Fluorography is a method of x-ray examination that allows X-rays to penetrate the human body, recording the resulting image on the image screen. The quality and uniformity of a fluorography image is determined by the ability of different body tissues to absorb these rays. In the picture, the heart, bronchioles, ribs and the bronchi themselves appear as light spots. Unevenness of lung tissue and white spots in the wrong place may indicate the presence of various pathologies: fluorography shows pneumonia, emphysema, tuberculosis, obstructive pulmonary disease and other diseases of the pulmonary system.
Doctors at the Yusupov Hospital carefully approach each case, prescribing proven medications and procedures that speed up the treatment process and minimize the risk of complications.
What is fluorography method
The X-ray diagnostic method has been known for a long time. It is based on the properties of X-rays, which pass through the tissues of the human body unevenly, due to which shadows are visualized in the image.
When examining pulmonary shadows, it is possible to diagnose inflammatory, oncological and infectious pathologies.
X-ray of the lungs is the norm.
Fluorography began to be used in the nineteenth century as an alternative to standard chest radiography, at that time it made it possible to significantly reduce research resources. The X-ray film that was required to visualize the OGK was large; a direct and lateral shot was required to complete the picture.
Fluorographic research made it possible, thanks to a high dose of radiation, to project an image on a film measuring 3.5x2.5 cm. The films in the device were one after another, each patient corresponded to a serial number, the images were developed at the end of the frame series.
This approach made it possible to reduce the time required for diagnosis and conduct research on 100 people in an hour. Thanks to these properties, chest fluorography began to be used as a preventive screening examination.
Modern devices use digital data processing, their radiation exposure is much lower and the images are broadcast on the device’s monitor screen and stored in the computer’s memory. The purpose of the method has remained the same: the study is carried out twice a year in people over 15-16 years of age and once a year in some categories (at-risk groups and for professional reasons).
Digital scanning fluorograph (the safest and most modern diagnostic method)
FAQ
Fluorography can perhaps be called the most famous and popular form of diagnosis. However, there is still some misunderstanding. Let us reveal the answers to the most common questions about the well-known “stick”.
Who makes FLG
A referral for the procedure is usually issued by a physician. If desired, the examination can be done without a doctor's prescription.
An x-ray technician works with a patient in a fluorography room. But fluorography is interpreted by a specialized specialist - a radiologist, pulmonologist, or phthisiatrician.
How long is fluorography valid?
The results of fluorography of the chest area are considered valid for 12 months. In the absence of indications, it is not recommended to undergo this radiological examination more often.
There are categories of citizens who need to undergo a preventive FLG examination once every six months. This includes people who are at risk due to an increased risk of infection or the development of occupational respiratory diseases. These are medical staff of maternity hospitals and tuberculosis dispensaries, workers whose activities are associated with hazardous production (steel industry, rubber, asbestos production, mining).
How often can fluorography be done?
Fluorographic examination is a mandatory preventive screening aimed at early detection of tuberculosis and lung cancer. The frequency of its passage for an adult is once a calendar year, but not less than once every two years. According to the law, a citizen has the right to refuse FLG, but before making such a decision, one should be aware of all the risks and possible consequences of such actions. Some citizens need to take a photo more often due to special professional conditions or health conditions.
If the fluorogram turns out to be defective, if there is a suspicion of diseases of the respiratory system, accompanied by concomitant symptoms, the doctor will refer the patient for the procedure again. There are no clear restrictions on the number of sessions allowed. It is only important not to exceed the permissible annual total radiation dose.
At what age can you pass
Fluorography is allowed for children only after they turn 16 years old, in some states - from 14 years old. If the danger to the life and health of the child in the absence of timely diagnosis exceeds the probable risks of the consequences of radiation, targeted radiography of the affected area is performed, and less often - FLG.
Who needs to undergo fluorographic examination more often?
Fluorography of the lungs should be performed every six months:
- employees of maternity hospitals;
- medical personnel whose activities are related to the treatment of tuberculosis patients;
- workers employed in the mining industry;
- citizens employed in hazardous industries - production of rubber, asbestos, steel casting and the like.
Are X-rays wrong?
The likelihood of obtaining unreliable results during any x-ray examination is negligible. This fact is usually associated with errors made during the scanning process, if the patient did not remain still, or foreign objects, such as hair or jewelry, got into the image. The human factor cannot be ruled out, when the radiologist interpreting the image incorrectly interpreted the resulting picture.
Fluorography and X-ray of the lungs - what is the difference
Both fluorography and radiography are methods based on the properties of ionizing rays. The principle and algorithm for both procedures are the same. In both cases, the image is obtained on film or a digital matrix after passing a beam of radiation through the tissues of the human body. The difference is that an X-ray image is a picture of the organ under study in real size, while a fluorographic image is a reduced one. This explains the differences in the radiation dose (with FLG it is lower) and the cost of the procedure (X-ray is a little more expensive because it requires more consumables).
Types of fluorography
To this day, there are two types of FLG left:
- Film. The study is carried out using outdated equipment, the radiation dose is higher than with conventional radiography, and the information content is low due to the small size of the film.
- Digital. A modern minimally invasive method in which the radiation dose is significantly reduced thanks to computer data processing.
Modern equipment takes pictures not only in a direct classical projection, but also in a lateral one. The angle allows us to examine the lesions that are covered by the bony framework of the chest (sternum, ribs), as well as the shadow of the heart.
What can you see in the photographs?
After the procedure, the doctor determines various pulmonary anomalies from the images.
Here are the main ones:
- adhesions;
- fibrosis;
- layers;
- sclerosis;
- heaviness;
- radiance;
- scarring.
If the patient is asthmatic, then the image will convey disturbances in the form of swollen bronchial walls that appear due to excessive tension.
Also in the pictures you can find:
- cyst;
- abscesses;
- calcifications;
- emphysema;
- cancerous formations.
When to do research
Indications for the study, in addition to the annual screening examination, are:
- prolonged unmotivated fever (temperature stays up to 37.5˚C);
- persistent cough;
- chest pain;
- hemoptysis;
- shortness of breath attacks;
- rapid loss of body weight for no apparent reason.
For the listed symptoms, the doctor prescribes an x-ray of the lungs .
Compaction syndrome.
Low to medium density lesion. Tuberculosis. Sometimes the study is required for a preventive examination twice a year. The following categories of people need in-depth diagnostics:
- workers of tuberculosis dispensaries, infectious diseases departments, sanatoriums, maternity hospitals;
- HIV patients;
- people with diabetes;
- presence of tuberculosis in the family;
- radiation, hormonal and/or cytostatic therapy;
- cancer patients.
The study is necessary, since in this category of people the risk of infection with the tuberculosis bacillus or the spread of metastatic lesions to the lungs increases. This approach will allow us to identify foci of pathology in the early stages, prevent the spread of infection and begin therapy in a timely manner.
Fluorography for pneumonia
Pneumonia (pneumonia) is an acute lesion of the pulmonary lobes that is infectious and inflammatory in nature. This inflammatory process involves the alveoli, lung tissue, and in case of improper treatment or severe form, other structural elements of the respiratory system. Diagnosis of pneumonia is carried out by auscultation, blood tests, and also using such common methods as x-rays or fluorography. With pneumonia, the clinical picture is characterized by the following symptoms:
- fever;
- cough (dry, wet, with mucus, paroxysmal or continuous);
- shortness of breath or shortness of breath;
- pain in the chest (most often in the right side);
- dizziness and headaches;
- general weakness and weakness;
- increased sweating;
- drowsiness and decreased appetite.
There are a number of factors that predispose to the development of pneumonia:
- old age or under 5 years of age;
- smoking and alcoholism;
- hypothermia;
- insufficient physical activity;
- unbalanced diet;
- diabetes;
- poor immune system function (including HIV);
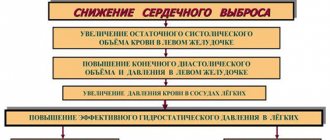
- chronic heart failure;
- atherosclerosis;
- oncological diseases.
Today, pneumonia is one of the leading causes of death among adults and children. Most deaths occur precisely as a result of untimely treatment. It is very important to start treating pneumonia at the first stages of its development, as this reduces the risk of developing side pathologies several times.
Contraindications for diagnosis
Since fluorography uses ionizing x-ray radiation, there are some contraindications to the study. Pregnancy is prohibited, since first of all, the X-ray method can cause gene mutations and congenital deformities of the fetus.
A relative contraindication is the lactation period. If necessary, diagnostics are carried out, but the child is weaned from the breast after 3-4 feedings and transferred to artificial feeding.
The study is not carried out on children under 15 years of age. Since the diagnosis is used to screen for tuberculosis and cancer, there is no need to expose the child’s body to unnecessary radiation.
Until the age of 15, children undergo a Mantoux test every year to determine infection with the tuberculosis bacillus. Cancer in childhood is a variant of a casuistic rare case and an X-ray image according to indications will be more informative.
What other additional examination may be required and why?
If the results of fluorography clearly indicate the presence of pathologies, the patient is sent for further examination. In this case, the fluorography transcript contains the code “R+” and the number 1 in the last (fourth) column. The main reasons for further examination are the need to establish a more accurate clinical and pathological picture, obtaining comprehensive information about the causes of anomalies and selecting adequate therapeutic measures.
The list of additional procedures that include additional examination after fluorography depends on the detected deviations:
- in case of deviations in the mediastinum, indicating heart pathologies, hypertension, a complex of cardiological studies is prescribed - blood biochemistry, blood for hormones, cardiogram, echocardiogram, consultation with a cardiologist;
- in case of deformation of bone structures, radiography of the spine and chest is required; if necessary, an MRI or CT scan of these parts of the musculoskeletal system is performed;
- if the diaphragm is deformed, the patient is sent for consultation to a gastroenterologist and surgeon, who will recommend undergoing an abdominal ultrasound, gastroscopy or colonoscopy, if radiologists have not directed these studies immediately after receiving the results.
If the patient was not sent for further examination when calcifications or signs of adhesions or localized fibrosis appeared on the fluorography image, there is no cause for concern. These conditions are not considered dangerous to health and require only systematic monitoring. If progress appears (increase in size, spread to neighboring tissues), the doctor will definitely write out a referral for further examination. He will not do this without visible reasons.
What does the study show and what diseases does the study reveal?
What diseases does fluorography reveal?
Depending on the radiological signs, the doctor assumes that the patient has the following pathologies:
| Symptoms that can be seen on fluorography | Main pathologies |
| Strengthening the pulmonary pattern | Inflammatory lung diseases. Obstruction of the bronchopulmonary system. Hypertension of the pulmonary circulation in congenital and acquired diseases of the cardiovascular system. Enlarged heart. Compaction of the aorta. |
| Ring shadows | Open forms of tuberculosis are cavities. Lung abscesses or cysts with fluid contents. |
| Darkening in the lungs | Inflammation (focal pneumonia). Oncological focus. Metastases of cancer of other organs to the lungs. Tuberculoma. |
| Violation of the structure of the pulmonary roots | Infectious process of lung tissue (both nonspecific with pneumonia, bronchitis, and with specific damage to tuberculosis, Pneumocystis pneumonia). Chronic obstructive disease of the lung tissue. Lymphogranulomatosis and other lesions of lymphoid tissue. |
| Calcifications (focal shadows, bone density) | Long-term infection with tuberculosis. |
| Diffuse small shadows in the form of a “snow storm” | Diffuse form of tuberculosis or Pneumocystis pneumonia in association with HIV infection. |
| Changes in the sinuses (disappearance of the angle, presence of fluid level in it) | The presence of pathological pleural effusion or adhesive pleurisy. |
| Fibrosis | The result of chronic pulmonary pathology. |
| Adhesions (seals in the area of contact of the parenchyma and pleura) | Indicate previous pleurisy, pleuropneumonia. |
| Pleuroapical layers (thickening of areas of the pleural layer) | Chronic long-term pulmonary tuberculosis, relapse of the disease. |
| Emphysema | COPD Bronchial asthma. |
Compaction syndrome. Infiltrate. Cancer.
X-ray of the lungs for pneumonia
An X-ray for pneumonia is performed if the doctor has recorded all visible signs of the disease and if laboratory tests (blood and urine tests) have confirmed this. There are no contraindications to x-rays, but it is recommended that women avoid this test during pregnancy. But in cases where the expected benefit to the mother’s health outweighs the harm to the child, x-rays are still used during pregnancy, while doing everything possible to minimize exposure to radioactive rays. There are two classifications of pneumonia, the differences of which are clearly visible on an x-ray: focal pneumonia (clinical manifestations include fever, wheezing during breathing, a slight increase in leukocytes in the blood. In the image, the initial stage of focal pneumonia may not be revealed, since of the obvious signs only the presence of a small infiltrate in the pleural cavity. However, a competent Yusupov hospital is able to determine the inflammatory process in the respiratory system by the following signs: by an increase in the size of the root of the lung due to effusions in the pleural cavity, by the presence of an uneven structure of the lungs, the level of the pleural cavity (pleurisy), dark spots in the lung area , which indicate a decrease in the airiness of the lung tissue) and lobar pneumonia (usually seen in the picture as a large, medium-intensive darkening. Can be localized in one or two pulmonary lobes. The causative agent of lobar pneumonia is most often Friendler's bacillus, which is dangerous to human life and can cause more severe consequences. Signs of lobar pneumonia on fluorography or x-ray include: total or subtotal darkening in the lung area, deformation of the domes of the diaphragm, total or subtotal deformation of the lung structure, pleural effusions, changes in the shape of the roots of the lungs).
Fluorography results
After the diagnosis, the radiologist interprets the study. It identifies pathological changes, a description of the results is transmitted to the local doctor during preventive examinations or to the referring specialist (pulmonologist, therapist, pediatrician, etc.).
If the lung tissue is normal, the results are stored in the clinic where the study was performed. If necessary, archives are retrieved and provided to the patient.
Regular fluorographic examinations help to predict the time of onset of pathology and identify the disease at an early stage. Based on the data obtained, the attending physician makes recommendations: continues the diagnostic search or prescribes therapy.
Main indications
The main task pursued by the method is to search for ailments related to deviations in the functioning of the lungs or bronchi. It is not for nothing that the technique is considered a preventive approach that prevents serious complications for diseases of the respiratory system.
Typically, a local physician or pulmonologist sends you to take the test at a clinic. The victim comes to them with three characteristic symptoms of possible pathologies in this part:
- prolonged persistent cough;
- dyspnea;
- pain syndrome in the chest area.
When the above signs are detected, the chance of detecting a pulmonary or bronchial deviation increases significantly. Often, a control cut allows you to establish:
- inflammatory process even at the initial stage of development;
- pneumothorax;
- neoplasms of malignant and benign nature;
- pleural damage;
- emphysema.
But more often than not, even a free test, which was a simple preventive measure, reveals tuberculosis. To catch such a terrible disease, which has a high fatality rate, doctors recommend not shirking the annual mandatory examination. You can create a schedule for checks yourself by simply setting a reminder in your phone.
In addition to standard indications, there are two more categories of reasons for sending to the diagnostic office. The first concerns the need to check family members living with pregnant women or newborns. This is necessary to minimize the risk of the baby contracting a dangerous disease. For the same reason, conscripts from military registration and enlistment offices also have to go and get tested.
The second case concerns unscheduled fluorography. This means that a person could have undergone an examination just a couple of months ago, but he will be sent to do everything again if they suspect:
- foreign body in the lungs;
- inflammation;
- tuberculosis;
- tumors of the mediastinal organs;
- diseases of the heart, large vessels.
Such precautions make it possible to recognize concomitant diseases such as fibrosis or sclerosis. Also, using a small image, it is possible to establish localization:
- cysts;
- cavern;
- abscesses;
- infiltrates;
- accumulations of gases.
Despite the productivity of the technique, fluorography can hardly be called the main argument for diagnosing pulmonary pathologies. Often it is necessary to use auxiliary tests such as sputum testing and MRI with contrast.
Radiation dose during examination
Modern digital techniques have made it possible to reduce the radiation dose during fluorography of the chest organs to 0.03 mSV. The maximum annual radiation dose should not exceed 5 mSv per year; no more than 1 mSV/year is allocated for preventive photographs.
For comparison, film fluorography irradiates a person with a dose of 0.1-0.3 mSV, and digital fluorography - 0.02-0.05 mSV. X-ray of the lungs is performed in 2 projections, so the total dose is 0.1 mSV. Fluorography is a safe method that is often used to monitor changes in lung tissue during therapy.
How harmful is the procedure?
Rumors about the dangers of fluorography are greatly exaggerated. Indeed, during the session the patient is exposed to radioactive radiation, but its dose is so small that it is not capable of causing damage to his health. Much more dangerous may be the consequences of refusing to do such a procedure every year.
After fluorography, the patient does not experience any discomfort, nothing hurts.
Radiation dose
In accordance with the requirements set out in the Resolution of the Chief State Physician of Russia, the annual permissible dose of radiation exposure to the body during medical procedures should not exceed 1 mSv. During fluorography, the patient is exposed to radiation in the following doses (depending on the type of equipment used):
- film FLG on old-style devices – 0.6-0.8 mSv;
- film FLG using modern technology – 0.15-0.25 mSv;
- digital FLG - 0.03-0.06 mSv, with the latest equipment - approximately 0.002 mSv.
For reference, the critical dose of radiation received is 700 mSv.
FLH during pregnancy and breastfeeding
Pregnancy is a period when X-ray examinations can really cause harm. Its passage is especially dangerous in the first trimester, which is characterized by processes of active growth and the formation of the main organs and systems. At this time, intensive cell division of the embryo occurs, and ionizing radiation is a factor that provokes the occurrence of mutations.
For women carrying a child, fluorography is prescribed in extreme cases, when there are no alternative, safer diagnostic methods, and the threat to the health and life of the mother if it is not performed exceeds the risks to the baby. In this case, it is necessary to use additional protective equipment in the form of a lead apron covering the area of the patient’s reproductive organs.
Fluorography does not affect the quality of mother's milk, so lactation is not considered a contraindication.
Errors in radiographic examination
As a rule, errors in research are rare and often depend on the human factor; well-programmed equipment does not fail. The likelihood of discrepancies between reality and the result of fluorography is possible when:
- confusion of patient images;
- inexperience of the specialist deciphering the result;
- if the person did not take off his jewelry during the study (pendants, chains, piercings, etc.) or did not pick up his hair.
When a pathology is detected, the results need to be clarified, and the person is re-sent for an x-ray of the lungs in two projections.
Photo gallery
Calcifications
The roots of the lungs are compacted
Focal spots
Sinus sealed or free
Scoliosis
Fluorography image of a healthy person
Fluorography and X-ray - what's the difference?
The basis of these studies is X-ray radiation. If fluorography is used as screening, then x-ray is a more in-depth technique, which is prescribed according to indications.
If fluorography is performed exclusively in a standing position, then x-rays are performed in any position and even in severe condition of the patient, as well as at home.
When fluorography of the lungs, the images are less clear than radiographic ones, therefore the information content and dose of the second study are higher. Read more about the difference between methods in this article.
Radiography
An important aspect is also the cost of diagnostics: the price of radiography is approximately 2 times higher than FLG.
Preparation and execution
Diagnostics does not require special or complex tedious preparation. The only thing the doctor will recommend on the eve of the procedure is abstaining from smoking for several hours and a light breakfast if the examination is scheduled for the next morning. The entire procedure, including undressing and dressing, will take no more than 5 minutes.
Step by step it will look something like this:
- the patient is invited to a special room intended for taking the image;
- he undresses to the waist, approaches the apparatus, and rises to a low step;
- the chin is located in a depression approximately corresponding to the average height of a person;
- the subject is warned not to hold his breath for a minute and not move;
- the nurse turns on the device, the picture is taken, the procedure is over.
- In some situations, during fluorography, a protective apron is used, which protects the organs located in the lower part of the abdominal cavity from radiation. The results of the study are usually ready the next day.
Adverse consequences
In fact, ionizing radiation from a fluorographic apparatus, especially with digital resolution and dose reduction, does not bring any particular adverse consequences.
A person is exposed to much more radiation every day, using the benefits of civilization: telephone, wireless Internet, radio. Thus, a single study per year is harmless and necessary.
Fluorography is a good screening method that detects serious diseases at an early stage.
Thanks to the introduction of research into the list of mandatory ones, the detection of pathologies such as tuberculosis and lung cancer has increased. Early detection of pathology helps to begin the necessary treatment measures earlier and increase the survival rate and quality of life of the patient, and prevent the spread of Mycobacterium tuberculosis infection.