Parathyroid hormone is a biologically active element that is a hormonal substance. In medicine it is deciphered in different ways, for example:
- PGT;
- parathyrin;
- parathyroid hormone;
- Pth.
This substance is synthesized by the parathyroid glands, of which, according to the norm, there should be exactly 4 in the body, although their number is not entirely stable. They have a symmetrical arrangement relative to each other, one pair from below, the second pair from above on the posterior surface of the thyroid gland.
The hormone is a single-chain polypeptide substance. It is formed from 84 amino acid residues. In a brain appendage such as the pituitary gland, somatotropic hormonal substances similar in chemical structure are formed. Placental lactogen and prolactin also join the ranks of these hormones. Excess fat in the body of an adult, a sudden delay in development in children, all these are consequences of a serious lack of somatotropic hormone. A normal concentration of this biologically active substance in the body ensures the constancy of a person’s emotional state, and also maintains the functioning of the organs of the human body and improves our internal sense of self.
Parathyroid hormone - what is it?
Parathyroid hormone is a hormone of the parathyroid glands
(it would be more correct to say “parathyroid glands”, but many patients are already very accustomed to the term “parathyroid glands”, although it is not entirely correct from the point of view of word formation).
Parathyroid hormone production
produced by parathyroid cells in response to a decrease in the level of ionized calcium in the blood. On the surface of the cells of the parathyroid glands there are special receptors that are able to assess the concentration of ionized calcium in the blood and, in accordance with its level, produce parathyroid hormone in larger or smaller quantities.
Very often the term “ parathyroid hormone”
"(parathyroid hormone - from parathyroid hormone) is written incorrectly, since it can be difficult for a non-specialist to hear all the features of the correct spelling.
Often on the Internet you can come across terms such as “ parad hormone
”, “
parade hormone
” and even “
parade of hormones
”. The correct term, of course, is one - parathyroid hormone (written together and without a hyphen).
Parathyroid hormone is a polypeptide hormone
(i.e. consisting of amino acids). There are 84 amino acid residues in the parathyroid hormone molecule. Currently, the structure of parathyroid hormone has been completely deciphered by scientists. It was found that in the parathyroid hormone molecule, the first 34 amino acid residues are responsible for the biological activity, and the rest are responsible for the binding of the hormone to receptors and the stability of the molecule as a whole.
The main effect of parathyroid hormone is to increase the level of ionized calcium
in blood. This action is realized through three different effects.
Firstly, parathyroid hormone enhances the activation of vitamin D in the kidneys
, which leads to the formation of an important hormone-like substance, calcitriol, from vitamin D. Calcitriol stimulates the absorption of calcium in the intestine, which leads to an increased flow of calcium from food into the blood. A prerequisite for the implementation of this effect of parathyroid hormone is the presence of a sufficient amount of vitamin D in the body. Without sufficient supply of vitamin D in the blood, parathyroid hormone is not able to enhance the absorption of calcium in the intestine.
Secondly, parathyroid hormone enhances the reabsorption of calcium ions from primary urine
. This effect is realized at the level of the renal tubules.
Thirdly, parathyroid hormone enhances the activity of osteoclasts
– cells that destroy bone tissue. Osteoclasts, like bulldozers or excavators, begin to actively destroy bone beams and release the resulting calcium into the blood. As a result, the concentration of calcium in the blood increases, but the strength of bone tissue decreases, which increases the likelihood of fractures.
Parathyroid hormone is a very interesting hormone, since the effect of parathyroid hormone on the bone directly depends on the mode of its production
. Everything that we said above about the negative effect of parathyroid hormone on bone tissue is true only for cases when parathyroid hormone is constantly and continuously elevated. At the same time, periodic and short-term release of parathyroid hormone into the blood has a positive effect on bone tissue, leading to increased formation of bone beams and bone strengthening. Now this effect is used in the treatment of osteoporosis - even a medicinal analogue of parathyroid hormone (teriparatide) has been synthesized, the periodic administration of which into the body can increase the strength of bone tissue and reduce the likelihood of fractures.
Action of PTH
Cells of target organs carry receptors suitable for PTH, and the interaction of parathyroid hormone with them entails a series of reactions that result in the movement of Ca from stores located in the cell into the extracellular fluid.
In bone tissue, PTH receptors are located on young (osteoblasts) and mature (osteocytes) cells. However, the main role in the dissolution of bone minerals is played by osteoclasts - giant multinucleated cells belonging to the macrophage system? It's simple: their metabolic activity is stimulated by substances produced by osteoblasts. Parathyroid hormone causes osteoclasts to work intensively, which leads to an increase in the production of alkaline phosphatase and collagenase, which, through their influence, cause the destruction of the basic substance of bones and thus help the movement of Ca and P into the extracellular space from bone tissue.
The mobilization of Ca from the bones into the blood, stimulated by PTH, enhances the reabsorption (reverse absorption) of this macroelement in the renal tubules, thereby reducing its excretion in the urine and absorption in the intestinal tract. In the kidneys, parathyroid hormone stimulates the formation of calcitriol, which, together with parathyroid hormone and calcitonin, is also involved in the regulation of calcium metabolism.
Parathyroid hormone reduces the reabsorption of phosphorus in the renal tubules, which promotes its increased removal through the kidneys and a decrease in the phosphate content in the extracellular fluid, and this, in turn, increases the concentration of Ca2+ in the blood plasma.
Thus, parathyroid hormone is a regulator of the relationship between phosphorus and calcium (restores the concentration of ionized calcium to the level of physiological values), thereby ensuring a normal state:
- Neuromuscular conduction;
- Calcium pump functions;
- Enzymatic activity;
- Regulation of metabolic processes under the influence of hormones.
Of course, if the Ca/P ratio deviates from normal limits, signs of disease occur.
Parathyroid hormone production
The production of parathyroid hormone is regulated by the level of ionized calcium
in blood. If calcium in the blood decreases, parathyroid hormone begins to be released more actively.
On the surface of the cells of the parathyroid glands there is a calcium-binding receptor, which is directly able to “sense” the concentration of calcium in the blood and regulate the rate at which parathyroid hormone is produced. This is the only receptor currently known to science that is “controlled” not by peptides or hormones, but by the substance itself—or rather, by its ions. Be that as it may, parathyroid hormone is normally produced by the parathyroid glands only when the concentration of calcium in the blood decreases.
What can influence the result?
Before donating blood for analysis, you should definitely consult with your doctor about preparing for the test. You need to know from the beginning what can lead to unreliable results, and take care to eliminate possible obstacles that could affect the data obtained. So, in order to go through the procedure correctly, you need to consider the following.
Drinking milk shortly before blood collection may cause lower values. An increase in the hormone is often observed during pregnancy and lactation. False reduction may occur in Burnett's disease (lactic acid syndrome). The use of radioisotope preparations can distort the results.
Medicines that can increase the concentration of PTH in the blood are diuretics, phosphates, rimphapicin, lithium, steroids, isoniazid, anticonvulsants and thiazide medications. Medicines that can cause the opposite effect, that is, lower the level, are propranolol, cimetidine.
Important! In addition, it should be taken into account that the concentration of the hormone is subject to circadian rhythms and is characterized by fluctuations throughout the day. Maximum values are observed at 14-16 hours, and basal rates are recorded around 8 am.
Parathyroid hormone and calcium
There are two “friends” in the body, two substances that are inextricably linked - parathyroid hormone, calcium
.
At the same time, there is a relationship between them, which in endocrinology is described as “double feedback”. They sort of regulate each other. When the level of calcium in the blood decreases, parathyroid hormone begins to be released more strongly, as a result of which calcium in the blood increases and acts on the cells of the parathyroid glands through the receptor, causing them to stop releasing parathyroid hormone. After the release of parathyroid hormone ceases, calcium begins to gradually decrease until it reaches a level at which the cells of the parathyroid glands are activated with the release of parathyroid hormone - and the cycle repeats. Calcium is the main thing that parathyroid hormone influences, and at the same time parathyroid hormone is one of the most important substances that calcium influences
.
What happens when the hormone levels are disrupted?
Due to a failure of the normal level of parathyroid hormone, the kidneys suffer. The thing is that this hormonal substance regulates the content of phosphorus salts in this organ. Since the mechanism goes astray, the kidneys suffer from excess phosphorus salts. This can also lead to a disease associated with stone formation in a given organ. In this case, the failure affects not only the kidneys, but also the stomach. Ulcers can form in it, the cause of which is calcification. There is a circulatory disorder in the blood vessels. If a person is found to have a fairly low level of parathyroid hormonal substance, which is called hypoparathyroidism, then many disorders are detected in the body. To begin with, this is the poor performance of the muscular system, in which their normal activity is disrupted. Problems with the heart, intestines, and the human psyche are also attributed here.
The amount of the hormone varies by age and gender.
The quantitative content of this hormonal substance depends on gender and directly on the age category. In order to maintain the normal level of parathyroid hormone in the body, you need to familiarize yourself with the following table indicators:
Norms of parathyroid hormonal substances for men:
- up to 19-23 years – from 12 to 94 pg/ml;
- from 24 to 71 years – from 9.5 to 73 pg/ml;
- over 72 years old – 4.7 to 116 pg/ml.
Norms of parathyroid hormonal substance for women:
- up to 19-21 years – from 13 to 94 pg/ml;
- from 22 to 72 years – from 9.5 to 74 pg/ml;
- over 73 years old – 4.7 to 115 pg/ml.
During pregnancy, the level of parathyroid hormone for women ranges from 9.4 to 74 pg/ml.
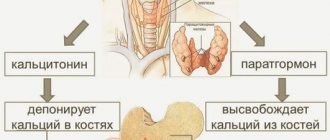
Parathyroid hormone and calcitonin
Unlike substances such as calcium, parathyroid hormone and calcitonin are “enemies”, antagonists
.
Parathyroid hormone aims to increase the level of calcium in the blood, and calcitonin aims to reduce it. Parathyroid hormone stimulates the destruction of bone beams with a prolonged increase, and calcitonin, on the contrary, causes the formation of new bone tissue and thereby strengthens the bone. The relationships between hormones, if you dig deep, are even deeper - for example, in some hereditary syndromes (multiple endocrine neoplasia syndrome, MEN), tumors simultaneously develop that produce both hormones - parathyroid hormone, calcitonin. Therefore, when examining for elevated parathyroid hormone, calcitonin is required
.
Functions of parathyroid hormone in the body
Anatomically, 3 or 4 parathyroid glands (PTG) are located on the posterior surface of the thyroid gland, as if at its corners. Their sizes are very small, the total mass barely reaches 85 mg.
PTGs synthesize a substance that has several names: parathyroid hormone, PTH, parathyrin and an important function: maintaining optimal levels of calcium and phosphorus in the blood. He does this in three ways:
- Enhances the removal of calcium and phosphorus from bones.
- Increases the absorption of the same mineral from food (forces the kidneys to synthesize more vitamin D).
- Reduces the excretion of calcium in the urine, and increases phosphorus.
At first glance, the exchange of calcium and phosphorus is important only for bone tissue. However, this is not true: excess parathyroid hormone affects all aspects of human health.
Vitamin D and parathyroid hormone
Vitamin D and parathyroid hormone are substances whose effects are similar and largely depend on each other. Both substances - vitamin D and parathyroid hormone - their main effect is to increase blood calcium levels
. As is the case with calcium, parathyroid hormone and vitamin D can influence each other. This effect is very interesting and is implemented in general terms like this. When the level of calcium in the blood decreases, the cells of the parathyroid glands begin to actively produce parathyroid hormone, which enhances the hydroxylation of vitamin D in the kidneys and the formation of calcitriol, the active form of vitamin D, which, due to the strength of its action, can be confidently recognized as a hormone. Calcitriol, on the one hand, enhances the release of a special transport protein in the intestinal wall - calmodulin, which “drags” calcium from the intestinal lumen into the blood, and on the other hand, it directly acts on a special receptor on the surface of the cells of the parathyroid glands (it is called the vitamin receptor D or VDR, vitamin D receptor). Activation of the vitamin D receptor leads to suppression of the proliferation of parathyroid gland cells, i.e. indirectly acts to reduce parathyroid hormone levels.
It is important to understand that a decrease in the intake of vitamin D into the human body leads to a “disinhibition” of the division of cells of the parathyroid glands and at the same time to stimulation of the production of parathyroid hormone by these cells. This occurs when there is little sun exposure to the skin, since vitamin D is produced in human skin. The second cause of vitamin D deficiency is insufficient intake of vitamin D from food. Low vitamin D in the blood leads to a low intake of calcium into the blood, which activates the production of parathyroid hormone by the cells of the parathyroid glands.
Vitamin D deficiency has been proven to increase the incidence of benign tumors
– adenomas of the parathyroid glands (probably due to the elimination of the inhibitory effect of vitamin D on the division of cells of the parathyroid glands due to its deficiency).
The second common situation with which patients come to the North-Western Endocrinology Center is the so-called secondary hyperparathyroidism, i.e. a condition in which parathyroid hormone is elevated in the blood, but calcium is normal
. The detection of normal or reduced calcium simultaneously with an increase in parathyroid hormone levels usually indicates a low level of vitamin D in the blood. You can, of course, conduct a blood test for vitamin D, but you can do it differently - prescribe vitamin D and calcium supplements to the patient, and after 1-2 months, repeat the blood test for parathyroid hormone and ionized calcium. If a repeated analysis reveals a decrease or normalization of parathyroid hormone, and the calcium level is normal, this will indicate with a high degree of certainty that the patient simply needs to take calcium and vitamin D supplements longer. If a repeated blood test shows that parathyroid hormone is is still high, and calcium has increased above normal - this will indicate that the patient has primary hyperparathyroidism, a tumor of the parathyroid gland.
Treatment for deviations from the normal level of parathyroid hormone
If there is a lack of PTH, hormone replacement therapy is prescribed for a long period of time or for life.
If there is an excess of PTH, surgical treatment is performed. This means that part of one or more parathyroid glands is removed. In this way it is possible to reduce the secretion of the hormone. If there is cancer of the gland, it is removed entirely. After complete resection of the gland, hormone replacement therapy is prescribed.
To prevent an increase in the level of the hormone, you need to know that its content increases when taking certain medications - such as steroids, some types of diuretics, anticonvulsants, phosphates, lithium, vitamin D, isoniazid, rifampicin. You cannot diagnose and prescribe treatment for yourself.
Blood test for parathyroid hormone
Analysis for parathyroid hormone
is one of the most important in the list of examinations prescribed for suspected calcium metabolism disorders, including the development of osteoporosis.
Blood for parathyroid hormone is usually donated simultaneously with an analysis for ionized calcium, phosphorus, calcitonin
, since such a block of studies allows the endocrinologist to most fully assess the metabolic state. It is also highly advisable to immediately perform densitometry - a study of bone tissue density, which shows the likelihood of developing bone fractures.
Parathyroid hormone - analysis
, the quality of which varies greatly between different laboratories. Currently, the most common methods of performing a blood test for parathyroid hormone are enzyme immunoassay (the so-called 2nd generation method) and immunochemiluminescence (3rd generation method).
Most laboratories analyze parathyroid hormone using a 2nd generation method
, since equipment and reagents for enzyme-linked immunosorbent assay (ELISA) are inexpensive, you can even use domestically produced reagents. At the same time, the use of the ELISA method leads to a decrease in the accuracy of the analysis of parathyroid hormone in the blood and an increase in error.
The specialized laboratory of the North-Western Center for Endocrinology uses a 3rd generation automatic immunochemiluminescent analyzer DiaSorin Liaison XL (Italy) to perform analysis for parathyroid hormone.
– a device with exceptionally high analytical accuracy. In the work of endocrinologists at our center, the accuracy of a test such as a blood test for parathyroid hormone is the main diagnostic component, so we take issues of research quality very seriously. The specialized laboratory of the center NEVER performs parathyroid hormone analysis using the 2nd generation method and NEVER uses either domestic or Chinese reagents - only reagents made in Italy by the DiaSorin company.
If you are deciding where to donate parathyroid hormone
, and are not sure what tests should be taken additionally -
do the following blood test: parathyroid hormone and calcium (ionized is very desirable), phosphorus, calcitonin
. If you also donate your daily urine test for calcium, that will be simply wonderful; any endocrinologist will appreciate your erudition in matters of taking tests.
In the laboratory of the Endocrinology Center, the analysis for ionized calcium is carried out using an automatic biochemical analyzer Olympus AU-680 (Japan) - a high-performance, high-precision automatic machine capable of conducting up to 680 biochemical tests per hour! Combined with the high accuracy of parathyroid hormone and calcitonin tests, an accurate calcium test will provide optimal diagnostic results.
How to get tested
First you need to understand what signs may indicate that it is time to get tested. These include:
- hypocalcemia and hypercalcemia;
- osteoporosis;
- frequent bone injuries and fractures without a sufficiently compelling reason;
- sclerosis of spinal tissue;
- calcium phosphate stones for urolithiasis;
- cystic bone changes;
- suspicion of tumor formations in the parathyroid glands.
If you come to the conclusion that research is necessary, you need to know how to take the test correctly. The rules are as follows:
- Before taking the test, do not eat anything for 10 hours;
- Avoid drinking alcohol at least 24 hours before;
- do not smoke an hour before donating blood;
- for three days, do not play sports and limit other physical activities;
- a day or two before the test, stop taking medications, especially those containing calcium and vitamin D);
- Blood must be donated between 8 and 11 am.
The analysis shown can be performed in almost any laboratory. If the results confirm that secretion is impaired, you should contact an endocrinologist.
Where to get parathyroid hormone
The specialized laboratory of the North-Western Endocrinology Center takes tests for parathyroid hormone and calcium, phosphorus and calcitonin
, as well as receiving other analyzes (more than 1000 studies) at the following addresses in St. Petersburg and Vyborg:
— Petrograd branch of the endocrinology center
– center of St. Petersburg, 200 meters to the left on foot from the Gorkovskaya metro station, Kronverksky Prospekt, building 31. Branch opening hours: 7.30-20.00, seven days a week. Phone: 498-10-30. There is parking for cars.
— Primorsky branch of the endocrinology center
– Primorsky district of St. Petersburg, 250 meters to the right from the Begovaya metro station. Branch address: st. Savushkina, house 124, building 1. Branch opening hours: 7.00-20.00, seven days a week. Phone: 565-11-12. There is parking for cars.
— Vyborg branches of the Endocrinology Center:
- Vyborg, st. Gagarina, 27A, tel., from 7.30 to 20.00, seven days a week. There is parking available for cars.;
- Vyborg, Pobedy Ave., 27A, tel. (81378) 36-306, from 7.30 to 20.00, seven days a week. There is parking for cars.
The branches of the endocrinology center provide everything for the comfort of patients who came to take parathyroid hormone, calcium and other tests
– no queues, comfortable treatment rooms with comfortable chairs and cartoons for a positive attitude, air conditioning and deep air purification systems, modern vacuum blood collection systems.
You can receive the results of a blood test for parathyroid hormone and other indicators by email
immediately after they are completed. In the vast majority of cases, tests are performed within 1 day (often the test for parathyroid hormone and calcium is ready in the evening of the day the patient came for the test).
You can find a complete list of laboratory branches in the Leningrad region (the cities of Luga, Gatchina, Kingisepp, Svetogorsk) here.
If you are not yet sure where to take parathyroid hormone in St. Petersburg or the Leningrad region
– contact the Northwestern Endocrinology Center. You will be confident in the quality of the research and conduct it with comfort. It is important that in the same center you can get a consultation with an endocrinologist who has significant experience in treating disorders of parathyroid hormone production.
Goals of PTH testing
A blood test for parathyroid hormone is used for the following diagnostic measures:
- assessment of pancreas functioning;
- identifying the causes of calcium metabolism disorders (hyper- and hypocalcemia);
- differentiation of hyperparathyroidism (primary, secondary and tertiary);
- definitions of hypoparathyroidism;
- monitoring the condition of patients with chronic pathologies of calcium metabolism.
In addition, the procedure is carried out to evaluate the effectiveness of prescribed therapeutic measures or after surgery on the pancreas to excise tumors.
Parathyroid hormone is normal
When you donate blood in a specialized modern laboratory and receive the result of a test for parathyroid hormone, the norm is indicated on the laboratory form
immediately after your individual result.
Parathyroid hormone levels can be expressed in two different units of measurement - pg/ml and pmol/l. Recalculation between them is possible using the following formula:
parathyroid hormone level in pmol/l x 9.8 = parathyroid hormone level in pg/ml
Parathyroid hormone is normal
, when it fits within the boundaries specified as reference limits (standards).
This indicator is not dependent on gender - if you take a parathyroid hormone test, the norm for women will not differ from the norm for men
.
What symptoms are observed with low parathyroid hormone?
Manifestations of the disease include the following groups of signs:
- convulsive syndrome;
- disorders of the autonomic system;
- mental changes;
- trophic disorders;
- visual disturbances.
Seizures in tetanic (otherwise convulsive) syndrome are characterized by selective and symmetrical (on both sides simultaneously) damage to certain muscle groups. Basically, convulsive activity develops in the muscles of the arms, much less often in the legs; in cases of severe disease, convulsions appear on the face, the muscles of the visceral organs are very rarely affected.
| Localization of seizures | Clinical manifestations |
| Hands | The shoulder is pressed to the body, the forearm is bent at the elbow, and the hand is in the radiocarpal and metacarpal joints, the fingers are clenched and slightly inclined towards the palm - “the hand of the obstetrician.” |
| Legs | The foot is curved inward, the toes are in a state of plantar flexion, with the big toe covering the others, and the sole is depressed in the form of a groove. Both limbs are extended and pressed tightly against each other. |
| Face | The eyelids are half-lowered, the eyebrows are shifted, the jaws are clenched, the mouth is half-open and its corners are lowered - “fish mouth” |
| Coronary vessels | Sharp chest pain, tachycardia, sensations of interruptions in heart function |
| Neck | Laryngospasm (spasm of the glottis), inhalation becomes difficult (inspiratory dyspnea), the skin of the face becomes cyanotic, foam appears on the lips. In severe cases, loss of consciousness is possible, the patient requires intubation or tracheotomy, otherwise death is possible |
| Torso – muscles of the neck and back | Rigidity of the spine, the body arches backward. |
| Torso - intercostal and abdominal muscles, diaphragm | Shortness of breath, bronchospasm |
| Gastrointestinal tract | Difficulty swallowing, nausea, vomiting, constipation, intestinal colic |
| Bladder | Anuria (lack of urination) |
In hypoparathyroidism, convulsive syndrome has a number of the following features:
- Cramps are always painful, voluntary movements of the contracted muscles are impossible. They are hard, difficult to stretch, after which they return to their previous state.
- Attacks rarely occur spontaneously; they are often provoked by external stimuli: trauma, physical exertion, overheating of the body; in women they can occur during pregnancy or childbirth (uterine tetany).
- Children are more likely than adults to suffer from cramps in the muscles of the larynx and internal organs, which can occur without connection with cramps in other muscle groups. During an attack, a child may die from asphyxia (suffocation).
If there is a mild form of the disease, attacks develop a maximum of twice a week, their duration is up to several minutes. In the case of a severe course, convulsive syndrome can develop repeatedly during the day, and its duration can reach several hours.
Autonomic disorders cause the following symptoms:
- profuse sweating;
- dizziness, sometimes ending in fainting;
- increased perception of loud or harsh sounds, bitter or sweet tastes;
- ringing in the ears, hearing loss;
- cardiac pain, heart rhythm disturbances;
- algomenorrhea in women (painful menstruation)
Changes in the psyche occur with long-term hypoparathyroidism. In such patients, intellectual abilities decrease, memory deteriorates, depression, neuroses and frequent insomnia develop.
Another manifestation of the chronic form of the disease is trophic disorders, the symptoms of which are:
- the skin becomes dry and flaky, pigmentation spots appear, and candidiasis occurs;
- the structure of the hair is disrupted, up to alopecia or early graying, and its growth slows down;
- the condition of tooth enamel deteriorates, caries develops or intensifies;
- In children, the risk of improper skeletal formation increases; they lag behind their peers in growth.
Also, patients suffering from hypoparathyroidism for a long time develop visual disturbances:
- blurred vision at dusk;
- disturbances of accommodation;
- the development of cataracts, which provokes deterioration of vision, possibly the development of blindness.
Hypoparathyroidism can greatly complicate a person's life. However, many symptoms, as calcium levels return to normal, gradually undergo regression (reverse development), and restoration of the activity of the affected organs is observed. But in cases of prolonged or severe course of the disease, as well as the absence or ineffectiveness of the treatment used, consequences may remain.
Parathyroid hormone is elevated
Increased parathyroid hormone
is one of the most common reasons for patients to visit an endocrinologist - and rightly so, since high parathyroid hormone in the blood always means the presence of a disease that needs to be treated.
An increase in parathyroid hormone is referred to as “hyperparathyroidism”
. High parahormone is the main symptom of hyperparathyroidism. There are two main variants of this condition: primary hyperparathyroidism and secondary hyperparathyroidism. Tertiary hyperparathyroidism is also identified, which occurs in patients with chronic renal failure receiving hemodialysis - but we will not consider it in this article.
Primary hyperparathyroidism is a condition when at the same time parathyroid hormone and calcium are elevated in the blood
. Additional symptoms of primary hyperparathyroidism are a decrease in blood phosphorus (not found in all cases) and an increase in the level of calcium in daily urine (also not in all cases). High parathyroid hormone in the blood in primary hyperparathyroidism is associated with the formation of a parathyroid adenoma - usually a benign tumor that produces parathyroid hormone uncontrollably. The increase in parathyroid hormone in the blood directly depends on the size of the adenoma - the larger it is, the higher the parathyroid hormone is detected. If a patient has primary hyperparathyroidism and parathyroid hormone is elevated - treatment is always surgical - removal of the adenoma gives excellent results, returning all components of phosphorus-calcium metabolism to normal limits.
When a patient has high parathyroid hormone, the causes of this condition may be associated with vitamin D deficiency (we talked about this earlier). If parathyroid hormone is increased in the blood, and calcium is normal or decreased
– most likely, we are talking about secondary hyperparathyroidism, associated with a low amount of vitamin D entering the body. Treatment of such an increase in parathyroid hormone is always carried out in a conservative way, taking vitamin D and calcium supplements.
It is very important, when understanding the reasons why parathyroid hormone is elevated, not to confuse secondary hyperparathyroidism with primary hyperparathyroidism - otherwise the patient will undergo an absolutely unnecessary surgical intervention, the results of which, of course, will not please either the doctor or the patient.
Consequences of exceeding the norm of the hormone in the blood
As we wrote above, recognizing hyperparathyroidism is not so easy. Therefore, up to 50% of people find out that their parathyroid hormone levels are elevated when they visit doctors for other reasons.
Reasons for seeking treatment are often related specifically to hyperfunction of the parathyroid gland:
- frequent fractures of limbs that do not heal well;
- formation of kidney stones, attacks of renal colic;
- calcium deposits occur in soft tissues - skin, blood vessels, heart muscle, muscles;
- flat bones (for example, ribs, phalanges of fingers) soften and are easily deformed;
- teeth become loose and fall out of the softened jaw bones;
- softening of the bones of the arch of the foot and lower extremities leads to lameness;
- destruction of the vertebral bodies is manifested by back pain, radicular syndromes - lumbago, radiculopathies with impaired skin sensitivity;
- articular cartilage ossifies, chondrocalcinosis develops, and human mobility suffers;
- stones are deposited in the ducts of the salivary glands and pancreas, in the latter case they can cause pancreatitis and pancreatic necrosis.
Now, thanks to laboratory diagnostics, many subclinical, mild forms of hyperparathyroidism are detected. For them, the only manifestations are depression, poor sleep, and a feeling of chronic fatigue. So if you have such symptoms, it won’t hurt to get tested. If parathyroid hormone is elevated, calcium is unlikely to be normal; then the level of this mineral must be examined.
Elevated parathyroid hormone - how to cure, where to cure?
For an accurate diagnosis, all patients are recommended to contact specialized centers for endocrinology and endocrine surgery, such as the North-Western Center for Endocrinology in St. Petersburg, the Russian leader in the treatment of hyperparathyroidism.
In our center, we annually consult several thousand patients whom doctors (!) refer for surgery to remove a parathyroid adenoma, but in fact the patients only have a deficiency or insufficiency of vitamin D, which is easily eliminated by taking pills. True, there are also the opposite situations, when patients with large parathyroid adenomas come to us for surgery, for whom the diagnosis has not been established for several years, which simply leads to catastrophic consequences for the body. Every year, several patients with increased parathyroid hormone due to adenoma require resuscitation due to the threat of coma. There are situations when patients undergo surgery on the very first day, the adenoma is removed, and then a two to three month course of resuscitation and restorative treatment is required - that is how far the pathological process goes.
In the vast majority of cases, patients from other regions of Russia at the North-Western Endocrinology Center undergo surgical treatment free of charge, under the federal quota system or simply under a compulsory health insurance policy. Outpatient examinations are carried out for a fee, but their cost is rarely high.
So, if you have elevated parathyroid hormone, it is wiser to come for examination and treatment to a specialized endocrinology center
where you will receive qualified assistance.
Signs of low parathyroid hormone levels
But there is also the opposite situation, when the amount of parathyroid hormone is reduced. What signs are observed in this case?
- poor sleep, or lack thereof;
- noticeable memory impairment;
- depression;
- tachycardia;
- pain in the heart area;
- uncontrollable muscle spasms that are very similar to an epileptic seizure;
- spasms in the bronchi or in other respiratory tracts, in the intestines;
- strong fever, chills in places.
Parathyroid hormone is low
The situation when parathyroid hormone is low
, occurs rarely in life. The main reason for a decrease in parathyroid hormone in the blood is a previous operation on the thyroid gland, during which the nearby small and not always clearly visible parathyroid glands were accidentally removed or deprived of blood supply.
Typically, when parathyroid hormone is low, symptoms
include numbness of the fingers and toes, the appearance of an unpleasant feeling of “goose bumps” on the skin, and the appearance of convulsive muscle contractions. The severity of these symptoms depends on the level of calcium in the blood - the lower they are, the worse the patient feels. In severe cases, generalized seizures may develop. If left untreated, the patient may die.
For a condition where parathyroid hormone is low, there is a special term - “hypoparathyroidism”. Many patients with a similar problem are trying to figure out how to increase parathyroid hormone
, however, whether an increase in parathyroid hormone will occur in the future or not after surgery usually depends only on how much injury was caused to the parathyroid glands. If restoration of the function of the parathyroid glands is possible, then it will certainly occur. However, during the entire time that parathyroid hormone is low, patients need to take vitamin D and calcium supplements - sometimes in quite large doses.
He's not even 50...
amino acid sequence of PTH in humans and some animals.
Conjectures about the significance of the parathyroid glands and the substance they produce were expressed at the dawn of the 20th century (1909) by the American professor of biochemistry McCollum. When observing animals with removed parathyroid glands, it was noted that under conditions of a significant decrease in calcium in the blood, they are overcome by tetanic convulsions, ultimately causing the death of the body. However, injections of calcium salt solutions given to experimental “our little brothers” suffering from convulsions, for a reason unknown at that time, helped to reduce convulsive activity and helped them not only survive, but also return to an almost normal existence.
Some clarification regarding the mysterious substance appeared 16 years later (1925), when an extract was discovered that had biologically active (hormonal) properties and increased the level of Ca in the blood plasma.
However, many years passed, and only in 1970 pure parathyroid hormone was isolated from the parathyroid glands of a bovine. At the same time, the atomic structure of the new hormone was designated along with its connections (primary structure). In addition, it turned out that PTH molecules consist of 84 amino acids arranged in a specific sequence and one polypeptide chain.
As for the parathyroid hormone “factory” itself, it would be a stretch to call it a factory, it is so small. The number of “peas” in the upper and lower parts in total varies from 2 to 12 pieces, but 4 is considered the classic option. The weight of each piece of iron is also very small - from 25 to 40 milligrams. When the thyroid gland (TG) is removed due to the development of an oncological process, the parathyroid glands (PTG), as a rule, leave the patient’s body along with it. In other cases, during operations on the thyroid gland, these “peas” are removed by mistake due to their size.