Pleurisy is an inflammation of the pleura, a thin membrane that covers the lungs and lines the inside of the chest. This pathological condition is not an independent disease, but rather a symptom that occurs for various reasons.
Pleurisy is accompanied by the appearance of pronounced symptoms that worsen the patient’s condition. Treatment of the pathology can be carried out using both conservative therapy and surgical intervention. Only a specialist can determine how to treat pleurisy after a thorough examination of the patient.
General characteristics of the disease
Pleurisy means inflammation of the pleura, the smooth serous lining of the lungs and the inner surface of the chest. It is represented by two layers - visceral (pulmonary pleura) and parietal (parietal pleura). The first one fits tightly to the lung tissues and is fused with them, the second one is connected to the surface of the chest. The parietal pleura covers different parts of the chest, therefore it is distinguished into costal, mediastinal and diaphragmatic.
Between the layers of the pleura is the pleural cavity. Normally, it should contain serous fluid, which allows the pleural layers to slide easily. With dry pleurisy, there is no effusion in the pleural cavity, that is, it remains dry.
Dry pleurisy, like other types of this pathology, can be infectious or non-infectious (aseptic). Depending on the course of the disease, acute, subacute and chronic forms are distinguished. An acute disease is accompanied by severe symptoms; in the subacute course of the disease, its symptoms appear moderately, while chronic pathology is characterized by a sluggish course.
In contrast to dry, exudative pleurisy is distinguished, that is, implying the formation of fluid in the pleural cavity. It is possible to transform one form into another. More often, dry pleurisy transforms into an exudative disease. This is usually due to obstruction of lymph drainage.
With dry pleurisy, exudate is formed, but in such a small quantity that the pleura absorbs it back, and fibrin threads settle on its surface. Such deposits prevent the sliding of the pleural layers, and the mobility of the lung is limited.
Stages of pathology
Fibrinous pleurisy is the body’s response to foreign bodies (microbes), developing in three stages:
- In the first stage, the infected person's blood vessels dilate. They are easily permeable and susceptible to various damages. As a result, the amount of accumulated fluid increases sharply.
- The second stage is characterized by the formation of a purulent mass, and pathology gradually develops. Certain deposits, known as fibrin deposits, create friction on the pleura as the patient breathes. The pleural cavity is filled with pockets and adhesions. All this disrupts the decrease in exudate. In general, the outcome of all of the above is a purulent formation.
- The third stage includes the patient’s recovery process; all disturbances that have occurred in the body gradually return to normal thanks to medications and various procedures. However, the disease does not leave the patient’s body - it enters a chronic stage and lurks in the body, but often does not manifest itself in the future. The person becomes much better, although the infection cannot be called completely defeated.
Causes
Dry pleurisy is a secondary pathology. This means that it does not develop independently, but against the background of any diseases.
One of the common causes of fibrinous pleurisy is tuberculosis. This may be damage to the lungs or intrathoracic lymph nodes. Pathology can also occur with nonspecific lung damage - pneumonia, bronchiectasis, abscess, heart attack, oncology.
The cause of dry pleurisy may lie in diseases that occur outside the lungs. These include damage to the digestive organs (pancreatitis, cholecystitis), systemic vasculitis, rheumatism, various infections (influenza, measles, whooping cough, typhoid).
Dry pleurisy of a traumatic nature is also distinguished. The inflammatory process can occur against the background of injury, including during surgery, if blood discharge enters the pleural cavity.
It is not always possible to determine the causes of dry pleurisy. In this case, the disease is called idiopathic. If there is also a version that the disease is primary, that is, it arises independently (if its cause is unknown, this is exactly what it seems).
If dry pleurisy was initially aseptic, then infection may occur during the course of the disease. This is due to the fact that the act of breathing is disrupted against the background of the disease. This leads to a lack of oxygen in the tissues and weakening of the body, which makes it more susceptible to various pathogens - staphylococci, pneumococci, gram-negative bacilli and other pathogens.
With the development of infectious dry pleurisy or the addition of a secondary infection, there are several possible ways for the pathogen to enter the pleural cavity:
- hematogenous (bloodstream);
- lymphogenous (lymph flow);
- contact (other organs affected by infection);
- direct (operation, puncture);
- traumatic injury.
Serous
Serous-fibrinous pleurisy is detected in the course of damage to the mediastinal nodes and lymph nodes. Tuberculosis is the main cause, the source for the manifestation of this disease. The allergic process, perifocal inflammation and tuberculous damage to the pleura are the three most important factors for the development of pathology. Its symptoms resemble ordinary pleurisy. This is a consequence of the fact that the initial stage of this type of disease is dry fibrinous pleurisy. Two types of pleurisy, serous and serous-fibrinous, have their own similarities and differences. The causative agents of such ailments include a number of viral diseases, as well as the notorious typhoid fever, syphilis, diphtheria and periarteritis nodosa.
Based on the location of the tumor itself, diaphragmatic, mediastinal (posterior, anterior, left lateral, right, etc.), parietal (mantle-shaped, interlobar) types are distinguished.
Symptoms of dry pleurisy
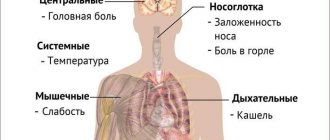
The clinical picture of the disease may vary depending on its cause and the location of the pathological process. There are several common symptoms:
- pain when breathing, bending in the direction opposite to the affected area;
- prolonged persistence of low-grade fever;
- fever is accompanied by chills and tachycardia;
- sweating (mainly at night);
- reflex cough (response to irritation of the pleural layers);
- breathing quickens and becomes shallow;
- general malaise.
To reduce pain, patients are forced to lie on their side (on the affected side). Auscultation reveals friction of the pleura - the noise can be localized or widespread.
If the costal pleura is involved in the pathological process, then the onset of the disease is accompanied by severe pain in the corresponding part of the chest. Painful sensations become stronger at the peak of inspiration, during coughing, and straining. When the activity of the inflammatory process decreases, the pain syndrome decreases. This is due to a decrease in the sensitivity of the nerve endings of the pleura.
If the diaphragmatic pleura is affected, the pain is localized in the abdominal cavity. The clinical picture in this case resembles damage to the digestive organs - acute cholecystitis, pancreatitis, appendicitis.
Painful sensations are caused by friction of the pleural layers, so the intensity of the pain syndrome depends on the amount of fibrinous deposits on the pleura.
With dry pleurisy, the patient tries to restrain the cough, which intensifies the pain. At the same time, ventilation of the lungs deteriorates, which is fraught with the development of hypoxia with corresponding signs - cyanosis of the skin and visible mucous membranes, deterioration in general well-being.
Any of the listed symptoms cannot be ignored. Any deviation from the norm is an alarming sign and a reason to consult a doctor.
Diagnostics
Several specialists are often involved in the diagnosis of pleurisy: a pulmonologist, a phthisiatrician, a rheumatologist, a gastroenterologist, and an infectious disease specialist. This is due not only to the variety of manifestations of the disease, but also to its various causes.
One of the first stages of diagnosis is auscultation. It reveals weakening of breathing, noise against the background of friction of the pleural layers.
In order to diagnose dry pleurisy, a number of laboratory and instrumental studies are carried out:
- Blood tests. With dry pleurisy, the number of leukocytes and the erythrocyte sedimentation rate slightly increase.
- X-ray and fluoroscopy of the lungs.
- Ultrasound scanning. This study allows us to exclude the presence of exudate.
- Pleural puncture.
- Thoracoscopy is an endoscopic examination of the pleural cavity.
With dry pleurisy, differential diagnosis is necessary. It is carried out to exclude the following pathologies:
- intercostal neuralgia;
- myositis;
- rib fracture;
- angina attack;
- myocardial infarction;
- pathology of the abdominal organs.
Pleurisy can acquire an exudative character, but the increased absorption surface of the pleura sometimes leads to the persistence of the dry form of the disease. In this case, diuresis may increase, which raises suspicion of kidney damage. Against this background, additional tests are prescribed: urine tests, ultrasound of the kidneys.
For diagnostic purposes, lavage of the pleural cavity can be performed. The liquid remaining after the procedure is used for bacteriological culture - this makes it possible to determine the nature of the disease (infectious, aseptic).
Symptomatic manifestations
A reliable auscultatory sign of fibrinous pleurisy is the friction in the pleura characteristic of this disease. Sometimes this sound resembles the crunch of dry snow. In addition, its most striking signs are: a painful, dry, severe cough, pain in the chest area, or even hiccups. Moreover, patients suffer from high fever or chills, shallow breathing, weakness and sweating. On an x-ray with fibrinous pleurisy, a clear lag in breathing is observed on the affected side. In medical practice, the most difficult and main task is to timely distinguish pleurisy from a rib fracture or intercostal neuralgia.
Treatment of dry pleurisy
Pathology occurs against the background of various diseases, so the main goal of treatment is to eliminate its root cause. The measures taken mainly depend on this.
General recommendations
One of the main manifestations of dry pleurisy is pain, therefore, in the acute course of the disease, the patient is prescribed bed rest and a tight pressure bandage on the chest. In agreement with the doctor, cups and mustard plasters are applied, and warm compresses are made.
With dry pleurisy, a massive adhesive process may occur in the pleural cavity. To prevent it, it is effective to perform breathing exercises.
With dry pleurisy, you need to eat a balanced diet. Carbohydrates and salt are limited, and the amount of protein is increased.
Drug therapy
If fibrinous pleurisy has a tuberculous etiology, then specific anti-tuberculosis drugs are prescribed: Rifampicin, Tubazid, Isoniazid, Streptomycin.
In case of nonspecific damage to the lungs and other organs, they resort to antibacterial therapy and anti-inflammatory drugs. An antibiotic is prescribed after identifying the pathogen or broad-spectrum drugs are used.
To combat the inflammatory process, non-steroidal anti-inflammatory drugs are usually prescribed. Steroid hormones are used for the same purpose - they are more effective, but are used for a short course due to the high risk of side effects. Among the glucocorticosteroids, hydrocortisone, Prednisolone, Methylprednisolone can be prescribed.
With dry pleurisy, a cough often develops, so the use of antitussive drugs such as Codeine, Ethylmorphine, Butamirate is appropriate.
Physiotherapy
Various physiotherapeutic methods can be used in the treatment of dry pleurisy. They are often prescribed after the main therapeutic course in order to speed up recovery and rehabilitation.
Treatment may include the following procedures:
- phonophoresis with medications;
- warming up with a Minin reflector (blue lamp);
- paraffin applications;
- inductothermy;
- diathermy;
- electrophoresis (with calcium for tuberculosis, with iodine for adhesions).
Surgical intervention
Surgical treatment may be required for advanced pleurisy, its recurrent nature and the development of serious complications. Surgery is also necessary if the conservative approach is ineffective.
If dry pleurisy recurs, then resort to pleurectomy with decortication of the lung. This operation involves the removal of pleural layers that have formed an encysted purulent cavity. The pleural sac is removed from the chest cavity, and fibrous layers are removed (decortication) to allow the lung to expand.
Prognosis, complications
The prognosis of dry pleurisy depends on the cause that caused it. In many cases, with timely identification of the disease and its root cause, as well as proper treatment, the outcome is favorable.
If dry pleurisy acquires an exudative form or recurs, the patient’s ability to work may be limited for a long time. There is a risk of developing chronic pneumonia.
Other organs may also be involved in the inflammatory process. These include the pericardium, inflammation of which is called pericarditis.
Diagnostic measures
One of the most important and difficult tasks on the path to recovery is the correct diagnosis of the disease. The most common way to detect pleurisy is considered to be an x-ray.
A complete blood count reveals leukocytosis, increased ESR or anemia. In addition, a urine test shows the presence of epithelium or red blood cells. The content of total protein, as well as foreign bodies (fibrinogen or sialic acids), is determined by a biochemical blood test.
Fibrinous-purulent pleurisy can be detected using a microscopic specimen. A microslide is a glass slide on which the unit being studied is placed. Using a microscope, objects in contaminated areas are examined. Fibrinous-purulent pleurisy is shown below on a demonstration microslide.
Prevention
Fibrinous pleurisy is characterized by severe and extremely unpleasant symptoms and can lead to serious complications. Prevention of pathology consists of the following measures:
- timely treatment and prevention of diseases that can cause dry pleurisy;
- regular medical examinations;
- avoiding hypothermia;
- strengthening the immune system;
- hardening;
- balanced diet;
- sufficient intake of vitamins from food, if necessary, additional intake of vitamin complexes (take after consultation with a doctor);
- sufficient physical activity;
- absence of bad habits.
Pleurisy is an inflammatory process. It is characterized by vivid clinical manifestations and the risk of complications. It is important to promptly identify the pathology and its cause and begin proper treatment. You can reduce the risk of such a disease by following certain preventive measures.
Rehabilitation
Even after complete relief from this disease, you should visit sanatoriums for the first 2-3 years. If the treatment was carried out correctly and all necessary procedures were performed, then complications should not arise. In case of untimely initiation of therapy or weak immunity, valvular pneumothorax may occur. However, its treatment is not difficult, and it appears extremely rarely.
In conclusion, we cannot help but recall that fibrinous pleurisy is a serious disease. It cannot resolve on its own, so attempts to treat it on your own, without experienced specialists, only worsen the patient’s well-being. As a result, sooner or later he ends up in the hospital, but by this time the disease is already too advanced. Unfortunately, there are known cases of death in medical practice, but they occurred decades earlier, and even then very rarely. You should pay more attention to your health and contact a specialist at the slightest change in your well-being.