What will happen in the video:
- 00:22 - what are monocytes
- 02:49 — number of lymphocytes in the blood
- 03:42 — reasons for the increase in monocytes in the blood
- 06:58 - symptoms of increased monocytes in the blood
- 10:39 - increased monocytes in children (monocytosis in children)
Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
What are monocytes and how are they formed?
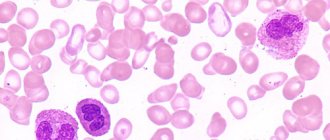
Monocytes are a type of agranulocytic leukocyte (white blood cell). This is the largest element of the peripheral blood flow - its diameter is 18-20 microns. The oval-shaped cell contains one eccentrically located polymorphic bean-shaped nucleus. Intense staining of the nucleus makes it possible to distinguish a monocyte from a lymphocyte, which is extremely important in the laboratory assessment of blood parameters.
In a healthy body, monocytes make up 3 to 11% of all white blood cells. These elements are also found in large quantities in other tissues:
- liver;
- spleen;
- Bone marrow;
- The lymph nodes.
Monocytes are synthesized in the bone marrow, where their growth and development are influenced by the following substances:
- Glucocorticosteroids inhibit the production of monocytes.
- Cell growth factors (GM-CSF and M-CSF) activate the development of monocytes.
From the bone marrow, monocytes penetrate into the bloodstream, where they remain for 2-3 days. After a specified period, the cells either die through traditional apoptosis (cell death programmed by nature), or move to a new level - they turn into macrophages. The improved cells leave the bloodstream and enter the tissues, where they remain for 1-2 months.
Dietary recommendations
During therapy, you should exclude certain foods from your diet and follow a certain diet.
- Consume less sugar - foods containing sugar increase glucose levels and can cause diabetes, which in turn releases a large number of mononuclear leukocytes of the agranulocyte group. First of all, do not consume sugary carbonated drinks, various sweets such as candies, refined sugar, and sweet tea.
- Do not drink alcoholic beverages - drinking and especially alcohol abuse will negatively affect your health and aggravate inflammatory processes in your body.
- Add fish to your diet - as already mentioned, products containing omega-3 fatty acids obtained from fish have a beneficial effect on humans, reducing inflammation and the total number of these leukocytes in the blood. If you are not a fan of fish, especially cod, salmon or mackerel, you can buy omega-3 supplements at the pharmacy.
Monocytes and macrophages: what is the difference?
In the 70s of the last century, it was believed that all monocytes sooner or later turn into macrophages, and there are no other sources of “professional janitors” in the tissues of the human body. In 2008 and later, new studies were conducted that showed that macrophages are heterogeneous. Some of them actually originate from monocytes, while others arise from other progenitor cells even at the stage of intrauterine development.
The transformation of some cells into others follows a programmed pattern. Coming out of the bloodstream into the tissue, monocytes begin to grow, and the content of internal structures - mitochondria and lysosomes - increases. Such rearrangements allow monocyte macrophages to perform their functions as efficiently as possible.
When is it necessary to see a doctor and take an OAC test?
There are no specific signs indicating that monocytes are elevated. But at the same time, monocytosis is accompanied by other diseases, the symptoms of which can indirectly suggest changes in the number of leukocytes.
You should consult a doctor and get tested if:
- Decreased or complete loss of appetite.
- Increased fatigue and causeless weakness.
- Aversion to meat dishes.
- Sudden weight loss.
- Insomnia and drowsiness.
- Irritation, apathy, nervous breakdowns.
- Increased psycho-emotional excitability.
- Loud motility of the gastrointestinal tract.
- Constant feeling of anxiety.
- Unexplained pain in the abdomen.
- Panic attacks.
- The appearance of foamy stools.
- Stool disorders.
- The appearance of pain in joints and muscles.
- Bloody impurities in the stool.
- The appearance of acne on the mucous membranes.
- Skin rashes.
- The presence of a long dry cough with bloody sputum.
- Rashes and redness on the genitals, as well as in case of heavy discharge from the genital tract.
- Discomfort and pain during sexual intercourse.
Biological role of monocytes
Monocytes are the largest phagocytes in our body. They perform the following functions in the body:
- Phagocytosis. Monocytes and macrophages have the ability to recognize and capture (absorb, phagocytose) foreign elements, including dangerous proteins, viruses, and bacteria.
- Participation in the formation of specific immunity and protection of the body from dangerous bacteria, viruses, fungi through the production of cytotoxins, interferon and other substances.
- Participation in the development of allergic reactions. Monocytes synthesize some elements of the complement system, due to which antigens (foreign proteins) are recognized.
- Antitumor protection (provided by the synthesis of tumor necrosis factor and other mechanisms).
- Participation in the regulation of hematopoiesis and blood clotting due to the production of certain substances.
Monocytes, along with neutrophils, belong to professional phagocytes, but have distinctive features:
- Only monocytes and their special form (macrophages) do not die immediately after absorbing a foreign agent, but continue to perform their immediate task. Losing a fight against dangerous substances is extremely rare.
- Monocytes live much longer than neutrophils.
- Monocytes are more effective against viruses, while neutrophils deal mainly with bacteria.
- Due to the fact that monocytes are not destroyed after a collision with foreign substances, pus does not form in places where they accumulate.
- Monocytes and macrophages are capable of accumulating in areas of chronic inflammation.
Determination of the level of monocytes in the blood
The total number of monocytes is displayed as part of the leukocyte formula and is included in the complete blood count (CBC). The material for research is taken from a finger or from a vein. Blood cell counting is carried out manually by a laboratory assistant or using special devices. The results are issued on a form, which must indicate the standards adopted for a particular laboratory. Different approaches to determining the number of monocytes can lead to discrepancies, so it is imperative to take into account where and how the analysis was taken, as well as how the blood cells were counted.
Additional Research
The problem is mainly solved by hematologists, immunologists, and oncologists. But monocytosis is the area of interest of rheumatologists, dermatologists, infectious disease specialists and doctors of a number of other specialized subspecialties.
Additional diagnostic methods include: medical history, physical examination, CBC, OAM, biochemical blood testing, coagulogram, immunogram, survey image of the chest organs, CT, MSCT, MRI, PCR, ELISA, biopsy from the lesion with histological examination. If necessary, the list of studies is expanded: culture of discharge from the lesion on media to determine the sensitivity of the pathogen to antibiotics, microscopy of sputum, sonography, and more.
Normal value of monocytes in children and adults
During hardware decoding, monocytes are designated MON; during manual decoding, their name does not change. The norm of monocytes depending on the age of a person is presented in the table:
| Age | Norm of monocytes, % |
| 1-15 days | 5-15 |
| 15 days – 1 year | 4-10 |
| 1-2 years | 3-10 |
| 2-15 years | 3-9 |
| Over 15 years old | 3-11 |
The normal value of monocytes does not differ between women and men. The level of these blood cells does not depend on gender. In women, the number of monocytes increases slightly during pregnancy, but remains within the physiological norm.
In clinical practice, not only the percentage, but also the absolute content of monocytes per liter of blood matters. The norm for adults and children is as follows:
- Up to 12 years – 0.05-1.1*109/l.
- After 12 years – 0.04-0.08*109/l.
Why might they decline?
A decrease in the number of monocytes in the blood (monocytopenia) can be caused by:
- congenital and acquired immunodeficiency;
- long-term treatment with cytostatics and corticosteroids;
- bone marrow tumors.
Also, the development of this condition can be facilitated by a lack of cyanocobalamin and folic acid, aplastic or hypoplastic anemia. In the initial stages of these diseases, the concentration of monocytes may increase slightly, but as bone marrow dysfunction occurs, a decrease in their absolute number is observed.
Reasons for the increase in monocytes in the blood
An increase in monocytes above the threshold value for each age group is called monocytosis. There are two forms of this condition:
- Absolute monocytosis is a phenomenon when there is an isolated growth of monocytes in the blood, and their concentration exceeds 0.8*109/l for adults and 1.1*109/l for children under 12 years of age. A similar condition is recorded in some diseases that provoke the specific production of professional phagocytes.
- Relative monocytosis is a phenomenon in which the absolute number of monocytes remains within normal limits, but their percentage in the bloodstream increases. This condition occurs when the level of other white blood cells decreases simultaneously.
In practice, absolute monocytosis is a more alarming sign, since it usually indicates serious problems in the body of an adult or child. The relative increase in monocytes is often transient.
What does an excess of monocytes indicate? First of all, it means that phagocytosis reactions have started in the body, and there is an active fight against foreign invaders. The following conditions can cause monocytosis:
Physiological causes of monocytosis
In all healthy people, monocytes increase slightly in the first two hours after eating. It is for this reason that doctors recommend donating blood exclusively in the morning and on an empty stomach. Until recently, this was not a strict rule, and a general blood test with determination of the leukocyte formula was allowed to be done at any time of the day. Indeed, the increase in monocytes after a meal is not so significant and usually does not exceed the upper threshold, but the risk of incorrect interpretation of the result still remains. With the introduction into practice of devices for automatic decoding of blood, sensitive to the slightest changes in cellular composition, the rules for taking the test were revised. Today, doctors of all specialties insist that the OAC be taken on an empty stomach in the morning.
High monocytes in women occur in some special situations:
Menstruation
In the first days of the cycle, healthy women experience a slight increase in the concentration of monocytes in the blood and macrophages in the tissues. This is explained quite simply - it is during this period that active rejection of the endometrium occurs, and “professional janitors” rush to the hearth to perform their immediate duties. The growth of monocytes is observed at the peak of menstruation, that is, on the days of the most heavy discharge. After the monthly bleeding is completed, the level of phagocyte cells returns to normal.
Important! Although the number of monocytes during menstruation usually does not go beyond the normal range, doctors do not recommend taking a complete blood count until the end of your monthly discharge.
Pregnancy
The restructuring of the immune system during pregnancy leads to low levels of monocytes in the first trimester, but then the picture changes. The maximum concentration of blood cells is recorded in the third trimester and before birth. The number of monocytes usually does not exceed the age norm.
Pathological causes of monocytosis
Conditions in which monocytes are so elevated that they are determined in a general blood test to be outside the normal range are considered pathological and require mandatory consultation with a doctor.
Acute infectious diseases
The growth of professional phagocytes is observed in various infectious diseases. In a general blood test, the relative number of monocytes in ARVI slightly exceeds the threshold values accepted for each age. But if during a bacterial infection there is an increase in neutrophils, then in the event of a viral attack, monocytes enter the battle. A high concentration of these blood elements is recorded from the first days of illness and persists until complete recovery.
- After all symptoms subside, monocytes remain high for another 2-4 weeks.
- If an elevated monocyte count is recorded for 6-8 weeks or more, a source of chronic infection should be sought.
With a common respiratory infection (cold), the level of monocytes increases slightly and is usually at the upper limit of normal or slightly beyond its limits (0.09-1.5 * 109/l). A sharp increase in monocytes (up to 30-50*109/l or more) is observed in oncohematological diseases.
An increase in monocytes in a child is most often associated with the following infectious processes:
Infectious mononucleosis
The disease caused by the herpes-like Epstein-Barr virus occurs primarily in preschool children. The prevalence of the infection is such that almost everyone gets it by adolescence. It almost never occurs in adults due to the peculiarities of the immune system's response.
Symptoms:
- Acute onset with fever up to 38-40 °C, chills.
- Signs of upper respiratory tract damage: runny nose, nasal congestion, sore throat.
- Almost painless enlargement of the occipital and submandibular lymph nodes.
- Skin rash.
- Enlarged liver and spleen.
Fever during infectious mononucleosis persists for a long time, up to a month (with periods of improvement), which distinguishes this pathology from other acute respiratory viral infections. In the general blood test, both monocytes and lymphocytes are elevated. The diagnosis is made based on the typical clinical picture, but a test for specific antibodies may be performed. Therapy is aimed at relieving the symptoms of the disease. Targeted antiviral treatment is not carried out.
Other childhood infections
The simultaneous growth of monocytes and lymphocytes is observed in many infectious diseases that occur mainly in childhood and are almost not detected in adults:
- measles;
- rubella;
- whooping cough;
- mumps, etc.
In these diseases, monocytosis is observed in the case of protracted pathology.
In adults, other causes of an increase in the number of monocytes in the blood are identified:
Tuberculosis
A severe infectious disease that affects the lungs, bones, genitourinary organs, and skin. You can suspect the presence of this pathology based on certain signs:
- Long-lasting causeless fever.
- Unmotivated weight loss.
- Prolonged cough (with pulmonary tuberculosis).
- Lethargy, apathy, increased fatigue.
Annual fluorography helps identify pulmonary tuberculosis in adults (in children, the Mantoux test). A chest x-ray helps confirm the diagnosis. To detect tuberculosis of other localizations, specific studies are carried out. In the blood, in addition to an increase in the level of monocytes, there is a decrease in leukocytes, erythrocytes and hemoglobin.
Other infections can lead to monocytosis in adults:
- brucellosis;
- syphilis;
- sarcoidosis;
- cytomegalovirus infection;
- typhoid fever, etc.
The growth of monocytes is observed during a prolonged course of the disease.
Parasitic infestation
Activation of monocytes in the peripheral blood is observed during helminth infection. These can be either opisthorchid, bovine or pork tapeworm, pinworms and roundworms, which are common in temperate climates, or exotic parasites. When the intestines are damaged, the following symptoms occur:
- Abdominal pain of various localizations.
- Loss of stool (usually diarrhea).
- Unmotivated weight loss due to increased appetite.
- Allergic skin reaction such as urticaria.
Along with monocytes, an increase in eosinophils, granulocytic leukocytes responsible for the allergic reaction, is recorded in the blood of a person infected with helminths. To identify parasites, feces are taken for analysis, bacteriological cultures are done, and immunological tests are performed. Treatment includes taking antiparasitic medications depending on the source of the problem found.
Chronic infectious and inflammatory processes
Almost any indolent infection that exists in the human body for a long time leads to an increase in the level of monocytes in the blood and the accumulation of macrophages in tissues. It is difficult to identify specific symptoms in this situation, since they will depend on the form of the pathology and the location of the lesion.
This could be an infection of the lungs or throat, heart muscle or bone tissue, kidneys and gallbladder, or pelvic organs. This pathology is manifested by constant or periodically occurring pain in the projection of the affected organ, increased fatigue, and lethargy. Fever is not typical. After identifying the cause, optimal therapy is selected, and as the pathological process subsides, the level of monocytes returns to normal.
Autoimmune diseases
This term refers to conditions in which the human immune system perceives its own tissues as foreign and begins to destroy them. At this moment, monocytes and macrophages come into play - professional phagocytes, well-trained soldiers and janitors, whose task is to get rid of the suspicious focus. But with autoimmune pathology, this focus becomes one’s own joints, kidneys, heart valves, skin and other organs, from which all the symptoms of the pathology appear.
The most common autoimmune processes:
- Diffuse toxic goiter is a lesion of the thyroid gland, in which increased production of thyroid hormones occurs.
- Rheumatoid arthritis is a pathology accompanied by the destruction of small joints.
- Systemic lupus erythematosus is a condition that affects skin cells, small joints, heart valves, and kidneys.
- Systemic scleroderma is a disease that affects the skin and spreads to internal organs.
- Type I diabetes mellitus is a condition in which glucose metabolism is impaired, and other parts of metabolism are also affected.
The growth of monocytes in the blood in this pathology is only one of the symptoms of systemic damage, but does not act as a leading clinical sign. To determine the cause of monocytosis, additional tests are required taking into account the suspected diagnosis.
Oncohematological pathology
A sudden increase in monocytes in the blood is always scary, as it may indicate the development of malignant blood tumors. These are serious conditions that require a serious approach to treatment and do not always end well. If monocytosis cannot be associated with infectious diseases or autoimmune pathology, you should see an oncohematologist.
Blood diseases leading to monocytosis:
- Acute monocytic and myelomonocytic leukemia. A variant of leukemia in which monocyte precursors are detected in the bone marrow and blood. It is found mainly in children under 2 years of age. Accompanied by signs of anemia, bleeding, and frequent infectious diseases. There is pain in the bones and joints. It has a poor prognosis.
- Multiple myeloma. It is detected mainly after the age of 60 years. It is characterized by the appearance of bone pain, pathological fractures and bleeding, and a sharp decrease in immunity.
The number of monocytes in oncohematological diseases will be significantly higher than normal (up to 30-50*109/l and higher), and this makes it possible to distinguish monocytosis in malignant tumors from a similar symptom in acute and chronic infections. In the latter case, the concentration of monocytes rises slightly, while in leukemia and myeloma there is a sharp increase in agranulocytes.
Other malignancies
If monocytes grow in the blood, attention should be paid to lymphogranulomatosis (Hodgkin's disease). The pathology is accompanied by fever, enlargement of several groups of lymph nodes and the appearance of focal symptoms in various organs. Possible damage to the spinal cord. To confirm the diagnosis, puncture of the altered lymph nodes is performed with histological examination of the material.
An increase in monocytes is also observed in other malignant tumors of various locations. To identify the cause of such changes, targeted diagnostics are required.
Chemical poisoning
A rare cause of monocytosis that occurs in the following situations:
- Tetrachloroethane poisoning occurs when the substance is inhaled or ingested through the mouth or skin. Accompanied by irritation of the mucous membranes, headache, jaundice. In the long term, it can lead to liver damage and coma.
- Phosphorus poisoning occurs through contact with contaminated vapor or dust or accidental ingestion. In acute poisoning, stool loss and abdominal pain are observed. Without treatment, death occurs as a result of damage to the kidneys, liver and nervous system.
Monocytosis in case of poisoning is only one of the symptoms of the pathology and occurs in combination with other clinical and laboratory signs.
Correction
Conservative therapy
It is impossible to directly bring the monocyte level to normal values. To do this, it is necessary to fight the cause, i.e. treat the underlying pathology against which monocytosis developed. If monocytosis is detected in the blood of a person who has recently suffered an acute infectious disease, then treatment is not required. This is an absolutely normal phenomenon; the concentration of monocytes returns to normal on its own after a few days. In case of prolonged and, especially, high monocytosis, medical intervention is necessary:
- Anti-infective treatment
. To treat most viral infections, only bed rest, plenty of hot drinks, the use of non-steroidal anti-inflammatory drugs (paracetamol, ibuprofen), as well as symptomatic therapy (gargling or irrigating the throat with antiseptic, anesthetic solutions, sprays, instilling vasoconstrictor drops into the nose) are sufficient. For bacterial infections, antibiotics are prescribed, for tuberculosis, a combination of anti-tuberculosis drugs. - Anti-inflammatory treatment
. As a pathogenetic treatment of chronic granulomatous diseases and collagenoses, drugs that suppress inflammation are used - glucocorticosteroids (prednisolone, methylprednisolone). For a more powerful anti-inflammatory effect, immunosuppressants are effective - methotrexate, cyclophosphamide. - Chemotherapy.
To treat malignant blood diseases, histiocytosis, courses of chemotherapy treatment are necessary. Sometimes it is necessary to resort to intrathecal administration of drugs (injection into the cerebrospinal fluid).
Surgery
There is a surgical method for the treatment of oncohematological diseases and some types of congenital neutropenia, which allows for complete recovery from the disease - this is a transplantation of donor hematopoietic stem cells. To carry out this operation, it is necessary to perform HLA typing (a genetic test that determines histocompatibility antigens) in order to select a suitable donor. However, this method of treatment is used as a last resort when conservative therapy is unsuccessful, as it is associated with a high risk of death.
Reasons for the decrease in monocytes in the blood
Monocytopenia is a decrease in monocytes in the blood below a threshold value. A similar symptom occurs in the following conditions:
- Purulent bacterial infections.
- Aplastic anemia.
- Oncohematological diseases (late stages).
- Taking certain medications.
Reduced monocytes are somewhat less common than an increase in their number in the peripheral blood, and often this symptom is associated with serious diseases and conditions.
Purulent bacterial infections
This term refers to diseases in which pyogenic bacteria invade and inflammation develops. We are usually talking about streptococcal and staphylococcal infections. Among the most common purulent diseases it is worth highlighting:
- Skin infections: boil, carbuncle, cellulitis.
- Bone damage: osteomyelitis.
- Bacterial pneumonia.
- Sepsis is the entry of pathogenic bacteria into the blood with a simultaneous decrease in the overall reactivity of the body.
Some purulent infections tend to self-destruct, others require mandatory medical intervention. In the blood test, in addition to monocytopenia, there is an increase in the concentration of neutrophilic leukocytes - cells responsible for a rapid attack at the site of purulent inflammation.
Aplastic anemia
Low monocytes in adults can occur in various forms of anemia, a condition in which there is a lack of red blood cells and hemoglobin. But if iron deficiency and other variants of this pathology respond well to therapy, then aplastic anemia deserves special attention. With this pathology, there is a sharp inhibition or complete cessation of the growth and maturation of all blood cells in the bone marrow, and monocytes are no exception.
Symptoms of aplastic anemia:
- Anemic syndrome: dizziness, loss of strength, weakness, tachycardia, pale skin.
- Bleeding of various localizations.
- Decreased immunity and infectious complications.
Aplastic anemia is a severe hematopoietic disorder. Without treatment, patients die within a few months. Therapy involves eliminating the cause of anemia, taking hormones and cytostatics. A bone marrow transplant has a good effect.
Oncohematological diseases
In the later stages of leukemia, inhibition of all hematopoietic germs and the development of pancytopenia are noted. Not only monocytes suffer, but also other blood cells. There is a significant decrease in immunity and the development of severe infectious diseases. Unreasonable bleeding occurs. Bone marrow transplantation is the optimal treatment option in this situation, and the sooner the operation is performed, the greater the chance of a favorable outcome.
Taking medications
Some medications (corticosteroids, cytostatics) inhibit bone marrow function and lead to a decrease in the concentration of all blood cells (pancytopenia). With timely assistance and discontinuation of the drug, bone marrow function is restored.
Monocytes are not just professional phagocytes, janitors of our body, ruthless killers of viruses and other dangerous elements. These white blood cells are a marker of health along with other indicators of a complete blood count. If your monocyte level increases or decreases, you should definitely see a doctor and undergo an examination to find the cause of this condition. Making a diagnosis and selecting a treatment regimen is carried out taking into account not only laboratory data, but also the clinical picture of the identified disease.
Author:
Selezneva Valentina Anatolyevna physician-therapist
Classification
There are no clear digital divisions of monocytosis. Conventionally, moderate and severe monocytosis are distinguished. According to the pathogenetic mechanism:
- Reactive monocytosis
. The cause of this type is inflammatory and infectious pathologies. - Neoplastic (malignant) monocytosis
. Occurs in patients with myeloproliferative and lymphoproliferative diseases (in children with lymphogranulomatosis and acute monoblastic leukemia).
In children, from the moment of birth, a slight increase in monocytes is observed, it reaches a maximum at the end of 1 week of life (up to 15%), then slowly decreases and by the 12th month it becomes like in adults.