Any stress, immunodeficiency conditions, exacerbations of chronic diseases, intestinal and vaginal dysbiosis can trigger the appearance of primary thrush or its relapse.
What is thrush in women?
Thrush in women
- This is a disease of the vagina, scientifically called candidiasis. Associations with milk among the population arose due to the fact that women have a white discharge on their genitals, similar in consistency to cottage cheese.
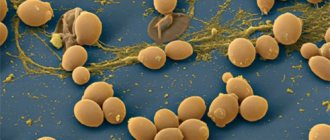
The causative agent of the disease is the fungus Candida albicans. Scientists estimate that this microorganism is present in the body of 80% of people as its own microflora, without causing any problems. A woman's vagina is not normally sterile. Its epithelium contains microorganisms, including this fungus. It is involved in maintaining normal vaginal pH levels, which is very important for the epithelium itself and the fertilization process.
The vagina's own flora, in addition, competes with other unwanted microorganisms and reduces the likelihood of developing infectious diseases. At the same time, the immune system of the female body strictly monitors the state of affairs and, if necessary, inhibits the proliferation of “its” bacteria. If for some reason this does not happen or conditions are created for their active reproduction, then the likelihood of developing thrush increases.
Candida carrier
If candidiasis is observed, this fact does not appear outwardly. A person can become a carrier of candida fungi if his immune system is functioning normally. This prevents the infection from actively developing. The first time you encounter a fungus is at birth, during passage through the mother’s birth canal. However, this flag does not mean that the infection will manifest itself in any way in the future. Typically, the first symptoms of pathology occur as a result of decreased immunity. It is for this reason that candidiasis is not classified as a sexually transmitted disease, although the risk of contracting the pathology through sexual contact is possible. However, much more often, it is not the partner who is to blame for the development of the disease, but a decrease in the body’s defenses. If a person has this type of disease, during the examination the doctor will not be able to notice any signs of pathology.
Causes of thrush in women
There are quite a few reasons that can lead to disruption of the delicate balance in a woman’s body and create conditions for the development of thrush.
- Taking antibacterial drugs
- one of the most common reasons. Many diseases currently have to be treated with antibiotics. This is an effective group of drugs that has made it possible to eliminate many deadly diseases in just a few days and prevent the development of serious complications. However, antibiotics have their side effects. They do not act selectively on one microbe and can have a bad effect on the vagina’s own microflora.
- Fungi
they have a completely different cell wall structure and antimicrobial antibiotics are not dangerous for them. The result is the following situation: fungi, the causative agents of thrush, remain safe and sound, but the bacteria suffer and partially die. Not a single niche in nature is empty, and the place of dead microbes is taken by Candida albicans, which simply has no competitors left. As a result, the woman develops candidiasis.
- Decreased immunity
, which inhibits the growth and reproduction of opportunistic flora. Candidiasis is the most common opportunistic infection in patients infected with HIV. If patients develop candidiasis in many places (oral cavity, vagina, intestines) and do not respond well to treatment, then there is a high probability that the underlying cause is HIV. Chronic inflammatory diseases and long-term bacterial infections can also negatively affect the body's immune defenses. (List of the best foods that boost immunity!)
- Impaired metabolism
- almost always this condition is caused by diabetes. Few people know that with this disease in the human body, not only does the regulation of sugar levels occur, but fat and protein metabolism also suffer. Diabetes mellitus contributes to the development of candidiasis through two mechanisms.
10 facts about the dangers of sugar, see here
- In the absence of proper control
on the human side (taking medications or insulin, monitoring glucose levels), his blood contains a lot of carbohydrates. This cannot but affect their content in the intercellular space and in the vaginal mucus. It turns out that the bacteria and fungus Candida albicans find themselves in a sweet environment, which is ideal for their nutrition and reproduction - the likelihood of developing thrush increases.
- Immunoglobulins
- these are substances due to which the immune response of the human body is implemented. The disruption of protein metabolism, which occurs in diabetes mellitus, affects their formation only in a negative way. The result is a decrease in immunity and a lack of necessary control over the condition and composition of the microflora. Fungi readily take advantage of this, given the good nutritional environment, and multiply uncontrollably, causing candidiasis.
- Unbalanced and irrational nutrition
- Normally, a person should take proteins, fats and carbohydrates daily in a certain ratio by weight. Many girls and women call themselves sweet tooths and eat unaffordably large amounts of sweets, flour products, and sweet carbonated drinks. Their pancreas tries, but cannot produce enough hormone to lower their blood glucose levels to even the upper limit of normal. Then everything happens approximately as described in the case of diabetes: a lot of sugar in the blood - a lot of sugar in the vaginal epithelium - good conditions for the proliferation of Candida albicans. In addition, people who abuse sweets increase the risk of developing type 2 diabetes, which is much more serious and dangerous than thrush.
- Hormonal background.
The condition of a woman’s genital organs, including the vagina, greatly depends on the hormonal levels in her body.
- Pregnancy
can lead to a significant change in it, which increases the likelihood of developing thrush.
- Incorrectly selected hormonal contraceptives
can change the level of hormones in the blood so much that the likelihood of developing candidiasis increases.
- Many diseases of the endocrine system
can lead to the development of thrush. Experienced doctors always remember this and try to find that original factor. This allows not only to prevent the development of candidiasis in the future, but also to eliminate hormonal pathology, which is important.
- Wearing tight synthetic underwear or improper use of sanitary pads
(they need to be changed quite often) creates conditions under which heat and moisture do not escape, and these are ideal conditions for the growth of fungi.
Symptoms of thrush in a woman
The disease has quite specific manifestations, which allows doctors to quickly make the correct diagnosis. Often, women themselves, even before visiting a doctor, understand what kind of illness they have and begin to make their own attempts at treatment, which is unacceptable.
So, thrush is characterized by:
- Curd-like discharge from the external genitalia.
They are especially noticeable on dark underwear. They are mucus with a large number of white lumps.
- Feeling of itching and burning in the vaginal area.
In no case should you try to scratch the affected area too much, as this can damage the delicate inflamed epithelium and create conditions for pathogens to penetrate deep into the tissue. Also, when scratching, the discharge spreads over a large surface and causes additional inflammation.
- Pain and discomfort when urinating
- caused by a decrease in the protective properties of vaginal and urethral mucus. The epithelium becomes defenseless against such an aggressive liquid as urine, and inflammation increases the sensitivity of the receptors.
- Pain and burning during sexual intercourse
- this is just one of the reasons why you should abstain from sexual activity until the disease recedes.
- Smell – this should be discussed separately.
It is not very pronounced and has a sourish tint (“kefir”). In most cases, only the woman feels it, but for her it is a very big problem. Patients believe that all her interlocutors will certainly be able to catch it. Many sexually transmitted diseases and bacterial vaginosis are accompanied by a really unpleasant odor, but it has almost nothing to do with thrush.
With an erased (atypical) course of thrush and mild symptoms, women may be bothered by only one of the indicated signs. It is impossible to find out about the disease in such cases without professional help. Candidiasis often accompanies many gynecological diseases, including hidden and dangerous sexually transmitted infections. Only a qualified doctor can analyze the symptoms and prescribe the correct treatment. Self-diagnosis in severe cases of the disease is useless, and self-medication is dangerous.
A comparative table of characteristic symptoms for thrush, bacterial vaginitis and trichomoniasis can be seen in the table. It should not be considered as a diagnostic aid. Diagnoses are made by a doctor based on tests, examination and complaints of the patient. Even in such cases, the presence of other sexually transmitted infections accompanying thrush cannot be ruled out. Self-medication is unacceptable. All prescriptions must be made by the attending physician.
| Thrush | Smell: Sourish Allocations: Homogeneous, thick, milky in color, reminiscent of cottage cheese Discomfort: Burning, itching, pain during intercourse and urination |
| Trichomoniasis | Smell: Unpleasant fishy smell Allocations: Abundant, purulent, foamy yellowish-green hue Discomfort: Intense increasing itching (external and internal), difficulty urinating, redness (irritation) of the vaginal mucosa. |
| Bacterial vaginitis | Smell: Fishy smell (typical of discharge) Allocations: Abundant and liquid gray-white, sometimes foamy Discomfort: Vaginal itching, burning, irritation of the mucous membrane. |
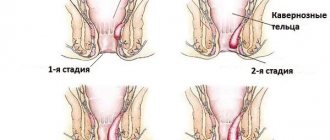
How to identify a fungus using a photo of candidiasis as an example?
In this article you can see a photo of what thrush looks like. For example, the following photograph shows the following: the skin of the vulva, clitoris, labia minora and majora, and the area surrounding the external opening of the urethra is intensely red and swollen. There are a large number of thick white pinpoint areas with round and oval plaques.
Small and shallow erosions (bright red defects with a shiny surface) are also visible. At the entrance to the vagina, you can find a slight residue from typical discharge and traces in the form of excoriations (formed due to scratching).
Thus, we can conclude that classic discharge from candidiasis is thick and abundant, has a dense consistency and a white, mushy appearance. As a rule, they are accompanied by a sour odor and severe itching. The reasons for the appearance of mixed discharge vary from the banal onset of the menstrual cycle to severe trichomoniasis or bacterial vaginosis. In any case, treatment should be selected by a doctor. Additionally, herbal remedies can be used to relieve symptoms; a striking example here is Candiston spray for thrush.
The first signs of thrush in a woman
The first signs of the development of thrush, which make a woman wary, are:
- Acute burning and itching in the external genital area;
- Hyperemia (redness) of the external genitalia and vagina;
- The appearance of copious white vaginal discharge;
- Painful urination;
- Painful sensations during sexual intercourse.
As a rule, the first symptoms appear a week before the start of menstruation. Burning and itching intensify significantly in a warm environment, especially after taking a bath, and often interfere with sleep. And the appearance of white discharge removes all suspicions a woman has about the disease and forces her to see a doctor.
Prevention
To exclude fungal infection, preventive measures are necessary. This will help avoid relapse after successful healing. Rules to be followed:
- avoid sexual intercourse during treatment;
- follow hygiene rules;
- support immunity;
- treat chronic diseases in a timely manner;
- have sex with a regular partner;
- adhere to the correct diet;
- use natural linen;
- avoid hypothermia;
- stop smoking;
- avoid stress.
Consequences of thrush in women
In the case of thrush, it is necessary to consider several options for the development of events:
- The patient promptly began treatment for acute thrush
. If a woman behaves correctly and follows all the recommendations of specialists, she can quickly get rid of thrush completely. Modern drugs are characterized by high efficiency and few side effects.
- Acute thrush was treated incorrectly and untimely
. Constantly postponing a visit to the doctor and subsequently failing to comply with his recommendations determine the likelihood of the disease becoming chronic. In this case, treating the disease is much more difficult, and the complications are much more serious.
Complications of chronic thrush
According to statistics, in almost 70% of cases, the chronic course of the disease leads to the development of some complication:
- Adhesive process of the pelvic organs;
- Obstruction of the fallopian tubes due to the development of adhesions;
- Infertility is a consequence of the development of tubal obstruction or ovarian damage;
- Decreased immunity of the body, which leads to frequent development of infections;
- If a woman is pregnant, then fungi can still infect the fetus in utero;
- Transition of the disease to other pelvic organs - bladder, rectum;
- If the pathogen enters the bloodstream, it is called candidiasis sepsis.
Is thrush transmitted to men?
Normally, a man’s body constantly encounters the same fungi as a woman’s. Since they are contained in the vagina of most women, the partner’s genitals in any case come into contact with the causative agent of thrush. A man can also develop candidiasis of the genital organs, which has approximately the same manifestations and causes as in women. Therefore, if a man has a reduced immune system, has diabetes mellitus or other prerequisites, then he can easily become infected with thrush. Moreover, a sexual partner can bring a large amount of fungus into a woman’s body, which will trigger the development of the disease.
Thus, thrush is transmitted to a man only if he has the prerequisites for its development and does not observe basic rules of personal hygiene. In the end, it is much easier for a man to remove all pathogens from the surface of the penis by simply washing it thoroughly, unlike a woman. And sexual intercourse itself in the presence of candidiasis is a rash action, contrary to the recommendations of doctors and is unlikely to bring pleasure
How to treat your husband for thrush?
Treatment of a spouse or partner is carried out according to the same scheme as for a woman. For therapeutic purposes, drugs for internal use are used, for example, Pimafucin 100 mg 4 times a day. The treatment cycle is 10 days.
Most often, candidiasis in men is asymptomatic. If visible signs of illness appear, you should undergo a thorough examination to identify an infection that reduces immunity. Such pathologies include hepatitis B, C, HIV infection, AIDS, acute leukemia.
Treatment
To remove the fungus, it is necessary to boost immunity and cure chronic diseases that weaken the defenses. An important role is played by the restoration of the normal microflora of the body. How to treat candidiasis? Doctors prescribe:
- immunomodulators;
- vitamins C, group B;
- for local use - antimycotic vaginal suppositories, ointments;
- inside – antifungal capsules, tablets;
- proper nutrition;
- restriction of sexual contacts;
- disinfection of linen;
- performing hygiene procedures;
- treatment of the sexual partner.
What kills candida in the body
In order for the body to get rid of the infection, it is necessary to act on the fungus. Medicines with a fungicidal effect, which damage bacteria and spores of microorganisms, help to cope with pathology. Dermatologists prescribe:
- inside the vagina - suppositories Livarol, Lomexin;
- for external treatment – Clotrimazole ointment, Triderm cream;
- if nail fungus is detected - Fungoterbin, Diflucan;
- if the intestinal walls or respiratory organs are damaged, take Fluconazole or Nystatin tablets orally.
Medicines
In the presence of a disease, when the cause of infection is a fungus, therapy involves the use of medications. Their action solves various problems. Doctors prescribe:
- Candide - the active ingredient clotrimazole, available in the form of cream, powder, solution, treats fungus on the skin, genitals, and mouth;
- Pimafucin – has antifungal and antiviral effects, effective against thrush;
- Linex is a probiotic, restores microflora and bacterial balance;
- Viferon - activates the immune system, prevents cell division.
Food
To destroy the fungus in the body, you need to eat right. You should eat more leafy greens, lentils, and beans. There is cabbage, zucchini, bell peppers, and fresh fruit. It is necessary to exclude products that cause fermentation, contain yeast and substances that provoke fungus:
- refined sugar;
- baking from yeast dough;
- pickled preparations;
- wine;
- beer;
- vinegar;
- sauces;
- mushrooms;
- smoked fish;
- fruit juices;
- grape.
Diagnosis of thrush
For an accurate diagnosis and drawing up a complete clinical picture, the doctor must have not only test results, but also draw conclusions based on examination data. When going to see a gynecologist, a woman will have to answer a number of questions. You need to be prepared for this and, if possible, provide the most complete and reliable information that will help the doctor.
The specialist may ask:
- What symptoms are you worried about? It must be described in all details.
- When were the first manifestations of the disease noticed?
- Have the signs of the disease changed since its onset? If yes, then how.
- What is the nature of the discharge? Color, smell, abundance, consistency, all the details are important.
- What causes increased symptoms? If the condition worsened, what caused it? When and for what reasons does relief occur?
- Have you had symptoms before?
- Have you or have not had to be treated for sexually transmitted diseases?
- How active is your sex life? How many sexual partners?
- How and with what do you protect yourself?
- Has your partner noticed any discharge from the penis?
- What medications have you taken recently? If antibiotics were prescribed, which ones?
- How many days does menstruation last? What is their regularity?
- Have you ever used douching or not?
- Do you have any chronic diseases? If there were in the past, which ones?
After collecting the necessary information, the doctor examines the patient. A smear of the cervix and vaginal mucosa is taken. Microscopic examination of a smear can reveal fungal mycelia. This examination method is considered more informative, since it is impossible to recognize the type of fungal infection that caused thrush.
Bacterial inoculation of a smear on special nutrient media allows you to find out which fungus provoked the disease. The sensitivity of the identified colonies and their susceptibility to antifungal drugs are determined. The quantitative factor is also very important. A small number of colonies is considered normal for healthy vaginal microflora.
All ongoing research by specialists indicates a connection between thrush and other sexually transmitted infections. In most cases, candidiasis occurs in a complex manner, with the symptoms of thrush masked by hidden infections. There has been a trend of their growth and widespread distribution in recent decades. This is why doctors recommend a differential method for diagnosing thrush. This will reveal the presence of diseases such as gardnerellosis, gonorrhea, trichomoniasis, genital herpes, and ureaplasmosis. A visit to a venereologist and taking the necessary tests makes it possible to confirm or exclude the presence of dangerous infections and draw up the correct treatment plan for thrush.
A comprehensive examination for chronic candidiasis helps to identify diabetes mellitus. The first symptom of this serious disease is thrush. If tests show that blood sugar is higher than normal, the woman is advised to consult an endocrinologist and follow his recommendations.
The participation of a gastroenterologist is also important. To effectively treat candidiasis, an abdominal ultrasound may be necessary. Most likely, you will need to take a stool sample and check your intestines. If there are indications, FGS and other diagnostic measures are prescribed.
If thrush causes complications in the urinary system, you need to visit a urologist, undergo an examination and take the necessary tests (ultrasound of the bladder and kidneys, urine analysis according to Zimnitsky, smear from the urethra).
When should you definitely contact a gynecologist?
- Relapses of candidiasis are observed more often than 4 times a year.
- Treatment for a week does not produce results and does not relieve symptoms.
- If, after taking prescribed medications, irritation appears in the genitals.
- In cases where the temperature rises due to thrush, weakness is felt, and pain in the lower abdomen begins to bother you.
- In case of relapse of candidiasis after a course of treatment.
- If blood and purulent discharge appears during treatment. Brown discharge in the middle of the therapeutic cycle is especially dangerous.
Will folk remedies help?
Folk remedies for candidiasis can only provide temporary relief; they cannot fight the causes of the disease. Traditional methods should be used exclusively as auxiliary and only on the recommendation of a doctor.
For vaginal candidiasis, you can wash yourself with a weak soda solution, water with the addition of tea tree oil, eucalyptus, or chamomile decoction (douching is not recommended, especially for expectant mothers). You can use the same products to rinse your mouth if candida has become active in it, or wipe the skin affected by the fungus. For intestinal candidiasis, you can drink a decoction of wormwood root or tincture of juniper fruits.
How to treat thrush in women?
If the disease is mild and the woman seeks help in a timely manner, doctors try to make do with local medications. These are tablets, creams or suppositories that are inserted into the vagina. There they quickly reach their destination and begin to act.
At the first symptoms
At the first symptoms of the disease, it is advisable to prescribe a specific treatment regimen:
- Clotrimazole in the form of suppositories 200 mg. 1 candle at night for 14 days.
- Fluconazole - 150 mg tablets. The drug is taken one tablet on days 1, 4 and 7 of treatment. Or Itraconazole tablets 200 mg - 1 tablet for 7 days.
- After two weeks of treatment, a course of probiotics is recommended to restore intimate microflora.
Video: Dr. Evdokimenko “How to cure thrush in women and men? Simple tips, effective remedies"
With a mild form
To treat candidiasis in a mild and uncomplicated form, you can use topical medications:
- Clotrimazole (Candizol, Kanesten, Candibene, Yenamazole 100, Antifungol). For 14 days, use 1 vaginal suppository.
- Miconazole (Gyno-daktarin, Ginezol 7, Klion-D 100). Has antifungal and antibacterial effects. Use 1 suppository in the vagina at night. The course of treatment is 14 days.
- Isoconazole (Gyno-travogen). The drug affects the permeability of fungal cell membranes. It has an antifungal effect and can eliminate symptoms of inflammation and itching. It has a good effect on types of fungi that are resistant to other antimycotics. For treatment, 1 suppository is inserted deep into the vagina at night. Course - 3 days.
- Fenticonazole (Lomexin).
- Fluomizin.
Read more about the treatment of uncomplicated thrush
In chronic form
In the chronic form of thrush, along with specific drugs, antibacterial and restorative agents are prescribed:
- Fluconazole. Analogues - Diflucan, Flucostat.
- Itraconazole Analogues - Kanditral, Irunin, Rumikoz, Itrazol, Orunit.
- Pimafucin (Natamycin) has virtually no toxic effect. Let's say during pregnancy. Destructive for various types of fungi. Suppositories are inserted into the vagina before bedtime. The course is 3-6 days, treatment is continued even after improvement.
- Ketoconazole. Analogues - Fungavis, Oronazole, Nizoral.
Read more about the treatment of chronic thrush
Features of treatment during pregnancy
The first three months of pregnancy are the most dangerous period for prescribing any medications. At this time, the laying of organs and systems of the fetus occurs. Thrush is rarely diagnosed in the first trimester, since the level of hormones is controlled naturally, and the protective functions remain at the same level.
For treatment in the first trimester, one of the following is used:
- Pimafucin - 1 suppository at night, for 6 days.
- Betadine - 1 suppository before bedtime, for 6 days.
For thrush in the second and third trimester, it is permissible to use other, more active antifungal drugs. The antimycotic course may consist of:
- Pimafucin - 6 suppositories.
- Betadine - 6 suppositories.
- Clotrimazole - 7 suppositories.
- Gino-Pevaril - 6 suppositories.
- Gynofort - vaginal applicator, 1 time.
Candidiasis during pregnancy requires full treatment. An improvement in the woman’s condition with the disappearance of symptoms occurs 2-3 days after the start of treatment. This does not mean that therapy should be stopped. It is important to complete the full course of treatment to avoid exacerbations and return of symptoms.
More details:
thrush during pregnancy and lactation
You might be interested:
- The best suppositories against thrush (pros and cons of each company)
- How to get rid of thrush at home?
- Treatment with folk remedies
It is important to initially treat only with antifungal drugs, since broad-spectrum substances can provoke the development of other infectious diseases due to the complete destruction of the flora.
Treatment of thrush accelerates the intake of vitamins and minerals. This normalizes the intestinal microflora and strengthens the immune system. It is recommended to take pribiotics and vitamin-mineral complexes.
Antifungal drugs in gynecology for local use:
| Drug name | Active substance |
| Zalain (vaginal suppositories) | Sertaconazole |
| Candizol, Antifungol, Canesten, Clotrimazole, Candibene, Yenamazole 100, Candide B6 | Clotrimazole |
| Gyno-pevaril and Ifenek | Econazole |
| Ovulum, Gyno-travogen | Isoconazole |
| Klion-D 100, Gyno-daktarin, Ginezol 7, Micogal | Miconazole |
| Lomexin | Fenticonazole |
| Pimafucin | Natamycin |
| Polizhinaks, Nystatitn, Terzhinan | Nystatin |
| Nizoral, Livarol, Mycozoral, Ketoconazole, Oronazole, Brizoral, Vetorozal | Ketoconazole |
Antifungal drugs for systemic use:
| Drug name | Active substance |
| Fluconazole | Flucostat, Mikomax, Enalapril hexal, Diflazon, Mikosist, Mikoflucan, Diflucan, Ciskan. |
| Itraconazole | Irunin, Orungal, Itrazol, Orunit, Rumikoz, Kanditral |
| Ketoconazole | Nizoral, Mycozoral, Fungavis, Oronazole |
| Nystatin tablets | |
| Pimafucin tablets |
Side effects.
Taking antifungal tablets may cause side effects. The digestive system is the most vulnerable. Possible diarrhea, nausea, flatulence, unpleasant painful sensations in the abdomen, impaired liver function, and changes in taste.
Side effects associated with the nervous system manifest themselves in the form of allergic reactions, seizures, headaches and dizziness. The most common and serious complications are caused by drugs that contain Itraconazole.
Most oral antifungal agents should not be taken during lactation and pregnancy, in case of liver dysfunction, renal failure and hypersensitivity. Antifungal agents are prescribed only in cases where local treatment is not enough and complex therapy is required.
What to do to prevent thrush from recurring?
To prevent relapse of the disease, adhere to the following measures:
- The prescription of a systemic antifungal agent is 200 mg of Itraconazole or 150 mg of Fluconazole on the first day of menstruation for 6 months.
- Vaginal suppositories for local use for 6 months, once a week.