Octreotide, 50 mcg/ml, solution for intravenous and subcutaneous administration, 1 ml, 5 pcs.
Octreotide is a synthetic analogue of somatostatin, which is a derivative of the natural hormone somatostatin and has pharmacological effects similar to it, but a significantly longer duration of action. Octreotide suppresses the secretion of growth hormone, both pathologically increased and caused by arginine, exercise and insulin hypoglycemia. The drug also suppresses the secretion of insulin, glucagon, gastrin, serotonin, both pathologically increased and caused by food intake; also suppresses the secretion of insulin and glucagon stimulated by arginine. Octreotide suppresses the secretion of thyrotropin caused by thyrotropin-releasing hormone. Unlike somatostatin, octreotide suppresses growth hormone secretion to a greater extent than insulin secretion, and its administration is not accompanied by subsequent hypersecretion of hormones (for example, growth hormone in patients with acromegaly).
In patients with acromegaly, octreotide reduces the concentration of growth hormone and insulin-like growth factor (IGF-1) in the blood plasma. A decrease in the concentration of growth hormone by 50% or more is observed in 90% of patients, while a growth hormone concentration of at least 5 ng/ml is achieved in approximately half of the patients. In most patients with acromegaly, octreotide reduces the severity of headache, soft tissue swelling, hyperhidrosis, joint pain and paresthesia. In patients with large pituitary adenomas, treatment with octreotide may lead to some reduction in tumor size.
For secreting tumors of the gastroenteropancreatic endocrine system, in cases of insufficient effectiveness of the therapy (surgery, embolization of the hepatic artery, chemotherapy, including streptozotocin and fluorouracil), the administration of octreotide can lead to an improvement in the course of the disease. Thus, in carcinoid tumors, the use of octreotide can lead to a decrease in the severity of the sensation of flushing and diarrhea, which in many cases is accompanied by a decrease in the concentration of serotonin in plasma and the excretion of 5-hydroxyindoleacetic acid by the kidneys. For tumors characterized by overproduction of vasoactive intestinal peptide (VIP), the use of octreotide in most patients leads to a reduction in severe secretory diarrhea and, accordingly, an improvement in the patient’s quality of life. At the same time, there is a decrease in concomitant electrolyte imbalances, such as hypokalemia, which makes it possible to cancel enteral and parenteral administration of fluids and electrolytes. In some patients, tumor progression slows down or stops, its size decreases, as does the size of liver metastases. Clinical improvement is usually accompanied by a decrease in the plasma concentration of vasoactive intestinal peptide (VIP) or its normalization. For glucagonomas, the use of octreotide leads to a decrease in erythema migrans. Octreotide does not have any significant effect on the severity of hyperglycemia in diabetes mellitus, while the need for insulin or oral hypoglycemic drugs usually remains unchanged. The drug causes a decrease in diarrhea, which is accompanied by an increase in body weight. Although the decrease in plasma glucagon concentrations under the influence of octreotide is transient, clinical improvement remains stable throughout the period of drug use. In patients with gastrinomas/Zollinger-Ellison syndrome, when using octreotide as monotherapy or in combination with proton pump inhibitors or H2-histamine receptor blockers, it is possible to reduce the hypersecretion of hydrochloric acid in the stomach, reduce the concentration of gastrin in the blood plasma, as well as reduce the severity of diarrhea and tides In patients with insulinomas, octreotide reduces the level of immunoreactive insulin in the blood (this effect can be short-term - about 2 hours). In patients with operable tumors, octreotide can restore and maintain normoglycemia in the preoperative period. In patients with inoperable benign and malignant tumors, glycemic control may improve without a simultaneous prolonged decrease in blood insulin levels.
In patients with rare tumors that overproduce growth hormone releasing factor (somatoliberinomas), octreotide reduces the severity of symptoms of acromegaly. This is due to the suppression of the secretion of growth hormone releasing factor and growth hormone itself. In the future, pituitary hypertrophy may decrease.
For bleeding from varices of the esophagus and stomach in patients with liver cirrhosis, the use of octreotide in combination with specific treatment (for example, sclerotherapy) leads to more effective stoppage of bleeding and early rebleeding, a reduction in the volume of transfusions and an improvement in 5-day survival. The mechanism of action of octreotide is believed to be associated with a decrease in organ blood flow through the suppression of vasoactive hormones such as VIP and glucagon.
Pharmacokinetics
Suction
After subcutaneous administration, octreotide is rapidly and completely absorbed. Tmax of octreotide in plasma is within 30 minutes.
Distribution
The connection with blood plasma proteins is 65%. The binding of octreotide to blood cells is extremely insignificant. Vd is 0.27 l/kg.
Removal
T1/2 after subcutaneous administration of octreotide is 100 minutes. After intravenous administration, octreotide is eliminated in 2 phases, with T1/2 - 10 and 90 minutes, respectively. Most of octreotide is excreted through the intestines, about 32% is excreted unchanged by the kidneys. The total clearance is 160 ml/min.
Release form and composition
Dosage form - solution for intravenous and subcutaneous administration: transparent, colorless, odorless [1 ml in ampoules: at a dose of 50 and 100 mcg/ml - 5 ampoules in blister packs, 1 or 2 packs in a cardboard pack; at a dose of 300 and 600 mcg/ml - 1, 2 or 5 ampoules in blister packs, in a cardboard pack 1 (1, 2 or 5 ampoules) or 2 (5 ampoules) packs; Each pack also contains instructions for using Octreotide].
The active substance is octreotide (in the form of acetate), its content in 1 ml of solution is 50, 100, 300 or 600 mcg.
Inactive components: sodium chloride and injection water.
Side effects
Criteria for assessing the frequency of side effects: very often - no more than 1 case out of 10, often - ≥1/100, but <1/10, sometimes - ≥1/1000, but <1/100.
Adverse reactions identified during clinical trials of Octreotide:
- From the digestive system: very often - diarrhea or constipation, bloating, nausea, abdominal pain; often – steatorrhea, change in stool color, feeling of fullness or heaviness in the abdomen, soft stool consistency, dyspeptic disorders, anorexia, vomiting;
- From the hepatobiliary system: gallstones (cholelithiasis); often - increased activity of liver transaminases, cholecystitis, hyperbilirubinemia, formation of cholesterol microcrystals due to a violation of the colloidal stability of bile;
- From the cardiovascular system: often – bradycardia; sometimes – tachycardia;
- From the endocrine system: very often – hyperglycemia; often - hypoglycemia, impaired glucose tolerance, hypothyroidism, dysfunction of the thyroid gland (manifested by a decrease in the levels of thyroid-stimulating hormone, total and free thyroxine);
- From the respiratory system: often – shortness of breath;
- From the nervous system: very often – headache; often - dizziness;
- Dermatological reactions: often - rash, itching, hair loss;
- Local reactions: very often – pain at the injection site;
- Other: sometimes – dehydration.
The cause-and-effect relationship of the following side effects with the use of Octreotide has not been established:
- From the hepatobiliary system: cholestasis, jaundice, cholestatic hepatitis, acute hepatitis without cholestasis, cholestatic jaundice, acute pancreatitis, increased levels of gamma-glutamyltransferase and alkaline phosphatase;
- From the immune system: hypersensitivity reactions, anaphylactic reactions;
- From the cardiovascular system: arrhythmias;
- Dermatological reactions: urticaria.
special instructions
Women of childbearing age with acromegaly should use reliable methods of contraception during therapy, because with a decrease in the level of growth hormone and normalization of the level of IGF-1 under the influence of octreotide, restoration of reproductive function is possible.
With long-term treatment, it is necessary to monitor thyroid function.
In patients with a history of vitamin B12 deficiency, it is necessary to monitor the level of cobalamin in the body.
Before prescribing Octreotide, patients should be referred for an ultrasound examination of the gallbladder. If stones are detected, the drug can be prescribed after a careful assessment of the expected benefits of therapy and possible risks. Repeat examinations should be performed every 6-12 months during treatment.
If stones are detected during treatment:
- Asymptomatic: you can discontinue the drug or continue therapy after assessing the benefit/risk ratio. There is no need to take any measures, more frequent monitoring is required;
- With clinical symptoms: you can discontinue the drug or continue treatment after assessing the benefit/risk ratio. Patients require standard therapy for gallstone disease (including bile acid preparations) and regular ultrasound monitoring.
Patients with growth hormone-secreting pituitary tumors require close medical monitoring during treatment, as the drug may cause the tumor to increase in size and develop serious complications such as narrowing of visual fields. If this occurs, it is necessary to consider the use of other treatment methods.
Octreotide may interfere with the absorption of fats in the intestines.
If bradycardia develops, it is necessary to consider reducing the dose of calcium channel blockers, beta-blockers or drugs that affect water and electrolyte balance.
It should be remembered that Octreotide is not an antitumor agent, and therefore does not help cure secreting endocrine tumors of the pancreas and gastrointestinal tract.
When treating endocrine tumors of the gastrointestinal tract and pancreas, sudden relapse is possible in some cases. If insulinoma develops during use of octreotide, the duration and severity of hypoglycemia may increase. Such patients should be closely monitored, especially whenever the dose of the drug is changed.
Octreotide affects blood glucose concentrations. Fluctuations can be reduced by administering the drug more frequently in smaller doses. In type 1 diabetes mellitus, the drug can reduce the need for insulin; in type 2 diabetes (with partially preserved insulin secretion) and in patients without diabetes, it can lead to the development of postprandial hyperglycemia. For this reason, patients with diabetes need monitoring of blood glucose levels and antidiabetic therapy.
Patients also need to monitor the concentration of glucose in the blood after bleeding from varicose veins of the stomach or esophagus, since in this case the risk of developing type 1 diabetes mellitus increases.
Impact on the ability to drive vehicles and complex mechanisms
Due to the risk of developing side effects from the central nervous system, it is recommended to exercise caution when driving a car and performing any work that requires increased attention and speed of reactions.
Octreotide, instructions for use: method and dosage
Octreotide is intended for subcutaneous (SC) and intravenous (IV) administration.
Prescribed dosage regimens depending on the indications and purpose of use:
- Treatment of acute pancreatitis: 100 mcg subcutaneously 3 times a day for 5 days. In some cases, the doctor may recommend intravenous administration of the drug in a daily dose of up to 1200 mcg;
- Prevention of complications after pancreatic surgery: 100-200 mcg s.c. The first dose is administered 1-2 hours before laparotomy, after surgery - 3 times a day for 5-7 days;
- Stopping ulcer bleeding: 25-50 mcg/hour as an intravenous infusion, course – 5 days;
- Stopping bleeding from varicose veins of the esophagus and stomach: 25-50 mcg/hour as a continuous IV infusion, course of treatment – 5 days;
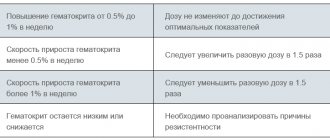
- Acromegaly: initial dose – 50-100 mcg subcutaneously every 8 or 12 hours. In case of ineffectiveness (the target concentration of growth hormone is less than 2.5 ng/ml, and the IGF-1 value is within normal values), the single dose is increased to 300 mcg. The maximum permissible daily dose is 1500 mcg. In patients receiving octreotide at a stable dose, growth hormone levels should be determined every 6 months. If after 3 months of treatment there is no sufficient reduction in this indicator and improvement in the clinical course of the disease, Octreotide should be discontinued;
- Tumors of the gastroenteropancreatic endocrine system: initial dose - 50 mcg 1-2 times a day, if necessary, it is gradually increased to 100-200 mcg 3 times a day subcutaneously. In case of ineffectiveness (assessed based on data on the achieved clinical effect, the concentration of hormones that produce the tumor, and tolerability of the drug), the dose is increased to 300 mcg subcutaneously 1-2 times a day. In exceptional cases, it is possible to increase the dose even further - up to 300-600 mcg 3 times a day. The doctor selects maintenance doses for each patient individually. If, for carcinoid tumors, therapy at the maximum tolerated dose is ineffective within 1 week, Octreotide is discontinued.
Patients with impaired liver function require adjustment of the maintenance dose.
Rules for subcutaneous administration of Octreotide:
- Carefully inspect the ampoule for the presence of foreign impurities and color changes in the solution;
- Warm the ampoule to room temperature;
- Open the ampoule immediately before administration;
- Throw away any unused amount of solution;
- Do not inject into the same place at short intervals.
Rules for intravenous drip administration:
- Carefully inspect the ampoule for foreign impurities and color changes;
- Warm the solution to room temperature;
- For dilution, use 0.9% sodium chloride (for example, 1 ampoule of 600 mcg is diluted with 60 ml of saline);
- Prepare the injection solution immediately before administration;
- If necessary, store for no more than 24 hours after dilution in the refrigerator (at a temperature of 2 to 8 ºС).
Drug interactions
Effect of octreotide on concomitantly taken substances/drugs:
- Cyclosporine - reduces its absorption;
- Bromocriptine – increases its bioavailability;
- Cimetidine - slows down its absorption;
- Drugs metabolized by the cytochrome P450 system (terfenadine, quinidine) reduce their metabolism.
When combining octreotide with diuretics, oral hypoglycemic drugs, insulin, blockers of “slow” calcium channels, and beta-blockers, adjustment of the dosage regimen is required.
Contraindications
The use of Octreotide is strictly contraindicated in children and adolescents under 18 years of age, as well as in all patients who have hypersensitivity to any component of the drug.
The drug should be used with caution when treating patients with diabetes mellitus and cholelithiasis (cholelithiasis).
The effect of the drug on the course of pregnancy has not been studied, so its use is possible only in extreme cases, if the expected benefits outweigh the possible risks.
It is unknown whether octreotide passes into breast milk, so it is recommended that you avoid breastfeeding during treatment.