Lymphedema is the accumulation of excess fluid between tissues. Most often, the disease affects the extremities (upper and lower). Lymphedema is associated with disruption of the function and integrity of the lymph nodes and vessels, which play the role of a filter in the body and are an important part of the immune system. Lymphedema leads to severe swelling of the arms and legs, which causes many problems: difficulty in moving, and the affected tissues are more susceptible to severe inflammation and infection. Treatment of the disease must begin at the first signs. In this case, the likelihood of inhibition and elimination of the pathological process increases significantly. Only a specialist can recognize lymphedema and prescribe adequate treatment.
Treatment of lymphedema in Moscow is performed at the Yusupov Hospital. There are doctors here who have extensive experience in eliminating such ailments. At the Yusupov Hospital, lymphedema is treated using effective therapy methods that help improve the patient’s condition and restore the functioning of the body’s systems.
How does lymphedema occur?
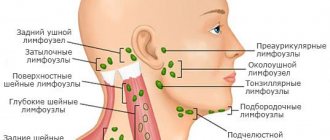
The lymphatic system is a network of lymphatic vessels passing throughout the body, the functionality of which is expressed in the collection of excess fluid rich in protein, lipids and products of cell metabolism. The fluid enters the lymph nodes, which contain cells of the immune system that respond to pathogenic cells - their own or foreign. Excess fluid is released back into the bloodstream. If the lymphatic vessels are blocked or are unable to drain fluid from the tissues, local swelling of the soft tissues—lymphedema—is formed.
Pathogenesis of lymphedema
Lymphedema is caused by impaired lymph transport. The function of the lymphatic vessels is to drain fluid from the capillaries that accumulates in the interstitial tissue to maintain constant interstitial pressure. Venous capillaries reabsorb 90% of interstitial fluid, the remaining fluid is transported into the blood by lymphatic ducts in the form of lymph. Under normal conditions, the same amount of fluid is transported into the interstitium as out of it. This balance is disrupted in lymphedema due to deterioration of lymphatic transport capacity, leading to fluid accumulation in the interstitial tissue and edema.
Causes of pathology
Lymphedema is divided into primary and secondary, based on the causes of its occurrence. The primary one is a congenital anomaly, in turn, the appearance of secondary lymphostasis can be caused by:
- formation of tumors of the lymphatic system;
- injuries, including burns, radiation, etc.;
- damage during surgery;
- physical inactivity;
- chronic pathologies leading to venous insufficiency and stagnation of lymph in the extremities;
- infections (parasitic and staphylococcal);
- erysipelas on legs;
- obesity;
- surgeries in the thoracic area related to oncology.
The pathological condition can be localized in various parts of the body:
- lymphedema of the lower extremities;
- lymphostasis of the hand;
- lymphedema of the foot, etc.
Lymphodermatitis and lymphodermatosclerosis may also occur.
Treatment
The goal of conservative treatment for lymphedema is to improve the contractile function of the lymphangion (a structural unit of the lymphatic system, consisting of a muscular cuff, the wall of the valvular sinus and the area of valve attachment. – editor’s note), improve the motility of the lymphatic vessels and tissue oxygenation, the rheological properties of the blood, and prevent erysipelas inflammation and trophic ulcers.
Conservative treatment methods can be divided into three groups:
- mechanical,
- physical,
- pharmacological.
Mechanical methods include therapeutic exercises, massage, compression therapy, pneumocompression, and body weight control.
Physical – various types of physiotherapeutic effects (amplipulse, electrophoresis, electrical stimulation, ultraviolet irradiation of blood).
Pharmacotherapy is an integral part of conservative treatment and may include the use of several groups of drugs: those that improve the rheological properties of blood, antibiotics (if indicated), immunomodulators, desensitizing agents, diuretics (however, due to their ability to increase fibrosis, they are prescribed infrequently), phlebotonics.
I would like to dwell on the latter in more detail, since they are the basis of lymphatic drainage therapy. In this regard, preparations based on highly purified diosmin are especially effective, since it has a polyvalent effect. This bioflavonoid has a venotonic and lymphatic drainage effect (increases lymph flow by increasing the oncotic pressure of lymph, reduces capillary permeability, has a direct protective effect on the microvasculature, and has an anti-inflammatory effect due to the blockade of inflammatory mediators.
Using the French drug Phlebodia 600, the direct effect of highly purified diosmin on the functional state of the lymphatic system was proven: activation of proliferation of the lymphatic endothelium was noted with the formation of new capillary lymphatic networks, which led to an increase in the total absorption area and a significant increase in the volume of lymph reabsorption.
It is curious that already on the 3rd day of using Phlebodia 600 in microscopic preparations there was an increase in the density of the lymphatic bed per unit volume, reaching an increase of 63% by the end of the second week of taking the drug, and by the 30th day - an increase in this indicator by 88%. Currently, the drug Phlebodia 600 is widely used in the treatment of chronic venous insufficiency of the lower extremities and hemorrhoidal disease, but it has also proven to be an indispensable remedy in the case of chronic lymphedema.
Its dosage regimen is simple and convenient - 1 tablet once a day. From a pharmaco-economic point of view, Phlebodia 600 compares favorably with its price-quality ratio. 1 package of this drug is enough for a month of regular use and provides a pronounced therapeutic effect.
For those patients in whom conservative therapy has failed (most often due to hypertrophy and fibrosis of fatty tissue), surgical methods are indicated. In this case, conservative therapy should be continued and is the key to successful results of surgical interventions.
Diagnostic methods
In order to exclude other causes of edema and plan surgical intervention, the following types of diagnostics are used:
- Ultrasound of veins to determine fluid accumulations in the subcutaneous tissue and thickening of the superficial fascia;
- lymphography. To carry it out, a contrast agent is injected into a peripheral vessel for the purpose of x-ray tracking of its movement;
- lymphoscintigraphy, which is an isotope study that reveals the condition of the lymph nodes and the degree of obstruction of lymph outflow.
In some cases, to diagnose lymphostasis, consultation with other specialists is necessary.
Clinical manifestations
Clinical signs of lymphedema arise due to the accumulation of edematous fluid in the subcutaneous fat. Chronic accumulation of interstitial fluid leads to inflammation. In addition, slow lymphatic circulation stimulates lipogenesis and fat deposition, which leads to fibrocyte activation and excess connective tissue growth.
Patients with lymphedema experience progressive thickening of the subcutaneous tissue due to fibrosis and hypertrophy of adipose tissue. Such pathological changes initially manifest themselves as swelling of the affected area. The swelling is soft at first, with pressure leaving indentations, but over time it hardens.
Clinical classification of lymphedematous edema:
- Stage 0. Latent or asymptomatic condition , in which swelling is not yet obvious, but lymphatic transport is already impaired. This condition can last for months and even years.
- Stage I: Early accumulation of protein-rich fluid that improves with elevation of the limb.
- Stage II. The appearance of fibrous changes in the skin and subcutaneous fat, the development of sclerosis. Limb elevation alone rarely reduces swelling.
- Stage III. Lymphostatic elephantiasis . Trophic changes in the skin appear, such as acanthosis, fat deposition and warty nevi.
And although the swelling itself usually does not cause serious discomfort, patients are prone to the periodic formation of cellulite due to the increased proliferative activity of microbes in the stagnant fluid. Lymphangitis is also common , which provokes further destruction of the lymphatic vessels. Other skin changes include hyperkeratosis, papillomatosis, and skin breakdown . The most dangerous of the common complications of lymphedema is erysipelas , which is difficult to treat due to severe trophic disorders.
A rare complication of chronic lymphedema is the development of cutaneous malignancies such as lymphangmosarcoma, Kaposi's sarcoma, or lymphoma.
Treatment methods
Lymphedema has no cure, but it can be controlled with proper care.
Conservative treatment
Conservative therapy is used in the early stages of diseases, until structural changes in the skin tissue appear.
Manual and hardware lymphatic drainage massage
With this type of massage, swelling is eliminated and the limb is prepared for wearing compression products. Regular drainage helps prevent the progression of lymphedema. A pneumatic compression sleeve or stocking connected to a pump creates consistent compression of the limb and creates an outflow of fluid. They are used both in the clinic and at home to prevent scarring of the skin.
Compression therapy
The compression bandaging method used is called bandaging. It is used together with lymphatic drainage massage to consolidate the results after a massage session. Elastic sleeves and stockings have a special structure and provide a pressure gradient from bottom to top for effective lymph drainage.
Physiotherapy
Special complex exercises performed in the air or in the pool improve the results of conservative therapy. Physical activity prevents decreased joint mobility, improves lymphatic drainage, and helps patients lose weight. The Miracle Doctor clinic has developed an effective set of exercises to increase physical activity and improve the results of treatment of lymphedema of the lower extremities.
Drug therapy
Treatment, which is based on the complex use of various medications, is aimed at regulating the functioning of the lymphatic system. Medicines and dosage regimen are prescribed by a doctor.
The following medications are prescribed:
- drugs to stimulate the immune system;
- venotonics with lymphotropic effect;
- diuretic and desensitizing treatment;
- antibiotics;
- angioprotectors and prostaglandins that improve peripheral circulation;
During treatment, it is important to follow a diet that limits salt intake, as well as the use of physical therapy: running, swimming, etc.
Lymphedema of the upper extremities
Lymphedema of the arm after removal of the mammary gland is quite often observed in women who have undergone a similar operation. Lymphedema after mastectomy develops as a result of disruption of the integrity of the channels through which fluid passes. After surgery, the patient is required to undergo mandatory examination at certain intervals for timely diagnosis of lymphedema. Redness of the skin or pain in the arm may indicate the onset of inflammation, so the doctor should offer adequate treatment as soon as possible.
Symptoms of lymphedema of the upper extremities may include:
- swelling of the fingers, forearm, shoulders, chest;
- feeling of heaviness in the hands;
- change in skin tone;
- stiffness in joints, loss of flexibility;
- tightly fitting clothes or jewelry (rings, watches) in a certain place on the hand (and the item is of a suitable size).
Therapy begins after confirmation of the diagnosis of upper limb lymphedema. Treatment is determined by a specialist based on the patient’s medical history, the degree of the disease and the individual characteristics of the person.
Advantages of treatment at the Miracle Doctor clinic
- The Miracle Doctor clinic employs highly qualified phlebologists with clinical experience of at least 10 years.
- Therapeutic procedures are carried out at reasonable prices; the cost of outpatient treatment of lymphedema includes the price of compression materials, the cost of seeing a doctor and massage therapist, and a course of exercise therapy.
- Doctors and physiotherapists are available 7 days a week.
- The clinic is located in close proximity to the Rimskaya and Ploshchad Ilyich metro stations.
- Make an appointment with doctors on the website or by calling the clinic.
Where is lymphedema treated in Moscow
Treatment of lymphedema is performed efficiently at the Yusupov Hospital. Qualified specialists work here who will select the most optimal method of treating the disease. Treatment of lymphedema at the Yusupov Hospital makes it possible to stop the development of pathology and improve the patient’s condition. The hospital has established oncology treatment and rehabilitation clinics, where they provide effective treatment for diseases of varying complexity and subsequent restoration of lost functions.
In the event of the development of cancer in the Yusupov Hospital, you can undergo diagnosis and treatment by experienced specialists. Further management of the patient is carried out by doctors from the Oncology and Rehabilitation Clinic. In the rehabilitation center, the patient is provided with all the necessary services to normalize his condition. Professional exercise therapy instructors, massage therapists, nutritionists and other specialists work with patients to help cure lymphedema. Patients are given an individual treatment plan depending on the nuances of their condition and the type of lymphedema.
The Yusupov Hospital treats lymphedema of any complexity. Doctors take on the most difficult cases and achieve maximum results.
You can make an appointment with rehabilitologists and other specialists at the rehabilitation clinic, find out information about the work of the rehabilitation center and other questions of interest by calling the Yusupov Hospital.
Scrotal lymphedema
Scrotal lymphedema is considered a rare disease and can be caused by:
- stay in tropical countries and infection with filariasis;
- sexual infections;
- injuries, wounds;
- operations on the pelvic organs, especially when removing lymph nodes due to tumor metastasis;
- congenital anomalies of lymph outflow;
- inguinal lymphogranulomatosis (malignant lesion of the lymph nodes);
- extrapulmonary tuberculosis;
- chronic erysipelas (streptococcal infection).
All these conditions are accompanied by blockage or external compression of the lymph outflow tract. It gradually accumulates in the scrotum.
Stagnation causes an inflammatory reaction and the growth of scar tissue. This causes irreversible changes and deterioration of tissue nutrition.
Symptoms
The main symptoms of scrotal lymphedema:
- increase in size: at first slightly, then the scrotum can reach gigantic sizes and drops almost to the knee, cases of sagging to ground level are described, its weight reaches 20 kg;
- the swelling is soft and then becomes dense;
- the penis is retracted into the depths of the swollen tissues, sexual intercourse is impossible;
- the size of the inguinal nodes is higher than normal.
In infectious diseases, there are seals on the skin, small ulcers, subcutaneous nodules, and discharge from the urethra. If lymphedema appears against the background of filariasis, then at first the clinical manifestations are similar to a cold: cough, fever, lacrimation. Rashes and red spots appear on the skin of the body. Then pain and swelling of the testicles and scrotum are noted.
Complications
In severe and advanced cases, complications are possible:
- skin cracks with lymph leakage;
- thickening and compaction, darkening of the skin;
- ulcers, erosions;
- microbial secondary infection, thrush (weeping lesions, crusts, unpleasant odor) due to the difficulty of personal hygiene;
- chronic inflammation of the genitourinary system;
- suppuration of the lymph nodes with the formation of an abscess (abscess);
- urinary incontinence, difficulty, pain when urinating;
- degeneration into a cancerous tumor.
Lymphedema of the lower extremities
The most common form of lymphedema is considered to affect the lower extremities. Lymphatic edema of the legs develops after severe symptoms of venous insufficiency (difficulty in the outflow of blood through the veins). It can progress simultaneously with varicose veins or occur as a complication of deep vein thrombosis of the leg.
The main manifestation is persistent swelling, which is difficult to treat with medications and folk remedies. The limbs gradually increase in size until irreversible elephantiasis, the leg becomes like a column. The skin becomes rough, thickened, ulcers and cracks appear on it. When walking, there is heaviness, pain, distension, and swelling that prevents flexion in the joints.
Such changes cause both physical discomfort and severe psychological suffering, leading to loss of performance and disability.
Overview of Lymphedema
Lymphedema is swelling of tissue caused by obstruction of the drainage of lymphatic fluid. Most often it occurs in the lower extremities, but the arm and scrotum in men can also be affected. The main symptoms are an increase in volume and dense swelling (no pit after pressure).
It can be primary (congenital) or secondary (after underlying diseases). It always has a chronic course and requires constant treatment. This pathology accounts for about 5% of all vascular diseases, that is, it refers to common vascular lesions.
Almost 10 million people, mostly women, suffer from lymphedema, among whom the vast majority associate the onset of lymph stagnation with an infectious process.
We recommend reading the article about lymphostasis of the extremities. From it you will learn about the causes of pathology, stages of progression, diagnostics and treatment methods, possible complications and preventive measures. And here is more information about the human lymphatic system.
MBK 10
According to the international classification of diseases, lymphedema (synonyms: lymphatic edema, lymphostasis) is included in the following categories:
- 0 lymphedema, dilatation of lymphatic vessels (lymphangiectasia);
- 2 lymphostasis after removal of the mammary gland, elephantiasis;
- 0 hereditary lymphedema.
Causes
Violation of lymph outflow is caused by:
- heart failure with blood stagnation (low contractility of the heart);
- kidney disease with protein loss - due to the low level of protein molecules in the blood, osmotic pressure decreases, so proteins accumulate in the tissues, causing persistent swelling;
- decreased outflow of venous blood (venous insufficiency) with varicose veins, after suffering venous thrombosis (thrombophlebitis), fistula between an artery and a vein (discharge of blood from the arterial into the venous bed);
- disruption of the patency of lymphatic vascular branches due to injury, burn, compression by an inflammatory focus or tumor (blockage of one path leads to expansion of the bypass and stagnation of lymph);
- infectious diseases of the skin (for example, erysipelas) and subcutaneous tissue, suppuration (phlegmon);
- tuberculosis of the lymph nodes;
- operations that involve removal of lymph nodes (most often oncological);
- a parasitic infection (filariasis, transmitted by mosquitoes), which affects the lymphatic tissue;
- the use of diuretics, dehydration - a lack of tissue fluid causes an expansion of the lymphatic pathways and a decrease in their tone (lymphovenous insufficiency);
- radiation therapy in the area where the lymph nodes are located.
Congenital anomalies in the structure of lymphatic vessels (underdevelopment, narrowing of the lumen, valve insufficiency, excess lymph production) arise due to:
- genetic abnormalities that are inherited;
- effects on a pregnant woman of viral infection, smoking, alcohol, medications, radiation, chemicals;
- increased levels of female sex hormones (gynecological diseases or estrogen treatment, hormonal stimulation of the ovaries).
Stages of the disease
The disease has a continuously progressive course and goes through several stages:
| Stages of Lymphedema | Description | Photo |
| Zero (pre-disease) | There is no edema, but upon examination one can find disturbances in the movement of lymph | |
| First | Swelling in the evening, intensifies after prolonged standing or heavy physical activity, its consistency to the touch is similar to plastic dough, the skin is normal, there is no swelling after sleep; | |
| Second | The swelling lasts around the clock, does not subside by morning, the skin is taut, fused with neighboring tissues (does not move, does not get folded, as it grows with scar tissue), dense, if you press, a hole does not appear, pain occurs; | |
| Third | Irreversible compaction, elephantiasis, no contours of the body in the area of edema (no folds, bends due to edema), increased keratinization, the appearance of tuberosity (the structure is similar to shapeless pillows separated by partitions), sweating increases on the affected part, papillomas (wart-like outgrowths) may grow ); | |
| Fourth | Complications appear in the form of movement disorders, thinning and dryness, lymphatic fluid leaks through skin cracks, trophic ulcers develop, suppuration and spread of infection into the bloodstream (sepsis) are possible. | |
In children, several variants of congenital lymphedema are found with a varied combination of symptoms:
- swelling of the fingers, hands or feet - from insignificant to the resemblance of the limbs to an elephant’s leg (without folds or characteristic outlines);
- gradual spread of swelling along the arm or leg from bottom to top;
- pain is absent (with slow progression) or appears with movement;
- skin folds appear from edematous tissue;
- the folding of the feet and hands is lost, it is impossible to pull or move the skin;
- Externally, the skin looks like an orange peel.
If the disease is associated with genetic disorders, then it can appear immediately after birth or during school or adolescence. With minor anomalies in the development of the lymphatic system, swelling is compensated for a long time due to the redistribution of lymph movement. Then congenital diseases give symptoms already in adulthood. They are provoked by pregnancy, weight gain, and lack of protein in the diet.
In severe cases, hereditary lymphedema leads to the appearance of ulcers or erosions (an area without epithelium), they tend to suppurate. If the infection spreads to the lymphatic vessels, this leads to very rapid progression of the disease. The limbs become ugly, sepsis and severe circulatory disorders are possible.
Lymphedema in oncology: signs
If lymphedema is associated with cancer, then characteristic signs include:
- lesion and thickening of one limb;
- dense painless swelling;
- thickening of skin folds;
- there is no pattern of the network of saphenous veins;
- pale skin, its color may change over time with the appearance of nutritional disorders (reddens, darkens and turns blue);
- swelling below the level of the lymph node (for example, with changes in the pelvic area, the thigh swells, and with axillary localization, the shoulder);
- spread downwards - from the thigh to the foot, from the shoulder to the hand;
- slow progression;
- general manifestations of the tumor: severe weakness, sweating, fever, weight loss.
Stagnation of lymph is provoked by prostate tumors, lymphomas (tumors in the lymph nodes), including lymphogranulomatosis, leukemia (blood cancer). Lymphedema is often the result of treatment for a malignant disease, as it occurs after surgery or radiation therapy. It is important to take into account that the first symptoms may appear even several years after removal of lymphatic tissue or irradiation.
The most common causes of lymphostasis are surgery in the axillary region for breast cancer and inguinal-femoral lymphadenectomy (excision of lymph nodes) for neoplasms of the pelvic organs.
Types: primary, secondary chronic
A comparison of the main types of chronic lymphedema (primary and secondary) is given in the table.
| Sign | Primary lymphedema | Secondary lymphedema |
| Age of patients | Newborns, children, young people (80% females under 18 years of age) | Adults, elderly |
| Development mechanism | Anomalies in the structure of the lymphatic network | Infection, tumor, trauma, surgery, burn disease, kidney damage, heart disease |
| Preferential localization | Lower extremities (91-95%), less often upper, genitals | |
| Symmetry | Double-sided | One-sided |
| Provoking factor | Trauma, pregnancy | Venous insufficiency, varicose veins, thrombosis |
| Detection rate | One case per 10 thousand population | Ten cases per thousand population |
Complications
Stagnation of lymphatic fluid leads to disruption of tissue nutrition, which manifests itself in trophic changes:
- dryness and thinning;
- excessive keratinization, peeling;
- skin cracks with fluid leakage;
- ulcers, fistulas;
- infection and its spread through soft tissues (phlegmon) or into the blood (sepsis);
- malignant degeneration – lymphangiosarcoma.
Lymphangiosarcoma