Doctors around the world are constantly fighting against skin diseases. Dermatitis is allocated to a special group. This is a difficult-to-treat disease that develops as a result of inflammation or allergies. The reasons may be chemical, mechanical or biological.
The professional name for the disease is allergic dermatosis. This heterogeneous group includes urticaria, eczema, toxicerma, and other varieties.
Description of the disease
Atopic dermatitis is a pathology characterized by chronic immune inflammation of the skin.
According to statistics, approximately every 4th child in the world suffers from atopic dermatitis. In Russia, approximately 15% of children have typical symptoms of the disease, which tend to subside as they grow older. According to research, about a third of patients who notice clinical signs in childhood feel satisfactory in adulthood if treatment was started on time. Girls are 1.6 times more likely to suffer from atopic dermatitis. The disease is of a pronounced allergic nature. The connection between atopic dermatitis and other manifestations of immune dysfunction, which include bronchial asthma, various forms of allergic rhinitis, conjunctivitis, and food allergies, has been proven.
A generally accepted international classification of atopic dermatitis has not yet been developed. In practice, doctors use the working classification proposed by domestic experts in the field of allergology.
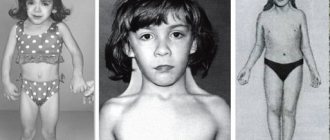
Depending on the age of the child, the following forms of atopic dermatitis are distinguished:
- infant (up to 2 years);
- children's (up to 12 years);
- teenage (after 12 years).
Taking into account the possible causes of the disease, atopic dermatitis can be:
- with increased sensitivity to food (food sensitization);
- with sensitivity to fungi (fungal sensitization);
- with tick-borne or household sensitization;
- with sensitivity to pollen.
The severity of the disease can be mild, moderate and severe. In the process of disease development, the stage of exacerbation, incomplete and complete remission is distinguished. Despite the availability of a large number of medications, achieving complete remission can be difficult. This is due to a chronic inflammatory process inside the skin, which has a genetic predisposition. However, timely treatment helps to avoid other dysfunctions of the immune system.
Prevalence
The prevalence of AD among developed countries is 10-20%. The manifestation of AD symptoms in children is observed at the age of 6 months in 60% of cases, up to 1 year in 75%, and up to 7 years in 80-90%. Over the past decades, there has been a significant increase in the incidence of AD, its course is becoming more complicated, and its outcome is aggravated. In the 20th century, the connection between AD, hay fever and bronchial asthma was confirmed, which was designated the term “atopic triad”.
The combination of AD with bronchial asthma is observed in 34% of cases, with allergic rhinitis - in 25%, with hay fever - in 8%. AD may be the debut of the “allergic march”, when in the future such patients develop other atopic diseases: food allergies, bronchial asthma, allergic rhinitis. AD associated with food allergies accelerates the progression of the “allergic march.”
Symptoms of atopic dermatitis in children
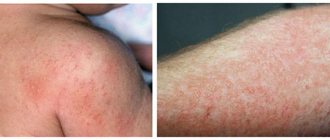
The clinical picture of atopic dermatitis is due to the formation of a large number of foci of inflammation in different areas of the skin. In this regard, the main manifestation of the disease is itching, which interferes with sleep, worsens general well-being, and leads to constant irritability of the child. Rashes form at the site of local inflammation. They may have different appearance depending on the stage of the disease:
- In the acute phase, the elements are bright red. Due to the influx of additional blood into the area of inflammation, local swelling is formed. Scales and plaques may be present. On palpation, the skin elements are moist.
- In the phase of incomplete remission, the rash is flesh-colored, dry, and may peel. The appearance of new elements is often caused by friction of the skin against clothing.
The location of skin rashes differs depending on the age of the child.
In infants, they most often occur in the head (the scalp), neck and chest. The favorite place for new rashes is the extensor surfaces of the joints. In adolescence, the “geography” of rashes moves to the back, abdomen, and groin.
Constant itching disrupts sleep, the child becomes capricious and labile. In adolescence, edematous rashes that change the aesthetics of the skin become the cause of psychological complexes. Skin elements in areas of friction can become infected with the formation of local abscesses. This is accompanied by an increase in body temperature, general weakness of the child, and a deterioration in general well-being.
Important Tips
In order for the child to suffer less due to dietary restrictions and unpleasant symptoms of the disease at the time of treatment, parents must create the most favorable and comfortable conditions for the baby at home.
Here are some valuable tips:
- All fabrics that come into contact with the baby's skin must be absolutely hypoallergenic. It is better to completely abandon synthetic underwear and textiles.
- A child's sleep should be sound and healthy. It is worth buying an orthopedic mattress and pillows. Orthopedic accessories correspond to the anatomical features of the child’s body and will allow the baby to sleep better, even if itching and pain prevent this.
- You can bathe your baby, but use decoctions of medicinal herbs (chamomile, calendula, oak bark, string) instead of regular water.
- Do not rub irritated skin with a towel, or wear clothes that are too tight and uncomfortable, which can cause additional irritation of the skin (sometimes it is poor-quality clothing that provokes the development of allergic rashes).
If a small patient suffering from allergic dermatitis is provided with proper care, coping with the disease will be much easier. This applies to both tired parents and the exhausted baby.
Causes of atopic dermatitis in children
Atopic dermatitis is a complex multifactorial disease. Several processes simultaneously play a key role in the pathogenesis of the disease:
- Immune inflammation against the background of activation of the Th2 cell population. Normally, they are in “combat” mode sporadically – only when exposed to provoking factors. In atopic dermatitis, these cells almost constantly maintain increased activity, which leads to chronic inflammation of the skin.
- Genetic damage accompanied by disruption of skin keratinization processes. This means that due to congenital gene defects, the synthesis of proteins that are responsible for creating the mechanical barrier of the skin is impaired. Under such conditions, the dermis becomes more susceptible to the penetration of bacteria, viruses and the negative influence of physical factors.
- Hyperactivity of mast cells. Tissue basophils are “containers” for histamine and other pro-inflammatory substances. When they are released, which is observed in particular with atopic dermatitis, the child feels severe itching.
It has been proven that atopic dermatitis is a genetically determined disease.
If one of the parents suffers from a similar pathology, the chance of its manifestation in the child reaches 30-40%. If both mother and father have the disease, the baby’s risk increases to 70-75%. Due to the fact that the disease is more common among city residents, scientists have identified additional provoking factors:
- the saturation of products with synthetic elements (antibiotics, flavor enhancers, preservatives);
- air pollution;
- excessive sun exposure;
- excessive use of children's cosmetics.
Triggers for the appearance of new rashes can be food allergens, mold, pet hair, and too strong emotional experiences.
In modern society, atopic dermatitis is an increasingly common problem. Therefore, it is important for parents to identify suspicious symptoms in their child in time in order to begin comprehensive treatment.
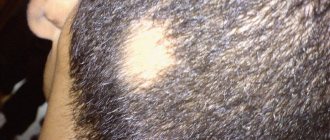
What complications can there be?
One of the most common complications of AD is skin infections. This is due to reduced immunity, which is common to almost all people suffering from dermatitis. The most common causes are pyoderma, herpes, eczema, and in severe cases, sepsis. The causative agent is both fungi and bacteria.
In childhood, a fungus of the genus Candida is most often detected, and in adults (after 20 years) the fungal infection is caused by Trichophyton rubrum.
Kaposi's eczema herpetiformis and sepsis are the most severe complications that can cause serious deterioration in health, including death.
Long-term exacerbation of atopic dermatitis often leads to neurosis. This leads to decreased activity, isolation, and aggression. Against the background of constant itching, the patient experiences other health problems - pressure surges, tachycardia, insomnia.
Diagnosis of atopic dermatitis in children
There are no specific diagnostic methods that would clearly indicate the presence of atopic dermatitis. The diagnosis is based on a comprehensive assessment of the child’s condition and consists of the following key points:
- Analysis of patient complaints. The allergist examines the affected areas of the skin, conducts dynamic monitoring of changes in pathological elements in the acute and chronic phases of the disease.
- Collection of allergy history. The doctor works not only with the child, but also with the parents.
- Conducting allergy tests. Helps identify the possible cause of the disease.
- Laboratory tests. The child is prescribed a general and biochemical blood test. The allergist is interested in the number of eosinophils, markers of the inflammatory process and the functioning of other organs and systems.
An important role in making a diagnosis is played by the combination of atopic dermatitis with other diseases of an allergic nature.
Skin problems are often present in children suffering from bronchial asthma. Instrumental diagnostics for children with atopic dermatitis is not included in the standard examination. The exception is cases of damage to internal organs.
What it is?
Atopic dermatitis is a chronic inflammatory disease of an allergic nature, the main symptoms of which are a rash on the skin of the exudative and/or lichenoid type, severe itching and seasonality.
Atopy is a genetic predisposition to produce excess immunoglobulin E in response to contact with environmental allergens. The term "atopy" comes from a Greek word meaning foreign. Manifestations of atopy are various allergic diseases and their combinations. The term “allergy” is often used as a synonym for allergic diseases, the mediator of which is immunoglobulin E, but in some patients with these diseases the levels of this immunoglobulin are normal, and then a variant of the course of the disease not mediated by immunoglobulin E is identified.
Treatment of atopic dermatitis in children
Treatment of atopic dermatitis in children should be comprehensive. The main goals of the therapy are:
- minimizing the child’s contact with agents that provoke inflammation;
- hypoallergenic diet;
- local and systemic drug therapy;
- teaching the child and parents the correct lifestyle that will help avoid relapse of the disease;
- therapy of concomitant diseases.
During treatment, the allergist tries not only to eliminate the symptoms, but also to prevent repeated episodes of the disease. This helps improve the quality of life of the child and parents, and prevents the likelihood of complications. Children with atopic dermatitis may be prescribed the following groups of medications:
- local and/or systemic glucocorticosteroids;
- antihistamines;
- antibiotics and antifungal drugs.
If obvious triggers for the appearance of new rashes are identified, the child should be taught to avoid them.
It is recommended to switch to a hypoallergenic diet. It is developed individually for each patient. If the effectiveness of classical methods is low, phototherapy, psychotherapy, and visits to resorts may be prescribed.
Typical localizations
There are 5 clinical forms of manifestation that classify dermatitis according to groups of the most pronounced symptoms and their typical locations.
- Erythematous-squamous. Typical for infants. The process begins on the cheeks, covering the entire face, concentrating on the area around the mouth and eyes. The skin of the head and neck and hands are often affected. The disease manifests itself as bright red spots, which are swollen tissue, then becomes covered with an itchy rash, in the form of papules, vesicles, which are replaced by erosions. After the severity of the process subsides, dry areas with loose flakes of dead skin appear on the affected areas. Seizures can form on the lips, which spread to the lip area in the form of areas of erythema, turning into infiltration and then into flaky areas. Often a secondary infection develops in the form of pustular skin lesions
- Vesicular-crustic (exudative) is characteristic of early childhood dermatitis, affecting children aged 3-5 months. It begins with erythemal areas, later vesicles are added, which, after opening, form weeping areas with microerosions - the so-called serous wells. The form is characterized by severe itching. The cheeks, flexor surfaces, chest, hands, and feet suffer.
- Erythematous-squamous with lichenification is typical for older children and adults. Characterized by areas of inflamed skin. Rashes of a papular nature (small, spherical) turn into flaky skin. Lesions often appear symmetrically, covering the elbow and popliteal folds, the back of the hands, and the lateral and posterior areas of the neck.
- The lichenoid form is characteristic of adolescents. The affected areas appear as foci of inflamed, thickened, swollen skin with a pronounced pattern. Rashes are large, merging formations with liquid inside, covered with scaly skin. This form is characterized by the symptom of polished nails (the patient has shiny nails with worn edges). The scratched areas may become covered with abrasions and bruises. A bacterial infection may occur.
- The prurigo-like form affects adults. It is characterized by a protracted course, rashes in the form of papules. Localization – face, popliteal and elbow bends, buttocks. The skin is thickened. Due to severe itching, the skin is constantly scratched. At the site of scratching, areas of atrophied skin can be seen.
| The most common sites of localization of rashes during the disease |
Questions
- Which doctor treats atopic dermatitis in children?
An allergist is involved in identifying and treating atopic dermatitis in children. - Can atopic dermatitis be cured?
Due to the chronic nature of the disease, it is almost impossible to completely get rid of atopic dermatitis. However, if you follow all the doctor’s recommendations and carry out high-quality treatment, you can achieve stable remission. Many patients, after targeted therapy, forget about their skin problems for years. - Is it possible to influence the risk of developing atopic dermatitis in a child if the parents suffer from this pathology?
To date, there is no effective mechanism for targeting a child’s genetics. Therefore, it is impossible to predict in advance whether a child will have atopic dermatitis. These children are recommended to undergo preventive monitoring by an allergist. - When should you contact a specialist?
You should consult an allergist when the first skin rashes appear that itch and bother your child. This will allow you to establish a correct diagnosis in time, begin targeted treatment and reduce the risk of complications.
Disease prevention
Primary preventive measures that are aimed at preventing the disease include:
- Maintaining a healthy lifestyle during pregnancy. Even passive smoking can have a detrimental effect on fetal development.
- A varied diet for the expectant mother.
- Use medications only as prescribed by a doctor, if necessary.
- To develop sufficient immunity in a baby, it is recommended to breastfeed for at least 6 months.
- Do not include potentially allergenic foods in complementary foods without consulting a pediatrician.
- If you have a family history, use emollients (fat-based cosmetics) for preventive purposes.
Secondary prevention is carried out with the aim of prolonging the period of remission of the disease and, if possible, preventing exacerbation. To do this, special attention must be paid to protecting and moisturizing the skin. Recommendations for secondary prevention:
- Control of humidity and air temperature in the room. This is especially important in winter when the heating devices are turned on.
- Clothes should be chosen only from natural fabrics. These are linen, cotton, flannel. A patient with atopic dermatitis should not have synthetic items in his wardrobe; wool should also be minimized. A loose fit is desirable, as contact of the material with inflamed skin can lead to infection.
- When washing things, use hypoallergenic products, preferably in liquid form. Eliminate air conditioners.
- Keep your nails long and clean. Women prefer to have a short manicure without decorative coating.
- Avoid tobacco smoke and harmful industrial fumes.
- You can sunbathe, but without fanaticism. Ultraviolet light has a beneficial effect for dermatitis, so sanatorium-resort treatment is indicated for such patients. However, being in the sun during high activity hours (from 12 to 17 hours) is not recommended. Sunscreens should only be used after approval by a dermatologist.
As for playing sports, increased sweating can lead to a worsening of the condition. In this case, preference should be given to less active sports. Participation in outdoor games is not recommended, as there is a risk of injury or damage to the skin, as well as contact of clothing with skin. When visiting the pool, be sure to take a shower before and after swimming, and also use protective moisturizing lotions or creams. You should give preference to non-chlorinated water - many modern swimming pools use non-chemical methods of water disinfection.
Atopic dermatitis is a psychosomatic disease, which means that a person’s emotional state plays an important role in its occurrence. Try to avoid stress, relax more often and pamper yourself. This will help reduce the manifestations of the disease in the acute period, as well as prolong the period of remission.