Pathologies of the cardiovascular system are considered one of the main conditions leading to death in patients around the world. With minor changes, the sad statistics remain on the planet.
As a result of many conditions of this profile, irreversible organic transformations of muscle fibers occur: the actual functional tissues.
Cardiosclerosis is the process of replacing normal cells, myocytes, with scar cells. The latter are not capable of contraction or spontaneous excitation. Hence the decline in the functional activity of the heart in general. Contractility and blood flow decrease, and tissue ischemia occurs.
The process is irreversible, but it is possible to maintain the condition at a stable level for a long time. Patients with cardiosclerosis undergo lifelong drug treatment under the supervision of a cardiologist.
The prognosis is relatively favorable. Significantly worsen against the background of extensive damage to cardiac structures. Recovery is carried out using conservative methods.
General information. Cardiosclerosis - what is it and how to treat it
Cardiosclerosis is understood as a chronic heart disease that develops due to excessive growth of connective tissue in the thickness of the myocardium .
The number of muscle cells themselves also decreases noticeably. Cardiosclerosis is not an independent disease, because formed as a result of other pathologies. It would be more correct to consider cardiosclerosis a complication that seriously disrupts the functioning of the heart.
The disease is chronic and has no acute symptoms. Cardiosclerosis is provoked by a large number of causes and factors, so it is quite difficult to determine its prevalence. The main signs of the disease are found in most cardiac patients. Diagnosed cardiosclerosis always worsens the patient's prognosis, because replacement of muscle fibers with connective tissue is an irreversible process.
The mechanism of pathology development
Cardiosclerosis does not develop in a patient who has never felt a heart problem. Many people simply do not concentrate on heart pathologies, especially if their symptoms do not particularly interfere with life and work, and often attribute the ailment to temporary overwork.
Due to failure to treat pathologies of the heart organ, as well as pathologies of the blood flow system (hypertension, high cholesterol in the blood), the development of a secondary type of pathology, cardiosclerosis, occurs.
Cardiac fibrosis is a scar on the muscle of the heart organ made of fibrous tissue, which can simply be a framework for destroyed cardiomyocytes, but it cannot replace them.
Minor destruction of the myocardium can occur in elderly people. If focal sclerosis does not occupy a large area on the myocardium, or the lesions are single, then there are no pronounced symptoms, and scarring does not disrupt the normal functioning of the myocardium and its contractile abilities.
When scarring occurs over a large area of the cardiac myocardium, or fibrosis affects important structures within the heart, or is in the path of the pacemaker, then this leads to dysfunction and develops cardiac organ failure with all its signs and symptoms.
Cardiac fibrosis
Pathogenesis
The development of cardiosclerosis is based on 3 mechanisms:
- Dystrophic changes. They are formed as a result of disturbances in the trophism and nutrition of the myocardium due to developed cardiovascular disease ( cardiomyopathy , atherosclerosis , chronic ischemia or myocardial dystrophy ). , diffuse cardiosclerosis develops .
- Necrotic processes . Develop after heart attacks , injuries and damage that occurred during heart surgery. , focal cardiosclerosis develops .
- Myocardial inflammation. The process starts as a result of the development of infectious myocarditis , rheumatism and leads to the formation of diffuse or focal cardiosclerosis.
What is aortocardiosclerosis?
Aortocardiosclerosis is an outdated term that is no longer used in medicine due to the transition to the international classification of diseases. At the moment, the official name of this disease is cardiosclerosis .
If damage to the heart muscle cells occurs, dense scar tissue consisting of connective tissue begins to grow at the site of these defects. Such tissue cannot perform the functions necessary for the heart.
At first, the remaining and healthy cells also do the work for the damaged cells, but over time their nutrition is disrupted, which leads to death and scarring.
The more scar tissue becomes, the faster the heart muscle loses its ability to work, the heart rhythm is disrupted (due to the fact that the damaged areas of the muscle cannot distribute contraction control impulses that come from the brain) and contractile function is lost.
Classification
Cardiosclerosis is classified according to the reasons that will be listed and described below in the appropriate section, by the intensity of the process and by localization. Depending on the classification, the course of the disease changes, different functions of the heart are affected.
Based on intensity and localization, they are distinguished:
- focal cardiosclerosis;
- diffuse cardiosclerosis (total);
- with damage to the valvular apparatus of the heart.
Focal cardiosclerosis
Focal damage to the heart muscle is observed after a myocardial infarction . Less commonly, focal cardiosclerosis forms after localized myocarditis. Characterized by a clear limitation of the lesion in the form of scar tissue, which is surrounded by healthy cardiomyocytes that are capable of fully performing all their functions.
Factors influencing the severity of the disease:
- Depth of damage . Determined by the type of myocardial infarction suffered. With a superficial lesion, only the outer layers of the wall are damaged, and after the formation of a scar, a fully functioning muscle layer remains underneath. With transmural lesions, necrosis affects the entire thickness of the muscle. The scar is formed from the pericardium to the cavity of the heart chamber. This option is considered the most dangerous, because... with it there is a high risk of developing such a serious complication as a cardiac aneurysm.
- Sizes of the hearth. The larger the area of myocardial damage, the more pronounced the symptoms and the worse the prognosis for the patient. There are small-focal and large-focal cardiosclerosis. Single small inclusions of scar tissue may not produce absolutely any symptoms and may not affect the functioning of the heart or the patient’s well-being. Large-focal cardiosclerosis is fraught with consequences and complications for the patient.
- Localization of the outbreak. Depending on the location of the source, dangerous and non-hazardous are determined. The location of a small area of connective tissue in the interventricular septum or in the atrium wall is considered harmless. Such scars do not affect the basic functioning of the heart. Damage to the left ventricle, which performs the main pumping function, is considered dangerous. Number of lesions. Sometimes several small foci of scar tissue are diagnosed at once. In this case, the risk of complications is directly proportional to their number.
- State of the conduction system. Connective tissue not only does not have the necessary elasticity, compared to muscle cells, but is also unable to conduct impulses at the required speed. If scar tissue has affected the conduction system of the heart, then this is fraught with the development of arrhythmias and various blockades. Even if only one wall of the heart chamber lags during the contraction process, the ejection fraction, the main indicator of the contractility of the heart, decreases.
From the above it follows that the presence of even small foci of cardiosclerosis can lead to negative consequences. Timely and competent diagnosis of myocardial damage is required to select appropriate treatment tactics.
Diffuse cardiosclerosis
Connective tissue accumulates in the heart muscle everywhere and evenly, which makes it difficult to isolate specific lesions. Diffuse cardiosclerosis most often occurs after toxic, allergic and infectious myocarditis, as well as with coronary heart disease.
Diffuse cardiosclerosis
The alternation of normal muscle fibers and connective tissue is characteristic, which prevents the heart muscle from fully contracting and performing its function. The walls of the heart lose their elasticity, do not relax well after contraction, and do not stretch well when filled with blood. Such disorders are often referred to as restrictive (compressive) cardiomyopathy .
Cardiosclerosis with damage to the valve apparatus
It is extremely rare that sclerosis affects the valve apparatus of the heart. Valves are involved in the process in rheumatological and systemic diseases.
Types of valve damage:
- Valve insufficiency. Characterized by incomplete closure and closure of the valves, which makes it difficult to eject blood in the desired direction. Through a poorly functioning valve, blood returns back, which reduces the volume of pumped blood and leads to the development of heart failure. In cardiosclerosis, valve insufficiency is formed due to deformation of the valve leaflets.
- Valve stenosis. Due to the proliferation of connective tissue, the lumen of the valve narrows. Blood does not flow in sufficient volume through the narrowed opening. The pressure in the heart cavity increases, which leads to serious structural changes. Thickening of the myocardium (hypertrophy) is observed as a compensatory reaction of the body.
In cardiosclerosis, the valvular apparatus of the heart is affected only in a diffuse process that involves the endocardium.
What changes occur in the vessel when it is compacted?
The aorta is an elastic type vessel, that is, its wall contains a large number of connective tissue fibers. She needs this to perform two main functions. Firstly, it stretches quite well, which allows you to maintain diastolic pressure.
It is because of the distensibility of the aorta that blood flows not in spurts, but in a continuous stream, which allows blood to be supplied to the internal organs. This is especially true for the myocardium, which is 85% supplied in the diastole phase.
Secondly, the high content of elastic fibers allows the aorta to withstand the enormous pressure that the blood ejected from the left ventricle exerts on it.
In various diseases, the vessel becomes denser due to the fact that the balance between elastic and collagen fibers shifts towards the latter. Also, in some pathologies, calcium begins to actively deposit in the aortic wall, making it hard.
When the aorta becomes sclerotic, its distensibility decreases, and therefore its ability to maintain diastolic blood pressure at the proper level. This leads to deterioration of blood circulation in internal organs, especially the heart. To correct this, the body has to compensatoryly increase systolic blood pressure through tachycardia and increased peripheral vascular resistance.
The result of such a chain of pathological reactions is the development of so-called isolated systolic arterial hypertension, or the aggravation of existing hypertension.
Due to the poor elasticity of the aorta, the “water hammer” of the blood is not softened, its gradual expansion (dilatation) occurs, and the risk of an aneurysm increases, which can rupture at any time and lead to death.
Causes
The transition of cardiomyocytes into connective tissue occurs due to the inflammatory process. In this case, the formation of connective tissue fibers is a kind of protective mechanism.
Depending on the reasons, several groups are distinguished:
- atherosclerotic form;
- post-infarction cardiosclerosis;
- myocardial form;
- other reasons.
Atherosclerotic cardiosclerosis
Includes diseases that lead to cardiosclerosis through long-term ischemia and ischemic heart disease. Atherosclerotic cardiosclerosis is not classified in a separate category according to ICD-10.
Coronary heart disease develops as a result of atherosclerosis of the coronary arteries. When the lumen of the vessel narrows, the myocardium ceases to receive normal blood supply. The narrowing occurs due to the deposition of cholesterol and the formation of an atherosclerotic plaque, or due to the presence of a muscular bridge over the coronary vessel.
With prolonged ischemia , connective tissue begins to grow between cardiomyocytes and cardiosclerosis forms. It is important to understand that this is a rather long process and most often the disease is asymptomatic. The first signs begin to appear only when a significant part of the heart muscle is filled with connective tissue. The cause of death is the rapid progression of the disease and the development of complications.
Myocardial form (Postmyocardial cardiosclerosis)
The mechanism of development of myocardial cardiosclerosis is completely different. A lesion forms at the site of former inflammation after myocarditis. This type of cardiosclerosis is characterized by:
- young age;
- history of allergic and infectious diseases;
- the presence of foci of chronic infection.
ICD-10 code for postmyocardial cardiosclerosis: I51.4.
The disease develops due to proliferative and exudative processes in the myocardial stroma, due to destructive changes in the myocytes themselves. With myocarditis, a huge amount of substances are released that have a damaging effect on the membranes of muscle cells. Some of them are destroyed. After recovery, the body, as a protective reaction, increases the production and volume of connective tissue. Myocardial cardiosclerosis develops much faster than atherosclerosis. The myocardial variant is characterized by damage to young people.
Post-infarction cardiosclerosis
Formed at the site of death of cardiomycytes after acute myocardial infarction. When blood access through the coronary artery to the heart muscle is stopped, necrosis of the corresponding area develops. The area may be of different locations depending on which vessel is blocked. Depending on the caliber of the vessel, the size of the affected area also changes. As a compensatory reaction, the body begins increased production of connective tissue at the site of the lesion. The code for post-infarction cardiosclerosis according to ICD-10 is I25.2.
The prognosis for survival after a heart attack depends on many factors. The cause of death after a heart attack lies in complications of the disease and lack of adequate therapy. Post-infarction syndrome is an autoimmune reaction that complicates myocardial infarction and is manifested by symptoms of inflammation of the pericardium, lungs and pleura.
Postpericardiotomy syndrome is an inflammatory autoimmune disease of the pericardium that develops after open heart surgery.
Other reasons
In addition to those described above, there are other reasons that are more rare.
- Radiation exposure. Under the influence of radiation exposure, changes occur in a variety of organs and tissues. After irradiation of the heart muscle, irreversible changes and complete restructuring occur in cardiomyocytes at the molecular level. Gradually, connective tissue begins to form, its proliferation and the formation of cardiosclerosis. The pathology can develop lightning fast (within several months after strong radiation) or slowly (several years after exposure to a low dose of radiation).
- Sarcoidosis of the heart. A systemic disease that can affect a wide variety of organs and tissues. In the cardiac form, inflammatory granulomas form in the myocardium. With proper therapy, these formations disappear, but in their place, pockets of scar tissue can form. Thus, focal cardiosclerosis is formed.
- Hemochromatosis. This disease is characterized by the deposition of iron in the tissues of the heart. Gradually, the toxic effect increases, an inflammatory process develops, which ends with the proliferation of connective tissues. With hemochromatosis, cardiosclerosis affects the entire thickness of the myocardium. In more severe cases, the endocardium is also damaged.
- Idiopathic cardiosclerosis. This concept includes cardiosclerosis, which has developed for no apparent reason. It is assumed that it is based on as yet unknown mechanisms. The likelihood of the influence of hereditary factors that provoke increased growth of connective tissue at a certain stage of the patient’s life is considered.
- Scleroderma. Damage to the heart muscle in scleroderma is one of the most dangerous complications of the disease. Connective tissue begins to grow from the capillaries that the heart muscle is so rich in. Gradually, the size of the heart increases against the background of constant thickening of the walls. Traditional signs of destruction of cardiomyocytes and the presence of an inflammatory process are not recorded.
There are many mechanisms and reasons for triggering the proliferation of connective tissue in the myocardium. It is quite difficult to reliably establish the true cause of the disease. However, identifying the root cause of the pathology is simply necessary to prescribe the correct treatment.
Prognostic assessments
Prognosis varies depending on the extent of the lesion. The form of the process also affects.
Thus, atherosclerotic cardiosclerosis is the cause of death in 3-6% at the early stage, in 17-30% at the late stage. This is a relatively easy variety.
Deviations against the background of a heart attack or inflammation have a worse outcome. In figures, the mortality rate is 40-50% over the course of several years, the risk may be greater. With treatment, the chances of survival increase.
The prognosis is assessed by a specialist, but not immediately. Need observation. Both the course of the process and the response to the therapy play a role.
Symptoms of cardiosclerosis of the heart
In the first stages of the disease, cardiosclerosis can be practically asymptomatic. The gradual proliferation of connective tissue negatively affects the elasticity of muscle tissue, the contractile force of the myocardium decreases, the cavities stretch, and the conduction system of the heart is damaged. Focal cardiosclerosis after a heart attack can proceed almost asymptomatically if the area of damage was small in area and located superficially. The main symptoms in the initial stages are not associated with cardiosclerosis, but with the underlying disease, which provokes the proliferation of connective tissue.
The main symptoms of cardiosclerosis:
- dyspnea;
- arrhythmia;
- cardiopalmus;
- dry cough;
- excessively rapid fatigue;
- dizziness;
- swelling of the limbs and body.
Dyspnea
Shortness of breath is one of the main manifestations of heart failure that accompanies cardiosclerosis. It does not manifest itself immediately, but years after the start of connective tissue growth. Shortness of breath increases most quickly after myocarditis or myocardial infarction, when the rate of progression of cardiosclerosis is maximum.
Shortness of breath with cardiosclerosis
Shortness of breath manifests itself in the form of respiratory failure. The patient has difficulty breathing normally. In some cases, shortness of breath is accompanied by chest pain, coughing and a feeling of rapid and irregular heartbeat. The mechanism for the appearance of shortness of breath is quite simple: with cardiosclerosis, the pumping function of the heart is impaired. With reduced elasticity, the chambers of the heart cannot absorb all the blood that flows to them, so fluid stagnation develops in the pulmonary circulation. There is a slowdown in gas exchange and, as a result, impaired respiratory function.
Shortness of breath most often occurs during physical activity, during stress, and while lying down. It is impossible to completely eliminate the main symptom of cardiosclerosis, because characteristic changes in the myocardium are irreversible. As the disease progresses, shortness of breath begins to bother patients even at rest.
Cough
Cough occurs due to stagnation in the pulmonary circulation. The walls of the bronchial tree swell, fill with fluid and thicken, irritating the cough receptors. In cardiosclerosis, stagnation is weakly expressed, so accumulation of water in the alveoli is observed quite rarely. A dry cough occurs for the same reasons as shortness of breath. With proper treatment, you can almost completely get rid of a dry, hacking and unproductive cough. Cough with cardiosclerosis is often called “cardiac”.
Arrhythmias and palpitations
Rhythm disturbances are recorded in cases where the connective tissue damages the conduction system of the heart. The conduction pathways that normally carry uniform rhythms are damaged. There is an inhibition of the contraction of certain areas of the myocardium, which negatively affects the blood flow as a whole. Sometimes contraction occurs before the chambers are filled with blood. All this leads to the fact that the required volume of blood does not reach the next section. With uneven contraction of muscle tissue, increased mixing of blood in the cavities of the heart is observed, which significantly increases the risk of thrombosis.
Most often, patients with cardiosclerosis experience:
- tachycardia;
- bradycardia;
- extrasystolic arrhythmia;
- atrial fibrillation.
Arrhythmias appear with severe cardiosclerosis. With small areas of cardiosclerosis or with moderate diffuse proliferation of connective tissue, the conducting fibers of the system are not affected. Arrhythmias worsen the life prognosis of a patient suffering from cardiosclerosis, because significantly increase the risk of developing serious complications.
With palpitations, the patient feels his heart beating at the level of the neck or in the abdomen. Upon careful examination, you can pay attention to visible pulsation near the lower point of the sternum (the area of the xiphoid process).
Fast fatiguability
When pumping function is impaired, the heart loses its ability to pump out a sufficient volume of blood with each contraction, and blood pressure becomes unstable. Patients complain of rapid fatigue not only during physical, but also during mental stress. When performing physical exercises or walking, the muscles cannot cope with the load due to insufficient oxygen supply. During mental activity, a negative factor is oxygen starvation of the brain, which leads to decreased concentration, attention and memory impairment.
Edema
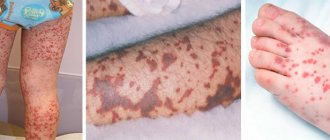
Swelling appears in the later stages with severe cardiosclerosis. Edema is formed due to stagnation in the systemic circulation, with inadequate functioning of the right ventricle. It is into this part of the heart that venous blood enters and stagnates when the heart chamber is unable to pump the required volume of blood.
First of all, swelling appears in those areas where blood circulation is slow and blood pressure . Under the influence of gravity, edema most often forms in the lower extremities. First, there is expansion and swelling of the veins in the legs, then the fluid leaves the vascular bed and begins to accumulate in the soft tissues, forming edema. At first, swelling is observed only in the morning, because due to mechanical movements, blood flow accelerates and swelling goes away. In later stages, as heart failure progresses, edema is observed throughout the day and evening.
Dizziness
At later stages, not only mild dizziness is recorded, but also occasional fainting , which is a consequence of oxygen starvation of the brain. Fainting occurs due to a sharp drop in blood pressure or serious heart rhythm disturbances. The central nervous system does not receive enough nutrients. Fainting in this case is a defensive reaction - the body saves energy in order to function on the volume of oxygen that a sick heart can provide.
Tests and diagnostics
At the initial stages of the disease, diagnosing cardiosclerosis causes certain difficulties. Most diagnostic examination techniques do not detect small accumulations of connective tissue among healthy cardiomyocytes. In addition, patients do not present any specific complaints. That is why cardiosclerosis is most often diagnosed in the later stages, when heart failure and other complications of the disease occur.
Only patients who have suffered myocarditis or myocardial infarction undergo targeted and timely examination. In this category of patients, myocardial sclerosis is a predictable and expected consequence.
Basic diagnostic methods:
- objective examination by a doctor;
- ECG;
- EchoCG;
- chest x-ray;
- scintigraphy;
- MRI or CT;
- specific laboratory tests.
Objective examination
It is the first step towards diagnosis. The examination is carried out by a therapist or cardiologist during communication with the patient. During examination, it is impossible to diagnose cardiosclerosis itself, but the disease can be suspected if there are signs of heart failure. The doctor examines the patient, performs palpation, auscultation, history taking and percussion.
Electrocardiography
Allows you to evaluate the bioelectrical activity of the heart. Characteristic changes on the ECG in cardiosclerosis:
- reduced voltage of the teeth of the QRS complex (an indicator of impaired ventricular contractility);
- reduction of the “T” wave or its negative polarity;
- decrease in the ST segment below the isoline;
- rhythm disturbances;
- blockades
The ECG should be assessed by an experienced cardiologist who can, based on the nature of changes in electrical impulses, determine the location of the lesion, the form of cardiosclerosis and diagnose complications.
EchoCG
It is the most informative method in assessing heart function. Ultrasound of the heart is a painless and non-invasive procedure that allows you to determine the morphological state of the heart muscle, evaluate its pumping function, contractility, etc.
Characteristic changes in patients with cardiosclerosis:
- conduction disturbance;
- impaired contractility;
- thinning of the heart wall in the area of sclerosis;
- focus of fibrosis or sclerosis, its location;
- disturbances in the functioning of the valvular apparatus of the heart.
Radiography
X-ray is unable to clearly display all changes in the heart during cardiosclerosis, and therefore is an optional diagnostic method. Most often, R-graphy is used to make a preliminary diagnosis for the purpose of further examination. The method is painless, but is contraindicated for pregnant women due to the small dose of radiation. Pictures are taken in two projections to evaluate the heart from both sides. In the later stages of cardiosclerosis, the heart is noticeably enlarged. An experienced doctor can even see large aneurysms on X-rays.
Computed tomography and magnetic resonance imaging
They represent high-precision methods for studying the structures of the heart. The diagnostic significance of CT and MRI is equivalent, despite the different principles of image acquisition. The images allow you to see even small foci of connective tissue spread in the myocardium (most often after a heart attack). Diagnosis is difficult with diffuse process of damage to the heart muscle, because changes in myocardial density are uniform. The difficulty in examining the heart using CT and MRI methods is due to the fact that the heart is in constant motion, which does not allow obtaining a clear picture.
Scintigraphy
An instrumental examination method based on the introduction of a special substance into the bloodstream that marks certain types of cells. The target for the administered substance in case of cardiosclerosis is healthy cardiomyocyte cells. The contrast does not accumulate in damaged cells, or accumulates in smaller quantities. After the substance is administered, pictures of the heart are taken, which show how the contrast is distributed in the heart muscle.
Myocardial scintigraphy
In healthy myocardium, the injected substance accumulates evenly. Areas of damage in focal cardiosclerosis are very clearly visible - there will be no accumulation of contrast in them. The examination is informative and practically safe (with the exception of allergic responses to a contrast agent). The disadvantage of scintigraphy is the low prevalence of the method due to the high cost of the equipment.
Laboratory research methods
In the TAM and OAK, no specific changes are usually observed. Laboratory examination methods allow us to find the cause of the development of cardiosclerosis. For example, with atherosclerosis, the patient will have increased cholesterol; with myocarditis, there will be signs of an inflammatory process in the CBC. The data obtained during a laboratory examination of the patient only allows one to suspect the disease based on indirect signs. Drug therapy cannot be started without assessing the functioning of the renal and hepatic systems, for which a biochemical blood test, OBC, and OAM are performed.
Diagnostic measures
The development of atherosclerotic lesions of the coronary vessels can be suspected during an ECG, which detects signs of ischemia of the heart muscle.
To confirm atherosclerosis of the coronary arteries of the heart, the following studies are performed:
- Stress scintigraphy. The method makes it possible to establish the localization of lipid neoplasms on the intima of blood vessels and the degree of their severity;
- Intravascular ultrasound and Doppler ultrasound. Allows to identify changes in the structure of blood vessels: wall thickness, chamber size, the presence of sections with impaired contractility, assess hemodynamics and valve morphology;
- Coronary angiography. It is an X-ray examination of the heart with contrast. The method helps determine the location and length of the affected vessels, the degree of narrowing of the artery;
- Pristress-ECHO. The technique allows you to determine transient disturbances in cardiac contractility in areas with altered blood flow.
Treatment of myocardial dystrophy with folk remedies
Alternative medicine can only be used as an addition to the main therapy in consultation with the treating doctor. Traditional medicine recommends herbal decoctions and tinctures. A decoction of cumin and hawthorn gives good results.
Below are simple folk remedies to combat cardiosclerosis.
- A mixture of sour cream, honey and fresh protein. Beat 2 fresh chicken whites with 1 teaspoon of honey and 2 teaspoons of sour cream. The resulting mass should be taken on an empty stomach.
- Healing collection. Pour 300 ml of boiling water over dry raw materials (1 teaspoon each of hawthorn, yarrow, mistletoe, periwinkle). Let it brew for 1 hour. Should be taken in small portions throughout the day.
- Elecampane root. Pour 300 g of dry raw material into 500 ml of vodka and keep in a dark place for a week. The filtered decoction should be taken three times a day, 30 ml.
- Lemon and pine. Peel the lemon and divide in half. Pour half a lemon with pine decoction. Let it brew. You need to take it for a week, then take a two-week break and repeat the course.
- Onion juice and honey. For myocardial diseases, drinking onion juice mixed with honey is beneficial. The mixture should be stored in the refrigerator.
Prices for treatment of post-infarction cardiosclerosis
Cost of services
| Description | price, rub. |
| Appointment with a cardiologist with the development and preparation of a treatment plan | 2100 rubles |
| ECG registration with additional leads | 500 rubles |
| Taking an ECG | 800 rubles |
| Taking an ECG with interpretation | 1500 rubles |
All services
All prices
Prevention
Prevention of the development of cardiosclerosis consists of timely treatment of the underlying trigger disease, which provokes the proliferation of connective tissue.
There are basic rules, the observance of which allows you to slow down the progression of cardiosclerosis and avoid the development of complications:
- Complete smoking cessation. When using tobacco, spasm of the coronary vessels is observed, which increases myocardial hypoxia;
- Limiting physical activity. Jerks, sudden lifting of weights, and physical overload are unacceptable. Moderate cardio exercises are encouraged, which keep the muscles toned, but do not overload the heart;
- Constant monitoring by a cardiologist. Regular visits to the doctor, even without deterioration in health, every 3 months will allow you to diagnose complications in a timely manner and promptly correct the treatment regimen;
- Timely treatment of hormonal disorders and acute infectious diseases. This measure will avoid the negative impact of concomitant pathology on the functioning of the heart;
- Avoid stress.
Ignoring these simple rules can lead to the development of complications, despite taking prescribed medications.
During pregnancy
When diagnosing certain dangerous conditions, pregnancy is called into question:
- myocarditis in the acute phase;
- severe coronary pathology;
- heart failure IIA;
- cardiosclerosis complicated by arrhythmia.
In such cases, in order to save the child, it is necessary to undergo a set of therapeutic measures that have a positive effect on the course of pregnancy. The first thing that needs to be done is the sanitation of foci of infection (pharyngitis, sore throat, caries). For this purpose, antibiotics are prescribed. Additionally, beta blockers, metabolic drugs and glucocorticosteroids are prescribed. Pregnant women with myocardial cardiosclerosis are under special supervision, because This category of patients has a high risk of developing complications from the cardiovascular system and kidneys.
Surgery
- Placement of an implantable pacemaker (ICS) - used when the conduction of impulses along the heart fibers is disrupted or the heart rate decreases.
- Coronary artery or mammary coronary artery bypass grafting.
- Surgeries on heart valves for heart failure caused by valvular defects.
- Heart transplantation.
Photo: https://pixabay.com/photos/hospital-operating-room-doctor-2767950/
Diet for cardiosclerosis
Diet for vascular atherosclerosis
- Efficacy: therapeutic effect after 2 months
- Dates: no data
- Cost of products: 1700-1800 rubles. in Week
Diet for heart failure
- Efficacy: therapeutic effect after 20 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Diet for cardiac arrhythmia
- Efficacy: therapeutic effect after 30 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Diet for coronary heart disease
- Efficacy: therapeutic effect after 30 days
- Timing: constantly
- Cost of products: 1700-1800 rubles. in Week
Diet after a heart attack
- Efficacy: therapeutic effect after 2-6 months
- Terms: 2-12 months
- Cost of products: 1800-1900 rubles. in Week
Diet for cardiosclerosis is important. The essence of dietary nutrition is to reduce cholesterol in the blood. Correction of the blood lipid profile helps prevent the development of atherosclerosis in the coronary vessels. Additionally, it is necessary to limit salt intake (up to 5 g per day, and in severe cases - up to 3 g). A salt-free diet can reduce the volume of circulating blood, reducing the load on the heart.
Prohibited foods for cardiosclerosis:
- animal fats (butter, fatty meat);
- smoked meats, pickles;
- chocolate;
- coffee and strong tea;
- flour products;
- alcoholic drinks, energy drinks.
The emphasis in nutrition should be on eating lean boiled meat, various cereals, fresh fruits and vegetables. It is better to give preference to foods rich in potassium. The effect of cardiac glycosides is better when there is sufficient potassium in the body.
It is useful to eat raisins, bananas, dried fruits. It is necessary to monitor the total daily caloric intake (1800-2600 kcal). A well-designed menu will cover all the body’s needs in conditions of limited physical activity. Calorie content can change by 20-30% only if the patient suffers from obesity or cachexia (exhaustion). Poor nutrition worsens the prognosis for the patient. A qualified nutritionist and attending physician will help create a specific menu for the patient.
What factors lead to the development of cardiosclerosis?
The causes of the disease can be both heart disease and non-cardiac pathology. Of these, the most common are:
- coronary heart disease, myocardial infarction;
- long-term arterial hypertension;
- hypertrophy of the heart chambers, most often the left ventricle;
- endocrine pathology: diabetes mellitus, thyroid diseases, etc.;
- alcohol abuse, malnutrition, low-protein diets.
Consequences and complications
It is important to understand that cardiosclerosis is an irreversible process, which in any case worsens the functioning of the heart and increases the risk of developing various complications. Even if the causes that worsen the course of the disease are eliminated, the presence of connective tissue in the thickness of the heart muscle can lead to adverse consequences. All complications are corrected with medication or treated surgically.
The most common consequences and complications:
- formation of CHF;
- development of cardiac aneurysm ;
- development of arrhythmias ;
- acquisition of heart defects;
- development of thromboembolism ;
- diagnosing chronic fatigue syndrome.
Forecast
The diffuse form of cardiosclerosis is considered unfavorable in its prognosis. For example, with the formation of connective tissue at the site of a transmural infarction, the risk of developing an aneurysm increases, the rupture of which most often leads to immediate death. In cases where cardiosclerosis arose as a result of natural age-related changes, this course of the disease is usually favorable.
Cardiosclerosis is a common heart pathology, the severity of which depends on the volume of affected tissue and the general condition of the body. If a person notices symptoms of this disease, he should consult a doctor as soon as possible, who will examine him and prescribe therapy.
Prognosis for cardiosclerosis
The prognosis is assessed after a thorough examination of the patient. If the patient has no pronounced complaints, and the disease is amenable to drug therapy, then the prognosis is considered favorable. Most often, positive dynamics are observed with small focal cardiosclerosis.
In patients with large-focal lesions, as well as with diffuse proliferation of connective tissue, the prognosis is considered unfavorable. After a transmural infarction, an aneurysm forms in the affected area, which entails very serious complications and consequences. Often, after large-focal infarctions, arrhythmias , which are also considered prognostically unfavorable.
The prognosis for survival in post-infarction cardiosclerosis depends on the area of the lesion, treatment regimen, concomitant pathology, age, and the presence of complications.
Expert advice
Changing your lifestyle is a difficult problem, especially psychologically. Not every person is able to leave their comfort zone. That's why I give talks or refer patients to health schools. During communication, patients become familiar with the formidable complications and make a choice for themselves: to live a long and happy life, or to die from vascular accidents over the next few years.
Drug therapy
Taking medications is aimed at eliminating and preventing various pathologies of the heart and blood vessels (hypertension, rhythm disturbances, edema, etc.).
For arterial hypertension the following are indicated:
- Beta blockers (Metoprolol, Betalok ZOK, Nebilong). They effectively reduce blood pressure and are a measure to prevent arrhythmias with high heart rate.
- Diuretics (Furosemide, Hydrochlorothiazide, Veroshiron, Lasix). They lower blood pressure by removing excess fluid from the body and help eliminate edema.
- Calcium channel blockers (Amlodipine, Nifedepine, Diltiazem) - prevent the occurrence of heart rhythm disturbances and significantly reduce the total peripheral resistance of the vascular walls.
- Angiotensin 2 receptor antagonists and angiotensin-converting enzyme inhibitors (Valsartan, Captopril, Enalapril). Reduce afterload on the heart by reducing vascular tone.
Selection of antihypertensive drugs taking into account the spectrum of vascular pathologies is an extremely difficult task for any clinician. Often, the pressure stabilizes only after several treatment adjustments. Based on personal experience, combinations such as “Betaloc” (b-blocker) and “Diroton” (ACE inhibitor) were tested in patients with stage 2-3 hypertension and atrial fibrillation or “Hydrochlorothiazide” with “Enalapril” in patients whose condition is accompanied by edema syndrome.
Patients are often prescribed antihypoxants (Preductal) and anticoagulants (Xarelto) to improve brain function and prevent vascular accidents.
In case of systemic pathologies of connective tissue, cardiosclerosis should be treated by an immunologist, occupational pathologist and other specialized specialists. The presence of myocarditis is a reason to prescribe rational antibiotic therapy and temporary use of cardiac glycosides. Frequent attacks of angina pectoris require the use of nitrates (Nitroglycerin, Nitrospray).
Surgery
In case of obstruction of the coronary bed, which cannot be compensated with medication, balloon dilatation of blood vessels and coronary artery bypass grafting are performed. The presence of aneurysms is a reason for their surgical excision. In case of arrhythmias and blockades on the part of the conduction system, pacemakers and cardioverters are installed, which in case of a critical violation will save lives.
List of sources
- Shopin A.N. Prediction of recurrent myocardial infarction in patients with post-infarction cardiosclerosis / A.N. Shopin, Ya.B. Khovaeva, E.N. Burdina, B.V. and others // Practical medicine, 2011
- Samorodskaya I.V. Cardiovascular morbidity and risk factors for cardiovascular events in the Russian Federation / I.V. Samorodskaya // Cardiovascular therapy and prevention, 2005. No. 3
- Tokareva E.A., Khatuntseva Yu.A., Makeeva A.V. ETIOLOGY, PATHOGENESIS AND DYNAMICS OF THE INCIDENCE OF CARDIOSCLEROSIS IN THE VORONEZH REGION // International Student Scientific Bulletin. – 2016
Diagnosis of atherosclerosis of the aorta of the heart
As a rule, it is almost impossible to suspect the development of atherosclerosis of the aorta of the heart only based on the patient’s complaints, which is why regular examination by a therapist and identification of associated risk factors is so important. These include increased blood pressure, increased body weight, and increased cholesterol levels in the blood.
If there is a suspicion of the presence of atherosclerosis of the aorta, the following clarifying methods are used:
- ECG supplemented by ultrasound results of the aorta and heart;
- Coronography and angiography;
- Duplex and triplex scanning;
- MRI.