- Etiology
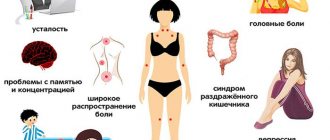
- Symptoms
- Diagnostics
- Treatment
Peeling of the skin is a symptom of a certain pathological process or vitamin deficiency, which manifests itself in the form of an excessive number of dead epidermal cells. In addition, peeling of the skin can be caused by severe dryness. Prolonged manifestation of such a symptom is the basis for a medical examination. Unauthorized use of drugs or traditional medicine can provoke the development of serious complications.
General information
Peeling of the skin is a natural process of renewal of the surface layer due to the rejection of the keratinized layer of the epidermis.
The desquamation of horny scales (terminally differentiated keratinocytes) from the surface of the epidermis occurs constantly, due to which the skin is cleansed of pollution and biological pathogens. Horny scales consist of a substance of albuminoid nature ( keratin ). The rate of epithelial renewal averages 28 days. The constant renewal of the epidermis is due to specific changes in keratinocytes during their differentiation and migration from the deep layers to the outer ones: from the basal layer to the spinous, granular and stratum corneum, which is represented by thin, anucleate dead cells tightly adjacent to each other (Fig. below).
The process of keratinization in epidermal cells is quite complex and ends with the deposition of a protein substance (keratin) and fats in the stratum corneum. In the epidermis, a dynamic balance is normally maintained between the proliferation of basal keratinocytes and the number of exfoliated horny scales. Thus, the homeostasis of the epidermis of the skin is ensured by such processes as:
- Cellular renewal.
- Targeted migration of keratinocytes in the epidermal layer.
- Cytodifferentiation with transformation of keratinocytes into corneocytes .
- Death of corneocytes (keratinization/apoptotic death).
- Desquamation of corneocytes from the surface of the epidermis.
The process of corneocyte desquamation (desquamation) is determined by two factors: mitotic activity (intensity of cell production) and the state of the intercorneocyte cement, which ensures adhesion (sticking) of corneocytes to each other. between mitosis adhesion strength . That is, the higher the intensity of cell reproduction, the lower the adhesion force of corneocytes. However, under the influence of various factors, this ratio may be disrupted.
During normal physiological processes in the skin, the stages of keratinization and peeling of the epidermis occur almost imperceptibly according to the type of soft keratinization, when the most superficial corneocytes, by desquamation of horny scales, “leave” from the surface of the skin and are replaced by keratinocytes that have gone through all stages of differentiation. That is, the body maintains a “fine” balance between the processes of desquamation of the stratum corneum and basal cell proliferation. However, under the influence of various exogenous and endogenous factors, the keratinization process may be disrupted, which is manifested by increased peeling of the skin. In 85% of cases, excessive peeling occurs against the background of increased dryness and is accompanied by increased skin irritability, a feeling of tightness, itching, and pain when cracks occur. Dryness and flaking of the skin can be either local (on the face, feet, ears, head, etc.) or general, depending on the reasons that caused them.
Dry skin with excessive peeling (pathological desquamation) can be caused by both banal reasons (improper skin care, adverse effects of menopausal factors, work in environmentally hazardous industries, poor diet, etc.), and indicate skin aging, hormonal changes, and also serve as a clinical symptom of a number of dermatological, endocrine diseases and pathologies of internal organs.
Thus, the symptom complex of excessive peeling and dry skin is a heterogeneous concept that includes various physiological and pathological conditions of the skin. Pathological desquamation associated with dry skin syndrome is a condition that significantly reduces the quality of life. And even without being a symptom of any disease, but having developed as a result of the negative impact of external factors or skin care disorders, it can eventually result in the formation of clinically pronounced dermatitis .
Prevention of hand diseases
Dry skin on the palms of the hands can become a gateway for bacteria if cracks form on it, so preventive measures to prevent infection must certainly include moisturizing and saturating the skin with nutrients. Preventing the appearance of eczema is much easier than treating it, so it is advisable for allergy sufferers to refrain from consuming prohibited foods.
Dry eczema will not occur if you regularly take care to protect your hands from aggressive substances that a person comes into contact with due to the nature of their work. To do this, you need to use gloves, preferably thin disposable ones, and additionally lubricate your hands with a cream containing silicone. This substance is easily washed off with soap and water and does not allow harmful substances to penetrate through it.
Pathogenesis
The main cause of pathological dry skin and desquamation of the epithelium is impaired hydration of the stratum corneum of the epidermis. The leading pathogenetic mechanisms of dry skin are:
- A decrease in the skin's ability to retain moisture due to a deficiency of hygroscopic substances inside corneocytes - natural moisturizing factor (NMF), which is a breakdown product of the filaggrin . With the participation of the enzyme peptidyl deaminase, the proteolytic breakdown of filaggrin occurs, and a multicomponent structure is formed in the stratum corneum, which forms the hydrolipid mantle of the skin (free amino acids, urea derivatives, lactate compounds, lactic and polycarboxylic acids, metal ions and other components) that bind and store water in corneocytes. It is this water that is the main moisture of the stratum corneum. The process of filaggrin breakdown and the effect of NMF components (urea, glycidine, glutamine) on the skin is schematically presented below.
- A decrease in the barrier function of the stratum corneum due to the failure of the lipid component (violation of their location and structure), which causes defects in the intercellular lipid layers and leads to a sharp increase in transepidermal moisture loss. It is the change in the composition of epidermal lipids that underlies the formation of inferiority of the protective hydrolipid layer, which leads to extensive loss of water and facilitates the penetration of irritants and allergens.
- Disruption of the process of transporting moisture from the dermis to the stratum corneum of the epidermis. The pathogenesis of peeling (desquamation) is based on pathological changes in the rate and order of destruction of corneodesmosomes in the stratum corneum of the skin, which affects the condition of the skin (thickness of the stratum corneum, peeling, dryness). Regulation of desquamative processes is controlled by many factors: exogenous/endogenous proteases, skin pH , activity of protease inhibitors, properties of corneodesmosomal proteins, external factors of aggression. A special role in the control of desquamative processes is given to protease inhibitors, which are secreted in the lamellar bodies of the granular layer (SLPI, SKALP, LEKTI, plasminogen activation inhibitor, etc.) and metal ions, in particular zinc. It is defects in protease inhibitors that lead to structural disturbances in corneodesmosomes, which contributes to the formation of defects in the process of desquamation of the stratum corneum of the skin.
Thus, impaired differentiation and proliferation of the epidermis, as well as the inability of the stratum corneum to retain moisture, underlie the mechanism of development of dry skin, pathological desquamation (flaking) and changes in skin texture.
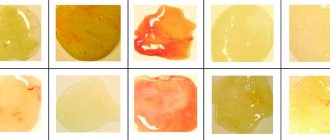
Fungal diseases
If you notice that the skin on your fingers has begun to peel off very much, the nail plates have become yellow and are also peeling off (as in the photo below), then most likely it is a fungus. You can “pick up” this insidious enemy anywhere: in the pool, in public transport, while using objects that were previously used by a person infected with the fungus. Treatment of the problem in this case is complex - you will have to take antifungal drugs, use medicinal ointments, and make special baths. Seeing a doctor is mandatory.
Presence of parasites in the body
Helminths and other parasites have a destructive effect on all systems of the human body. They weaken a person’s immunity and undermine his health. The waste products of parasites poison the body and lead to side diseases. The person feels tired, loses weight and appetite. In this case, not only fingers, but also nails, hair, and teeth are affected. If you suspect you have helminths, then be sure to get the appropriate tests and undergo a course of antiparasitic therapy. You should not self-medicate and rely only on creams and folk remedies against peeling fingers.
Classification
Based on etiopathogenetic characteristics, several groups of dry skin accompanied by excessive peeling are distinguished:
- Acquired. Associated with the impact of harmful environmental factors on the surface layers of the skin.
- Constitutional. At the same time, dryness and flaking of the skin are caused by genetic mutations leading to functional/structural disorders in the surface layers of the epidermis. For example, mutations of the FLG gene, which is responsible for the synthesis of filaggrin (filament-aggregating protein). Its deficiency leads to a disruption in the structure of the natural moisturizing factor (NMF), respectively, to transepidermal water loss from the skin.
- Dry skin and flaking due to age-related changes. There are several such periods: from the first day of a newborn and for 15-30 days after the birth of a child (in infants), which is due to the removal of caseous lubricant and a decrease in swelling of the skin. The second period (in a child from 4 to 8 years old), since during this period there is minimal activity of sex hormones ( cortisol , estrogen , testosterone , progesterone ), which is accompanied by a decrease in the production of sebum by the sebaceous glands. And the third period is old age (after 70 years), which is explained by involutional dystrophic processes in the skin and a reduced content of sex hormones, which leads to a decrease in the function of the sebaceous glands.
Causes of peeling skin
The leading cause of dry and flaky skin is insufficient moisture content in the stratum corneum of the skin. There are exogenous and endogenous causative factors that cause dryness and excessive peeling of the skin.
Exogenous causes (external triggers) include harmful environmental factors:
- Climatic conditions that adversely affect the skin (long stay in the cold, insolation, poor water quality, swimming in chlorinated water, dry air and high temperatures, industrial air pollution, strong wind).
- Change of time zones.
- Incorrect/inappropriate skin care - gels, soaps, cosmetics inappropriate for the skin type, frequent hot baths, contact with detergents (hygienic detergents, especially those with a high alkali content), use of aggressive cosmetic procedures: clay-based masks, peeling, laser resurfacing, etc. d.
- Harmful professional/domestic contacts with chemically aggressive substances (aeropollutants, tobacco smoke).
Endogenous factors that cause dryness and flaking of the skin include:
- Dermatological diseases: psoriasis , dry eczema , seborrheic dermatitis , keratosis pilaris , ichthyosis , pityriasis rosea .
- Infectious and allergic diseases (atopic/contact/ allergic dermatitis ).
- Hormonal imbalance ( hypothyroidism , diabetes mellitus , intestinal malabsorption ).
- Improper diet with insufficient vitamins (hypovitaminosis/ avitaminosis ) and minerals (calcium, copper, selenium, zinc), as well as sudden weight loss caused by dietary restrictions (mono-diets).
- Long-term use of certain medications (topical corticosteroids, alcohol-containing solutions, azelaic acid , benzoyl peroxide , retinoids , etc.). And long-term use of vitamins ( nicotinic acid ), diuretics and statins generally contributes to the development of generalized dry skin.
- Diseases of internal organs (chronic renal failure , hepatitis , cirrhosis , intestinal diseases, hematological and oncological diseases).
- Physiological conditions - aging of the body, which is accompanied by dehydration of the skin and changes in hormonal levels (about 75% of people over 70 years old have dry skin and peeling). Dry skin and flaking are especially characteristic of women during menopause , when, due to the reduced production of female sex hormones, the function of the sebaceous glands decreases and the production of sebum slows down. As a result, the skin becomes dry, peeling and irritation appear.
After identifying the main causes of dry skin, we will consider the relationship between local peeling of the skin (including pathological desquamation) and etiological causes. The most common reasons why the skin on the face peels is unfavorable meteorological conditions, which mainly affect exposed areas of the body. This may appear over time as mild flaking or as severe flaking and redness of the skin.
Often, as a reaction to unfavorable climatic conditions, the skin on the face peels off locally in one or another part of the face: the skin on the forehead or around the eyes peels off. Also, under the influence of wind and frost, sea water and ultraviolet radiation, the skin on the eyebrows of men can peel off. However, if there is peeling on the eyebrows, it is necessary to exclude demodicosis .
Peeling is often present on the nose or around the nose, which often happens with a long runny nose, when you have to blow your nose frequently, irritating the skin of the nose.
One of the reasons that causes skin irritation in men is shaving, especially with an insufficiently sharp razor, which leads to peeling of the skin on the face and especially on the chin (the skin also turns red on the chin). The leading reason why the skin on the face peels in women is improper skin care, abuse of cosmetics and rough methods of cleaning the skin.
Daily contact of the skin of the hands with substances that destroy the epidermal barrier (surfactants included in household detergents/cleaning products) is often the reason why the skin on the hands peels. At the same time, peeling can be on the palms of the hands, on the fingers or between the fingers (Fig. below).
In advanced cases, the skin of the hands peels and cracks, forming painful cracks, especially on the palmar surfaces; less often, the skin cracks and peels off in flakes.
The skin on the hands can peel for other reasons: vitamin deficiency, dermatitis of various etiologies. Especially often, severe peeling of the skin on the palms of the hands is observed when the skin comes into contact with harmful, aggressive substances at work or at home ( contact dermatosis ). Also, the skin on the fingers and palms of the hands becomes very peeling with palmoplantar psoriasis. But at the same time, the skin of the feet also suffers - the skin on the feet is dry and flaky, mainly on the soles of the feet, on the plantar part.
There could be other causes of peeling skin on the fingers, in particular, fungal diseases of the skin of the fingers involving the nail plates in the pathological process.
The cause of excessive dryness and flaking of the skin on the elbows may be constant contact with hard surfaces that locally injure this area of the skin (when working in an office, at a computer), dehydration, wearing rough/synthetic clothing, hypovitaminosis, endocrine diseases ( hypothyroidism , diabetes mellitus ) , iron deficiency anemia , eczema , psoriasis and others.
Quite often, patients complain that the skin on their legs is dry or the skin on their legs is peeling, mainly in the area below the knees. The most common cause of peeling skin on the soles of the feet and between the toes is: contagious dermatosis of the skin ( epidedmophytosis pedis ), which mildly manifests itself in the form of mild itching with erythematous-flaky lesions in the folds between the toes. of erythema appear on the toes and between the fingers , accompanied by pain, itching, and a pronounced feeling of tension.
In some cases, a red scaly spot initially appears on the skin ( pityriasis rosea , psoriasis , atopic dermatitis , etc.); in some diseases, the red spots do not itch, but simply flake off.
Another problem area is the skin on the scalp (the scalp, in the auricle and behind the ears). The skin on the head can peel for a variety of reasons, ranging from frequent washing with incorrectly selected hair detergents that have an aggressive effect on the skin or an allergic reaction to various cosmetics used for styling and coloring hair.
Severe flaking of the scalp is often one of the symptoms of a disease ( seborrheic dermatitis , caused by the yeast Malassezia), in which there is an accelerated formation of yellowish oily hair scales along the growth line, accompanied by occasional itching. Peeling of the skin on the scalp in an adult is also observed with psoriasis of the scalp, in which the scalp is severely flaky and comes off in flakes. In this case, the skin behind the ears in adults is often involved in the process.
Dry skin and flaking in the ears can be either a manifestation of a reaction to various types of unfavorable factors (weather conditions, hygiene products), or be one of the signs of the disease. Peeling of the skin in the ears is often one of the symptoms of a fungal infection of the skin of the ear canal or a manifestation of an allergic reaction ( allergic dermatitis ) to various allergens.
Much less common are complaints about peeling skin on the genital organs - on the penis, the skin of the scrotum (the incorrect expression is peeling on the “testicles” or “on the balls”), on the labia and in the “bikini” area in women. The skin on the penis can peel for a variety of reasons. These may be symptoms of inflammation of the glans penis ( balanitis ) or inflammation of the foreskin ( balanoposthitis ), a manifestation of genital herpes . The reason that the skin on the labia peels can be candidal vulvitis / vulvovaginitis , dysfunction of the endocrine system (hormonal imbalances / age-related changes).
In addition, in both men and women, peeling of the skin on the genitals may be a consequence of poor intimate hygiene or the use of highly chlorinated water for this purpose; special products to which there may be a local allergic reaction; wearing tight underwear, especially made of synthetic fabrics, lack of vitamins E , C and B ; reaction to long-term use of antibiotics or vitamin A ; frequent depilation procedures and hair in the bikini area, which provoke redness and peeling of the epidermis and others.
Unfortunately, it is impossible to unambiguously determine the causes of dryness and excessive flaking of the skin locally or in general. In each specific case, a thorough examination of the patient and laboratory tests are necessary.
Chemical exposure
If your hands regularly come into contact with products that contain acid or alkali, then the appearance of peeling is a matter of time. First, pimples appear on the skin of the fingers, which soon burst and lead to peeling of the upper layer of the epidermis. How to protect yourself in this case:
- It is necessary to use special rubber gloves when working with caustic substances.
- For washing dishes and other household needs, it is better to use gentle, natural-based detergents.
- After unprotected contact of hands with chemicals, it is necessary to apply a protective cream to them.
- It is better to use a brush, brush and other tools instead of a rag, where possible.
If a burn occurs as a result of skin contact with chemicals, it is better to immediately consult a doctor without self-medicating.
Symptoms
Clinical manifestations are: excessive peeling against the background of dry skin, roughening ( lichenification )/thinning of the skin, the appearance of small cracks, decreased skin turgor and elasticity due to lack of water and lipids. Patients may be bothered by mild itching, burning, a feeling of tightness and increased irritability of the skin. In cases of various dermatological, endocrine diseases and pathologies of internal organs, dry skin and excessive peeling may be just one of the symptoms among the various manifestations of the disease.
There are several stages of clinical manifestation:
- First degree. Dry skin is not constant, there may be slight flaking and a slight feeling of skin tightness. Typically, these symptoms quickly disappear with the use of moisturizers.
- Second degree. A constant feeling of dryness and tightness of the skin, visually noticeable fine-plate peeling, small wrinkles appear. The skin becomes sensitive, irritation and peeling may appear even with mild exposure to physical/chemical irritants or under the influence of minor negative environmental factors. Using cream does not completely solve the problem.
- Third degree. Severe dry skin, the presence of large-plate peeling, possible itching and erythema, with deepening cracks in the skin. Wrinkles. Emollients/moisturizers are not very effective.
- Fourth degree. Severe large-plate peeling, accompanied by degenerative changes in the epidermis/dermis.
Allergic reactions to cosmetics or hygiene products
Unfortunately, most cosmetic and hygiene products contain aggressive allergens, which cause allergic manifestations in the form of itching, burning, and peeling of the skin. Before using a new hand cream, lotion or elixir, it is recommended to first apply a little product to your wrist and leave for half an hour. If there are no changes, then you can use this cosmetics without fear.
You should choose soft and gentle cosmetics that support the protective function of the skin and do not disrupt its lipid metabolism. It is better to purchase creams, gels and shampoos without parabens and sulfates.
Treatment. What to do if your skin is peeling?
It is necessary to clearly distinguish between the treatment of flaking and dry skin in physiological and pathological skin conditions. Let us consider only the principles of treatment of physiologically normal skin. It should be said that the principles of care and treatment of peeling of physiologically normal skin that manifests itself locally (for example, treatment of peeling skin on the elbows, face, fingers, and so on) are not fundamentally different. Accordingly, consider separately the questions “what to do if the skin on the face or elbows, around the nose, etc. is peeling.” doesn't make sense. First of all, all patients with dry, excessively flaky skin are recommended to:
- Maintain a drinking regime with the consumption of clean water in a volume of at least 2.0 l/day (in the absence of contraindications), which allows the body not only to obtain the required amount of fluid, but also to accelerate the elimination of toxins/impurities that negatively affect the condition of the skin.
- Balance your diet by enriching it with fruits and vegetables. Periodic intake of vitamin and mineral preparations.
- Eliminate the adverse effects of environmental factors (exposure to cold, wind and sun, prolonged contact with detergents, water, avoid staying in rooms with low levels of air humidity, taking hot baths, etc.).
- Special skin care using products for protection, skin cleansing, replacement (moisturizing) external therapy preparations that effectively restore the water-lipid balance and help soften and moisturize the skin.
The main groups of substances that have a moisturizing effect are humectants and occlusive agents . The first group includes agents that attract and bind water in the surface layers of the skin. They are based on the components of a natural moisturizing factor: urea (at a concentration of up to 10%), glycerin, transurocanine, hyaluronic, lactic and pyrrolidonecarboxylic acid, sodium lactate, potassium lactate, propylene glycol, sodium cirrolidone carboxylate and others. Such preparations, as an example, include: Edel cream , Argalan cream mask , Liftofin , Balzamed and Balzamed intensive , preparations (emulsions, milk, cream) of the TOPICREM SOS line and others.
Reducing transepidermal water loss is achieved through the use of occlusive agents containing lipid compounds, which effectively prevent drying of the skin, soften it and make it elastic due to the formation of a surface water-repellent film. For this purpose, it is preferable to use natural products (vegetable oils and animal fats - grape seed oil, fish oil, lanolin, beeswax, etc.), since the vast majority of natural fat-soluble substances of plant and animal origin correspond to the composition and concentration of skin lipid compounds.
Moreover, natural fatty compounds have another profound effect - they saturate the skin with fatty acids, ceramides and other compounds that are actively built in the epidermis. These products include Bepanten , which can effectively get rid of flaking and can be used to moisturize the skin of children. For severely dry skin accompanied by desquamation, Keratosan Xemoz Uriage cream , which are applied after cleansing the skin.
Management of patients with sensitive dry flaky skin includes individual selection of skin care products that improve skin hydration, reduce damage to the lipid/protein component of the stratum corneum and accelerate the process of its repair. Use only care products that do not contain dyes, fragrances, or parabens (preservatives).
In case of severe peeling and dryness of the skin, for example, if the skin of the face is very peeling, before applying products that improve skin hydration, it is necessary to pre-clean it, for which you can use special (alcohol-free) lotions, creams or emulsions - cold creams and non-ionic detergents. You should completely avoid regular soaps and standard cleansers, as they can dry out your skin even more. All care products should be designed for dry skin (GARNIER micellar water with natural oils, LA ROCHE-POSA cleansing cream-gel for dry skin, Uriage Mustela Stelatopia cream and others).
It is recommended to purchase and use not just one skin care and treatment product, but an entire set (series) for the care of dry, flaky skin from one manufacturer, since they complement and enhance each other’s effects. After water procedures, the skin should not be roughly wiped; it is better to blot it with a soft towel.
Patients with dry skin must always use daytime protective creams before going outside. In summer, you should use creams with an spf filter containing a sunscreen component. Also, be sure to moisturize your skin after sunbathing.
Medicinal products for external treatment of skin diseases (dermatitis, eczema, psoriasis), accompanied by dryness and flaking of the skin, are selected exclusively by a dermatologist individually.
Procedures and operations
For dry, flaky skin, peelings (mechanical, chemical, hardware), biorevitalization (injections of hyaluronic acid , which has a pronounced moisturizing effect), collagen masks, salon procedures for active moisturizing and nourishing the skin are recommended.
Peeling skin in children
Often parents are concerned about the question “why the skin of a newborn baby is peeling.” Peeling of the skin in children of the first month on the hands or face is a natural phenomenon caused by the adaptation of the skin to new living conditions (contact with air, water, clothing) and, as a rule, passes quickly. A common cause of flaking in infants is dry air in the home during the heating season, improper skin care (bathing with the addition of potassium permanganate, bathing, using shampoos, milk, gels and other hygiene products to which allergic reactions develop), and rough wiping of the body.
The artificial material of the baby's clothing and low-quality dyes of the fabric in contact with the newborn's skin can also cause redness, itching and peeling of the baby's delicate skin. Often a newborn's skin on the body peels off due to active exposure to ultraviolet rays, reaction to cold or wind.
Peeling of the scalp in a child may be one of the signs of seborrheic dermatitis or simple overheating and fogging of the skin on the baby’s head when using out-of-season headwear. Often, a newborn’s skin peels due to an allergic reaction to food products, especially to various milk formulas when complementary foods are introduced.
cheilitis is also common in children , one of the symptoms of which is peeling of the skin around the mouth (peeling of the red border), caused by the bad habit of licking the lips. This leads to rapid drying of the mucous membrane of the lips and its subsequent peeling.
A more dangerous option is atopic cheilitis , which affects the red border of the lips and skin, especially intensely in the area of the corners of the mouth. The disease begins with the appearance of pink erythema, swelling and itching. After the acute inflammatory phenomena subside, lichenification of the lips occurs. At the same time, the red border of the lips becomes infiltrated and later peels off in small scales.
Parents often complain that the child’s skin behind the ear gets wet, and a little later the skin behind the ear becomes crusty. There are many reasons for a child’s weeping behind the ear, ranging from simple non-compliance with hygiene rules, overfeeding, high air temperature and sweating of the child’s head, an abundance of sweets in the diet, to eating foods that cause allergic reactions on the skin and dermatitis. In particular, weeping dermatitis localized on the skin behind the ears.
Nervous tension and stress
Each person reacts differently to stress: some people experience dry mouth, some people start to go bald, and some people get peeling fingers. If the state of stress is permanent, then there are disruptions in many body systems. If a person has not previously had allergic reactions, and after experiencing a shock the skin on the fingers begins to peel off, then the nature of this phenomenon clearly lies in stress. To get rid of this manifestation, it is necessary to remove the root cause - the source of anxiety.
Diet
Diet for skin diseases
- Efficacy: therapeutic effect after a month
- Time frame: three months or more
- Cost of products: 1400-1500 rubles per week
Diet for dermatitis
- Efficacy: Therapeutic effect after 3 weeks
- Timing: Constantly
- Cost of products: 1300-1390 rubles per week
There is no specially designed diet for physiologically normal flaky skin. A balanced diet is recommended, including unrefined vegetable oils, fish, chicken eggs, vegetables and fruits, garden herbs, nuts, as well as fortified drinks (rosehip infusion, oats, freshly prepared juices). Smoked, fatty, spicy and pickled foods/dishes, alcoholic drinks to which the skin reacts poorly are subject to restrictions.
For dry and flaky skin due to dermatological or endocrine diseases, appropriate diets are prescribed, for example:
- Diet for hypothyroidism of the thyroid gland.
- Diet for hormonal imbalance in women.
- Diet for dermatitis.
- Diet for psoriasis.
- Diet for eczema.
- Antifungal Diet.
- Hypoallergenic diet.
List of sources
- Trukhan D.I., Viktorova I.A., Bagisheva N.V. SKIN CHANGES IN SOMATIC DISEASES // International Journal of Applied and Fundamental Research. – 2021. – No. 8-5. – pp. 736-740.
- Studenikin V.M., Studenikina N.I. Skin care for children in the first years of life: neuropediatric aspects. Attending doctor. 2008; 3:66–70.
- Arabian E.R., Sokolovsky E.V. Dry skin. Causes and mechanisms of occurrence. Principles of correction // Journal of dermatovenereology and cosmetology. 2002. No. 2.
- Kuznetsov S. L., Goryachkina V. L., Tsomartova D. A., Zaborova V. A., Lutsevich O. A. Modern ideas about the structure and functions of the epidermis // Russian Journal of Skin and Venereal Diseases. 2013. No. 2. P.26 - 31.
- Lomakina E. A. The role of the barrier function of the skin in the pathogenesis of some dermatoses // Modern problems of dermatovenereology, immunology and medical cosmetology. 2009, no. 2. pp. 87–90.