema may not appear immediately.
Cerebral edema in children with hydrocephalus is associated with increased intracranial pressure.
Brain cancer, a person is drawn to sleep
The further the disease progresses, the longer the patient is prone to sleep. He sleeps constantly and his sleep time is rapidly increasing every day. Initially, symptoms can be controlled by using various strong steroids, which will discourage the desire to sleep. Problems begin with a person’s brain activity and he simply fades away. Every day his drowsiness increases, he constantly wants to sleep.
At this stage, patients can still lead a normal life and are able to enjoy life, but due to sleep they are unable to do so. Relatives should always cheer a person up and dissuade him from sleep and tell him that life needs to be lived.
Over time, it becomes more and more difficult to wake up a person with brain cancer. He simply leaves in front of his family and friends. The patient begins to forget a lot, get lost in space and become absent-minded. It’s hard to admit this, but on the eve of death it is simply impossible to talk to a person. He will not understand what is happening and simply will not remember who you are, and even if he remembers, he is unlikely to convey all the feelings that he feels for you.
Who's at risk
High-risk groups include people with severe diabetic ketoacidosis, as well as children who are experiencing acidosis for the first time. Factors that increase the likelihood of swelling are: dehydration, inflammation and blood clotting.
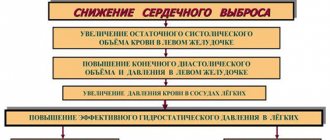
As a result, blood flow to the brain decreases and a cascade of ischemia and edema reactions occurs. Intracranial pressure increases, blood pressure and heart rate decrease. A brain herniation can compress vital structures in the brain stem. Patients with hyperactive ketoacidosis are at greater risk. High levels of ammonia above 200 µmol/L in the blood may be an indicator of the risk of developing intracranial hypertension.
In hepatic encephalopathy, cerebral edema is caused by a decrease in perfusion pressure in the brain vessels, swelling of astrocyte cells due to the accumulation of ammonia and increased glutamine production. Against the background of edema, intracranial pressure increases, ischemic contusion and brain hernia develop.
Often, cerebral edema develops in children who have suffered hypoxia and have hydrocephalus. Cerebral edema can complicate the course of strokes and traumatic brain injuries.
Therapeutic measures
Patients with symptoms that resemble cerebral edema should be urgently admitted to the intensive care unit, as they require constant monitoring of vital signs: pulse, blood pressure, oxygenation and osmolarity, etc.
The principles of treatment for cerebral edema are as follows:
- maintaining adequate breathing and functioning of the cardiovascular system;
- treatment aimed at correcting water and electrolyte balance and eliminating oxygen starvation of the brain;
- carrying out anticonvulsant therapy and normalizing body temperature;
- management of the disease that led to cerebral edema;
- fight against intracranial hypertension.
Patients who have developed cerebral edema require round-the-clock monitoring and specialized care. Therefore, at the first signs of severe neurological pathology, the patient should be hospitalized in a hospital with an intensive care unit.
Emergency help
Emergency care is provided in the intensive care unit; it is impossible to cope with cerebral edema at home. It includes correction of blood pressure, external respiration and gas exchange.
To do this, artificial ventilation of the lungs is carried out in the mode of moderate hyperventilation, which reduces the risk of developing acidosis, fights liquor hypertension and reduces intracranial blood volume.
To preserve the vital activity of neurons in conditions of cerebral edema, hypothermia is often used, that is, an artificial decrease in body temperature. This is necessary to reduce the rate of metabolic processes in the brain, protect it from prolonged hypoxia, and stabilize enzyme systems and cell membranes.
A negative aspect of using this type of treatment is the thickening of the blood and a decrease in the body's resistance to various infections.
To create craniocerebral or general hypothermia, the following methods are used:
- covering the patient with bags filled with ice;
- wrapping with wet cold sheets;
- fan blowing.
Hypothermia should be carried out under the condition of blocking the protective mechanisms that are activated when body temperature decreases (shivering, increased metabolism, vasospasm, arrhythmia). For this, the patient is administered neuroleptics (aminazine, chlorpromazine hydrochloride, tizercin).
Dehydration therapy
The main method of treating cerebral edema remains dehydration therapy, which consists of the use of the following groups of drugs:
- Osmodiuretics. These include mannitol, sorbitol and glycerol. Their action is to increase diuresis due to an increase in blood plasma osmolarity. In this case, fluid from the intercellular space and brain cells is directed back into the vessels. Among these drugs, mannitol is considered the most effective.
It has the greatest diuretic effect, does not disrupt metabolic processes, weakly penetrates the blood-brain barrier and does not have a toxic effect on the body. All osmotic diuretics are good for short-term control of intracranial hypertension. Since with prolonged excess intake they lead to disruption of the water-electrolyte balance and the development of re-edema.
Also, when the infusion of these drugs is stopped, a “rebound” phenomenon often occurs due to their penetration into the interstitial space of the brain when the blood-brain barrier is damaged, followed by fluid accumulation. This side effect is prevented by intravenous administration of albumin solution;
- saluretics, or loop diuretics (furosemide, lasix, torasemide, hypochlorothiazide, clopamide, ethacrynic acid, uregit), the action of which is aimed at inhibiting the reabsorption of sodium and chlorine ions in the renal tubules. This group of drugs is used due to their lightning-fast effect.
But they can cause blood thickening and a decrease in potassium and sodium levels in the plasma. Therefore, saluretics are used to consolidate the action of mannitol and stop the “recoil” phenomenon;
- corticosteroids. The use of these drugs is due to their ability to stabilize the vascular membrane, reducing its permeability, and also restore normal blood circulation in the area of edema. Therapy with corticosteroids (dexamethasone, hydrocortisone, prednisolone hemisuccinate) begins from the first hours of the onset of pathology and continues for about a week. Vasogenic cerebral edema is most sensitive to their action, and cytotoxic is the least sensitive.
Against the background of active dehydration therapy, it is necessary to maintain a normal water-electrolyte balance, which is achieved by infusion of isotonic sodium chloride solution, hypertonic glucose solution (10%) with the addition of potassium chloride, Ringer's solution, etc.
Improving brain tissue metabolism
In order to improve blood supply and metabolic processes in the brain, the following is used:
- vascular agents (pentoxifylline, trental, nicotinic acid, vinpocetine, cavinton);
- protease inhibitors (gordox, contrical);
- membrane and angioprotectors (troxevasin, ascorutin, dicinone);
- neuroprotectors (ceraxon, neuroxon, pharmacoxon, somaxon, pantogam);
- metabolic drugs (Cerebrolysin, Cerebrolysate, Cortekin, Actovegin);
- gamma-aminobutyric acid preparations (aminalon).
Elimination of accompanying symptoms
To relieve convulsive syndrome, anticonvulsants (carbamazepine, lamotrigine, valprocom) and sedatives (diazepam, phenobarbital, Relanium) are used. Vomiting and nausea are combated by administering metoclopramide (Cerucal).
It is also necessary to stop the disease that caused the swelling as soon as possible, otherwise it will recur. Thus, in case of large brain tumors, they are removed, in case of poisoning, detoxification therapy is carried out, etc.
To prevent infectious complications, broad-spectrum antibiotics are administered that are able to penetrate the blood-brain barrier (for example, ceftriaxone, cefepime, cefuroxime).
Pathogenesis
Brain swelling is a stepwise process in which acute injury results in the formation of cytotoxic, ionic, or vasogenic edema. What is edema? This is a combination of pathogenetic mechanisms. Cytotoxic edema is characterized by depletion of intracellular adenosine triphosphate (ATP), which impairs the active transport of osmolytes across cell membranes. Sodium and water ions accumulate in cells.
On the surface of cell membranes, the pressure and ratio of ions are disrupted, which leads to the movement of fluid into the extracellular space of the brain parenchyma from the vessels. This mechanism is also called ionic. During brain contusions, the activity of the Sur1-Trpm4 ion channel in endothelial cells increases, which leads to fluid accumulation.
A separate form of cytotoxic edema is vasogenic. The pathology develops due to increased permeability of the blood-brain barrier of the brain after a bruise, the release of inflammatory substances during infection and an increase in free radicals. As a result, fluid is released outside the cell along with blood plasma proteins.
As brain contusion develops, these mechanisms replace and complement each other, leading to swelling. It is believed that edema is preceded by an increase in intracranial pressure due to the fixed volume of the closed cranial cavity. At the same time, capillary perfusion - blood pressure in the vessels of the brain - decreases. The tissues do not receive enough nutrients and oxygen, and hypoxemia develops.
Complications and prognosis
Therapy for cerebral swelling is based on preventing relapses and restoring the activity of the hemispheres and nerve plexuses. The prognosis of treatment depends on the severity of the pathology and the qualifications of the doctor. When therapy is started on time, the outcome is favorable.
At the initial stage, cerebral edema is completely curable; when the disease is detected at the last, third stage, the death of nerve fibers and destruction of the myelin sheath of neurons is recorded.
Note! Complete elimination of swelling without the development of complications is possible only in young people with a toxic form of the pathology.
Self-relief of painful symptoms is observed with mountain edema. In many cases, death is diagnosed from cerebral edema. Survivors experience residual effects in the form of headaches, decreased intellectual abilities, neurological disorders, and disability.
The functions of dead brain cells can be performed by nearby areas of the brain after a long period.
Therefore, it takes a long time for a person who has suffered a stroke to re-acquire speech and movement skills.
One of the common consequences of cerebral swelling is cerebral edema-swelling (CEBS). Symptoms of this complication in adults include vomiting, headaches, and hallucinatory syndrome. As ONGM progresses, a person falls into a comatose state, and death is often recorded.
Classification
Brain edema occurs due to increased cerebral fluid content. In the pathogenesis of edema development, three forms are conventionally divided: cytotoxic, vasogenic and interstitial, or a combination thereof.
Vasogenic edema
Vasogenic edema is the most common form caused by disruption of the blood-brain barrier. Plasma proteins penetrate beyond the blood vessels, causing osmotic pressure to force fluid into the interstitial space of the brain. For example, endothelial growth factor, glutamate and leukotrienes locally increase the permeability of cells around the tumor. It is this, along with the weakness of the vascular walls, that leads to the entry of fluid with proteins into the parenchyma of the white matter. Swelling near tumors in 65% leads to cognitive impairment in patients due to displacement of brain structures.
Vasogenic edema is provoked by impaired vascular permeability and changes in perfusion pressure against the background of the following diseases and conditions:
- brain abscess;
- stroke;
- hypercapnia;
- encephalopathy due to hypertension;
- hepatic encephalopathy;
- metabolic disorders;
- diabetic ketoacidosis;
- lead poisoning;
- mountain sickness
Pathogenic microorganisms in meningitis disrupt the permeability of the blood-brain barrier to proteins and sodium ions. This leads to the accumulation of fluid in the intercellular space, as well as cell swelling due to passive hypoxia. Increased intracranial pressure disrupts connections between neurons.
Cytotoxic edema
Cellular or cytotoxic edema occurs within cells without damage to the blood-brain barrier. Pathology develops after a stroke or traumatic brain injury with damage to glial tissue, neurons and endothelial cells. The hemostatic mechanism in the cells is disrupted, and sodium accumulates in them, and the release of ions outside the membrane is disrupted. Anions try to restore neutrality on the surface of the membrane, which leads to swelling inside the cell.
Cytotoxic is associated with a change in the ion balance on the surface of cell membranes as a result of several reasons:
- hypoxic ischemic brain injury (drowning, cardiac arrest);
- brain injury;
- metabolic disorders of organic acid metabolism;
- hepatic encephalopathy;
- Reye's syndrome (acute liver failure);
- infections (encephalitis and meningitis);
- diabetic ketoacidosis;
- intoxication (aspirin, ethylene glycol, methanol);
- hyponatremia, or excess water intake without electrolytes.
Interstitial edema
One of the main causes of interstitial edema is obstructive hydrocephalus. Interstitial edema develops due to the leakage of cerebrospinal fluid from the ventricles of the brain into the interstitial space of the brain. Patients with hydrocephalus or meningitis are predisposed to this pathology. Increased pressure in the ventricles causes the contents of the ventricles to be forced out, resulting in swelling of the white matter.
First aid
We can do little on our own. You need to call an ambulance. While the brigade is driving, it’s worth following a simple algorithm:
- Lay down or make the patient sit. Under no circumstances should blood rush to the head. Therefore, find the optimal position for the victim.
- Provide fresh air. Open a window or window.
- Create conditions of complete peace. No noise, no intense light irritation. Nothing that could lead to the release of excess hormones.
- Carefully monitor your breathing, the condition of your pupils, and your heart activity. If this is possible, then also blood pressure.
What do doctors do after they arrive on site? First, conditions are provided to transport the patient to the hospital.
Several types of drugs are used:
- Osmotic diuretics. The favorite of this type is Mannitol. The concentration is selected individually.
- Electrolytic solutions to restore basic functions of the central nervous system and heart.
- Hormones, corticosteroids. Prednisolone, Dexamethasone, Hydrocortisone in individual quantities. These medications reduce the permeability of the blood-brain barrier.
- Psychomotor agitation is almost always present. It is eliminated with tranquilizers. For example, Diazepam.
- Cerebrovascular drugs. Another option is Piracetam.
Also other means at the discretion of the paramedic or doctor. Next, you need to transport the patient to a hospital. It is important to restore all body functions. This cannot be achieved in an outpatient setting.
Symptoms of cerebral edema
Cerebral edema, depending on the degree of changes, can be asymptomatic or symptomatic. The severity of the manifestations depends on the age of the person. In children, edema is compensated by the presence of fontanelles, and therefore the symptoms are different.
Cerebral edema has various manifestations:
- changes in consciousness, including coma;
- headaches and migraines;
- epilepsy;
- intoxication;
- intestinal obstruction (volvulus, intussusception)
- optic neuritis;
- hypertrophic pyloric stenosis
- macrocephaly.
General cerebral symptoms are associated with increased intracranial pressure:
- With a slow increase, patients experience morning headaches and vomiting without nausea, which is typical for brain tumors Transient dizziness occurs. Behavior changes slowly: patients become irritable and moody.
- With a rapid increase, the pain is paroxysmal, bursting, and severe. Vomiting does not provide relief. In patients, tendon reflexes increase, heartbeat and motor reactions slow down. Eye movements change, drowsiness sets in, speech and thinking are impaired.
With decompensation of increased intracranial pressure, coma develops, and with displacement of brain structures, breathing problems and heart contractions occur.
Symptoms
Symptoms of the pathological process increase gradually as intracranial pressure increases. Common signs of cervical edema in adults include:
- sharp pain in the head that cannot be relieved even with the help of strong antispasmodics;
- constant feeling of nausea;
- vomiting (does not depend on meals and does not bring even short-term relief);
- partial/complete loss of hearing and vision, a feeling of constriction in the eyeballs;
- shortness of breath;
- arrhythmia;
- the patient is poorly oriented in time and space, looks lost, is vaguely aware of real events;
- seizures;
- speech disorder;
- neurology – sleep disturbance, sensitivity, muscle tone, fainting, lack of appetite, tremors, etc.;
- visual hallucinations;
- cerebral palsy, paresis;
- loss of consciousness – as edema progresses, the frequency and duration of attacks increases; in severe cases, a person may fall into a coma.
If a patient exhibits signs of cerebral edema and his condition worsens every day, immediate correction of metabolic disorders is required.
Diagnosis of cerebral edema
Early diagnosis of cerebral edema reduces mortality and improves functional capacity of patients after ischemic stroke. When pathology is established, decompression trepanation is performed. An increase in cerebral edema can be determined by symptoms of increased intracranial pressure: increased episodes of loss of consciousness, nausea and vomiting, headache, blurred vision, and hemiparesis. Among the listed signs, it is the unconscious state associated with damage to the reticular activating system and the thalamic-hypothalamic-cortical axis that is considered the most important clinical parameter. The degree of consciousness impairment is measured using the Glasgow Coma Scale.
In hemorrhagic stroke, there are other criteria for assessing the risk of cerebral edema. The likelihood of an enlarged hematoma increases with its initial significant size, the use of anticoagulants, and the early onset of symptoms. The risk of edema increases with hyperglycemia, elevated blood pressure, large hematoma size, and increased cerebral perfusion pressure.
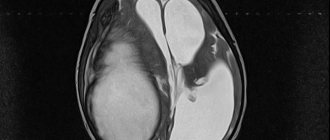
Swelling and dislocation of the brain during cerebral ischemia
CT picture - cerebral edema
Pathological anatomy
Frontal section of the cerebral hemispheres during swelling: an increase in the volume of the left hemisphere, blurring of the boundaries between the white and gray matter, collapse of the lateral ventricles, more pronounced on the side of the swelling (indicated by arrows).
Macroscopically, edema and swelling of the brain are characterized by a number of signs: moisture and turbidity of the surface, an increase in volume, increased flabbiness (water content) of the brain matter, which has a yellowish-pink color, and unclear boundaries between the gray and white matter (Fig.). Due to the general increase in the volume of the brain, deep depressions are found in the area of the cerebellar hemispheres and protrusion of its tonsils, which is a morphological sign of strangulation of the stem sections in the foramen of the tentorium of the cerebellum. However, differences in the signs of edema and swelling are also noted. With predominant edema, there is plethora and swelling of the soft membrane of the brain, and a clear liquid drains from the surface along with blood. There is an increased amount of cerebrospinal fluid in the ventricles of the brain. On sections, the brain substance appears to be excessively moist, it can be easily cut with a knife, and clear liquid flows from the cut surface. With predominant swelling of the structural elements of the brain, the soft meninges, on the contrary, are dry, the brain substance is dense, the knife sticks to the cut surface. In the ventricles of the brain, cerebrospinal fluid is absent or contained in small quantities; the ventricles are slit-like.
Features of the microscopic picture are determined by the presence in the medulla of interstructural spaces filled with interstitial fluid, which occupy up to 10-15% of the organ’s volume. Electron microscopic data on the gapless fit of the structural elements of brain tissue and the predominantly intraglial nature of cerebral edema require correction. The possibility of rupture of astrocytic processes overloaded with fluid is also recognized by some supporters of the intrastructural theory of edema. Increased hydration of brain tissue under light microscopy is manifested by its loosening, more or less widespread dystrophic changes in the neurons of the cortex and subcortical centers, as well as the walls of intracerebral vessels, swelling of the myelin sheaths of nerve fibers with the formation of balloon-shaped swellings, dystrophic and proliferative changes in astrocytic neuroglia with phenomena of disintegration of processes ( clasmatodendrosis), hydropic transformation of hyperplastic oligodendroglia (especially along the brain capillaries), sometimes activation of microglia.
When pathomorphol. diagnostics must take into account a complex of macro- and microscopic signs, as well as their relationship with each other. The presence of individual signs, for example, expansion of the perivascular spaces, does not yet indicate edema and swelling of the brain, since it may be a consequence of the redistribution of tissue fluid without increasing its quantity. Therefore, the common term “perivascular cerebral edema” is relative. One of the reliable indicators of edema and swelling is a violation of the specific density of brain tissue. Edema and swelling of the brain can be predominantly local (perifocal) or diffuse. The process usually involves both gray and white matter, but according to some researchers, it predominates in white matter. It is not possible to clearly identify areas of brain tissue that are particularly susceptible (or resistant) to edema and swelling.
Treatment of cerebral edema
The goal of intensive care is to maintain breathing and normal hemodynamic parameters. The patient's head is elevated at a height of 30 degrees for the outflow of venous blood. Early enteral nutrition is started.
The following therapy methods are used:
- artificial ventilation for symptoms of brain dislocation;
- hyperventilation subject to monitoring blood oxygen saturation levels;
- administration of hyperosmolar solutions;
- barbiturate coma;
- craniotomy;
- hypothermia (lower body temperature).
Treatment protocols for edema depend on its cause. With vasospasm, it is important to increase the volume of blood plasma, and with hyperemia, diuretics and hyperventilation.
Conservative methods
Osmotherapy is a basic drug therapy for cerebral edema. It is rarely used for prophylaxis due to limited effectiveness due to early use. Hyperosmolar agents create an intravascular osmotic gradient that facilitates water excretion. The most commonly used drugs are mannitol and hypertonic saline. The latter helps to expand intravascular volume, increase cardiac contractility and intracranial pressure.
Osmotic diuresis with mannitol can cause intravascular dehydration and hypotension, and after it it is necessary to ensure adequate fluid replacement with isotonic solutions. Prolonged repeated use of hypertonic saline will lead to the development of hyperchloremic metabolic acidosis. Therefore, the drugs are used as an alternative for the treatment of symptomatic cerebral edema.
Surgical methods
Surgical intervention avoids deaths in cases of extensive hemispheric strokes. Especially in patients under 60 years of age, if the procedure is performed within 48 hours of the onset of symptoms. Decompression surgery is performed at an early stage of edema development, bone with a diameter of at least 12 cm is removed. After decompression, doctors monitor the development of subdural hemorrhage, external hydrocephalus, and prevent wound infection and divergence of blood vessels.
Surgery is used to remove a mass that is causing swelling of the brain - an intracerebral hematoma, abscess or tumor. Hematomas in the cortex larger than 3 cm in size, as well as in the cerebellum area larger than 2 cm must be removed.
Features of the treatment of cytotoxic edema
Cytotoxic edema is treated with mannitol or another osmodiuretic. Mannitol is used in a dosage of 0.5-1 g per kilogram of body weight intravenously. The effectiveness of osmotic agents lasts for the first 48-72 hours. In case of cytotoxic edema, they try not to reduce blood pressure if the mechanisms of autoregulation are preserved. Solutions are administered intravenously to increase the volume of circulating blood, and vasopressor therapy is carried out. The approach is used while maintaining the blood-brain barrier. Barbiturate anesthesia reduces swelling. Sodium thiopental is administered to reduce intracranial pressure below 20 mmHg. Art.
Features of the treatment of vasogenic edema
Vasogenic edema requires the use of angioprotective drugs. Escinulisinate restores the tone of vascular walls, enhances reabsorption and reduces interstitial edema. For vasogenic edema, glucocorticoids are used to reduce the permeability of the blood-brain barrier. Dexamethasone is usually administered simultaneously with antibiotics for meningitis. In vasogenic edema, mannitol, on the contrary, increases the flow of fluid into the tissue. To protect the brain parenchyma, antioxidants and agents to improve metabolism (Actovegin, Cortexin) are used.
How to recover?
Brain edema, which has developed in a climber due to the desire to quickly gain height, or the accumulation of fluid in a separate area of the brain (local edema), which has arisen for another reason, may not require treatment in a hospital and will go away in 2-3 days. True, a person will be prevented from being particularly active by the symptoms of AMS, which will still be present (headache, dizziness, nausea). In such a situation, you will have to lie down for several days and take pills (diuretics, analgesics, antiemetics). But in severe cases, treatment may not even be limited to conservative methods - sometimes surgical intervention is required.
To treat cerebral edema, conservative methods are used:
- Osmotic diuretics (mannitol) and loop diuretics (Lasix, furosemide);
- Hormone therapy, where corticosteroids (for example, dexamethasone) prevent the expansion of the area of edema. Meanwhile, it should be borne in mind that hormones are effective only in the case of local damage, but do not help with the generalized form;
- Anticonvulsants (barbiturates);
- Medicines that suppress agitation, have muscle relaxant, sedative and other effects (diazepam, relanium);
- Vascular agents that improve blood supply and nutrition to the brain (trental, chimes);
- Inhibitors of proteolytic enzymes that reduce the permeability of vascular walls (contrical, aminocaproic acid);
- Medicines that normalize metabolic processes in the brain (nootropics - piracetam, nootropil, cerebrolysin);
- Oxygen therapy (oxygen treatment).
surgery, depending on the form of edema
- Ventriculostomy, which is a minor operation that involves draining cerebrospinal fluid from the ventricles of the brain using a hollow needle and catheter;
- Cranial trephination, which is performed for tumors and hematomas (eliminates the cause of OGM).
It is clear that for such treatment, where surgery is not excluded, the patient is required to undergo mandatory hospitalization. In severe cases, the patient should generally be treated in an intensive care unit, since it may be necessary to maintain basic body functions with the help of special equipment, for example, if a person cannot breathe on his own, he will be connected to a ventilator.
Forecast
Cerebral edema after a stroke in adults develops under the influence of a number of factors. Epidemiological includes a history of hypertension or coronary heart disease. An important clinical criterion is a score on the neurological scale NIHSS for stroke above 20 in the dominant hemisphere or more than 15 in the non-dominant hemisphere. Development of nausea and vomiting the first day after a stroke. Systolic blood pressure is above 180 mm Hg. the first 12 hours after the attack. Decreased reactions to stimuli.
You can determine the risk of cerebral edema using MRI:
- occlusion of large arteries;
- damage to a large number of vessels;
- anomalies of the circle of Willis.
- infarction greater than 82 ml 6 hours after the onset of symptoms;
- outbreak of more than 145 or 14 hours after the first signs.
In case of traumatic brain injuries, even before hospitalization, it is important to begin neuroprotective therapy, the administration of corticosteroids and diuretics, which improves the prognosis in young patients.
What development options are possible?
Depending on the spread of edema, three syndromes of its development are distinguished:
- General cerebral – associated with an increase in intracranial hypertension. Headache, vomiting, visual disturbances, decreased pulse due to increased SBP and impaired thinking.
- Rostrocaudal growth syndrome is the spread of edema to the cortex, subcortical structures and brain stem. When the cortex is damaged, convulsions appear, in the subcortical areas - hyperkinesis, pathological reflexes. Impaired consciousness means damage to the hypothalamus. Trunk damage is manifested by respiratory depression and cardiovascular activity.
- Dislocation syndrome is manifested by loss of function of the oculomotor nerves, stiffness of the neck muscles, and impaired swallowing.
When the brain stem is wedged into the foramen magnum, many changes are irreversible.
When is a visit to the doctor necessary?
Based on the above, it is necessary to pay close attention to headaches of a certain nature.
If you experience the following painful sensations, you should consult a doctor:
- if for the first time a severe and sharp pain occurs inside the head, reminiscent of an “explosion”;
- the pain is accompanied by an increase in temperature, in the complete absence of any other symptoms. When it disappears, the temperature returns to normal; - accompanied by heaviness in the cervical region;
- pain that changes over time. It became frequent, accompanied by vomiting. In this case, nausea may be absent;
- with little physical activity a sharp headache appears;
- disturbing at night and when waking up. Continues throughout the day and subsides towards evening;
- accompanied by impaired motor function, vision, thinking, and convulsions.