Consultation with a gastroenterologist – 1,750 rubles.
- Causes
- Symptoms
- Diagnostics
- Treatment
- Prevention
Celiac disease (gluten enteropathy, intestinal infantilism, G-Herter-Heubner disease) is a pathological disorder of the intestines in which gluten intolerance is observed. This protein is found in cereals. As a rule, symptoms manifest themselves most clearly in childhood; over time, signs of the disorder become less pronounced. In women, the disorder is diagnosed more often.
Celiac disease is common throughout the world. According to the World Association of Gastroenterology, the incidence of celiac enteropathy in different populations ranges from 1:100 to 1:300. In Russia, the estimated incidence of celiac disease is 1:1000 Source: Bai J. WGO-OMGE / J. Bai, E. Zeballos, M. Fried // Practice Guideline Celiac Disease. - 2005. - Vol. 10. - P. 1-8. .
Undiagnosed celiac disease can lead to serious consequences, such as: malignant diseases of the gastrointestinal tract, in particular small intestinal lymphoma, unexplained infertility, osteoporosis, growth impairment, autoimmune diseases that occur 10 times more often in adult patients with celiac disease Source: Kamalova A.A. Evolution of approaches to the diagnosis and treatment of celiac disease / A.A. Kamalova, M.O. Pirogova // Bulletin of modern clinical medicine. - 2013. - T.6. — Vol. 3. - pp. 40-48. . The mortality rate among patients with untreated celiac enteropathy is 10-30%, while with adequate treatment - a strict gluten-free diet - it drops to 0.4% Source: Mikhalik D.S. Celiac disease: disease and lifestyle / D.S. Mikhalik [and others] // Zemsky doctor. - 2012. - No. 4. - P. 35-38. .
Etiology
The leading role is played by gliadin - the alcohol-soluble fraction of gluten
- squirrel. Gluten is a water-insoluble complex of proteins (prolamins, glutenins) with a low content of lipids, sugars and minerals. Prolamins that are toxic to patients with celiac disease are: wheat gliadin; rye secalin; barley hordenine; Ovein does not cause atrophy of the mucous membrane of the small intestine and an increase in autoantibodies, but contamination of oat products with other grains cannot be ruled out, so it is also not recommended for use in celiac disease.
What is gluten
From Latin gluten
translated as
glue
.
In Russian, this substance is usually called gluten
. The concept combines several proteins from different cereals: wheat - gliadin, rye - secalin, barley - hordenin. It is these proteins that form the sticky network that makes the dough so viscous and elastic.
Gluten, according to the FSA (Food Standards Agency), is included in the list of allergens that the manufacturer is required to indicate on product packaging
Pathogenesis
There is no doubt that celiac disease does not occur without gluten, but there are still no clear opinions about its pathogenesis, so there are a number of hypotheses.
1) Sensitization with gliadin,
as a result, the intestinal epithelium becomes a target for the development of the immunological process. Once in the mucous membrane, the protein antigen (gluten) undergoes cleavage in the macrophage lysosomes into peptides. Peptides bind to HLA class II molecules located in the endoplasmic reticulum of the same cell. In this case, the peptides undergo deamination in the presence of the tissue transglutaminase enzyme – TG2, which ensures closer binding of gluten peptide residues to the DQ2 and DQ8 molecules. This complex is presented on the macrophage membrane and is recognized by lymphocytes that have passed through Peyer's patches. Activated T-lymphocytes turn into cytotoxic cells carrying CD8 markers (killer cells) and helpers (Th1 and Th2), which are CD4-positive. At the same time, the content of CD4 lymphocytes in the lamina propria of the mucous membrane increases almost 50 times, and CD8 T cells in the epithelium - almost 10 times. Th1 produces IL-2, tumor necrosis factor (TNF) and interferon-γ, which induce inflammation and activate a cytotoxic immune response; Th2 – a significant amount of IL-4, 5 and 10, inhibiting Th1 activity. In turn, TNF activates metalloproteases, in particular MMP-3 and MMP-1, disrupting the structure of the subepithelial region of the mucosa and destroying collagen. B lymphocytes potentiate the production of antibodies to gluten and tissue transglutaminase. In parallel, the production of autoantibodies to TG2 occurs, which in the form of IgA deposits are located in the subepithelial layer of the intestine, on fibroblasts, as well as in the liver, lymph nodes, muscles, and blood vessels. Blocking tissue transglutaminase by autoantibodies leads to destruction of the epithelium and mucosa, villous atrophy and proliferation of crypt epithelial cells, which increases the permeability of the mucosa, including gluten.
2) The role of viruses
in the pathogenesis of celiac disease (in some patients, an increase in antibody titers to adenovirus type 12 is detected in the blood, a decrease in which was noted when the patients’ condition improved on the background of the agliadine diet).
In celiac disease, there is an autosomal dominant type of inheritance with incomplete penetrance. In the patient's closest relatives, the incidence of the disease varies from 2 to 12% according to histological examination of the mucous membrane of the small intestine. In identical twins, concordance for celiac disease is approximately 70%, and in HLA-identical individuals it is up to 30%. Parents of patients with celiac disease themselves suffer from latent celiac disease in approximately 14% of cases.
ESPGHAN 2012 Diagnostic Criteria for Celiac Disease
The first criteria for diagnosing celiac disease were developed by experts from the European Society of Pediatric Gastroenterology and Nutrition in 1979 and were based on repeated biopsies of the small intestine.
The development of immunological diagnostic methods has made it possible to significantly improve the criteria and recommend a serological test for selecting patients for endoscopic examination. In the 1990 criteria, the number of endoscopies was reduced to one.
At the same time, with all its undeniable advantages, an endoscopic examination followed by a biopsy of the wall of the small intestine in a child is associated with physical and psychological trauma. In addition, biopsy is not without methodological errors. First of all, this is due to the difficulty of orienting small pieces of biopsy material when preparing histological sections. Biopsy orientation may lead to false assessment of villous height and other incorrect findings.
ESPGHAN experts (2012 criteria) clearly defined the list of people who need to be examined to identify celiac disease.
Celiac disease should be suspected in children and adolescents who have unexplained symptoms including:
- chronic or intermittent diarrhea;
- delayed growth and development, weight loss, delayed puberty, amenorrhea, iron deficiency anemia, chronic weakness, fracture due to minor trauma/osteopenia/osteoporosis;
- diarrhea and vomiting, chronic abdominal pain, bloating and cramps, chronic constipation, and elevated liver enzymes;
- reductive aphthous stomatitis, dermatitis herpetiformis.
Symptoms of celiac disease
Clinical manifestations and symptoms of celiac disease are as follows.
Celiac disease manifests itself after the introduction of gliadin-containing products (formulas, complementary foods) into children's diets.
After 2-3 months, the first signs of the disease appear. The onset of the disease may also be late - 5-6 months or more after the first introduction of gluten into the diet, sometimes after an infectious disease (intestinal infection, ARVI), and often for no apparent reason. The most common clinical manifestations of the disease
: 1) persistent decrease in weight and height indicators, 2) vomiting from rare to daily 3) diarrhea (malabsorption syndrome, stools are frequent, mushy, abundant with a grayish tint) 4) abdominal pain syndrome, 5) increase in abdominal circumference, 6) edema syndrome (decrease in blood protein levels), 7) development of food allergies (more often - intolerance to cow's milk proteins), delayed psychomotor development (loss of acquired skills), 9) polyhypovitaminosis (development of signs of rickets, osteoporosis), 10) development of lactase insufficiency.
delayed psychomotor development (loss of acquired skills), 9) polyhypovitaminosis (development of signs of rickets, osteoporosis), 10) development of lactase insufficiency.
Why does a gluten allergy occur?
Allergies are just one of the “bad” reactions to gluten. In addition to it, true intolerance and simply sensitivity are distinguished.
- Celiac disease
is a true intolerance. An autoimmune disease that affects many organs at once. It is chronic and occurs if there is a genetic intolerance to gluten. - Gluten allergy
is a reversible reaction of the immune system to gluten proteins without a genetic predisposition. In particular, a reaction to wheat occurs in 60% of children and often disappears by age 12. How it manifests itself: nasal congestion, sneezing, redness of the skin, runny nose, difficulty breathing, diarrhea. - Non-celiac gluten sensitivity (NCGS)
is a non-allergic and non-genetic reaction to gluten. However, it can cause typical signs of gluten intolerance. There are symptoms, but there is no diagnosis of a genetic disease or allergy - which means it is NCCH.
Classification of celiac disease in children
(St. Petersburg, May 2010)
Shapes:
- Typical
- Atypical (asymptomatic)
Periods:
- Latent (from the introduction of gluten to the appearance of clinical manifestations - 1.5-2 months)
- Active (clinical manifestation)
- Remission (clinical, clinical-serological, morphological); initial remission (up to 3 months of diet), incomplete remission (3-12 months of diet)
Severity
(determined by the presence and number of deficiency conditions and complications:
- Mild – deficiency conditions of the 1st degree (protein-energy deficiency of the 1st degree, anemia of the 1st degree, osteopenia, iodine deficiency goiter of the 1st degree, dysbiosis of the 1st degree), height 25-5 percentile
- Moderate – deficiency conditions of the 2nd degree (protein-energy deficiency of the 2nd degree, anemia of the 2nd degree, osteoporosis, iodine deficiency goiter of the 2nd degree, dysbiosis of the 2nd-3rd degree), growth less than the 5th percentile
- Severe – deficiency conditions of degree 3 or more, complications
An example of a diagnosis:
- Celiac disease, typical form, period of incomplete remission, moderate severity. Diagnosed at age 10. Gluten-free diet with disorders for 1 year. Genetic diagnosis: HLA – DQА1*501*501HLA – DQВ1*303*301. Atopic dermatitis, common, moderate course (polyvalent food allergy).
Diagnostics
Stages of primary diagnostic examination (
when verifying the diagnosis before prescribing a gluten-free diet):
- clinical and anamnestic stage,
- serological
- histological
- genetic (if necessary).
Stages of diagnosis of the disease period
(against the background of a gluten-free diet during dispensary observation):
1) clinical and anamnestic,
2) serological (not earlier than 3 months from the prescription of the diet),
3) histological (not earlier than 1 year from the prescription of the diet, provided there is no increase in AGA and Anti-TSH).
Stages of diagnosis in genetic risk groups
(1st degree relatives):
1) genetic stage,
2) clinical and anamnestic,
3) serological,
4) histological.
Research methods
To mandatory laboratory research methods
for celiac disease include (in a hospital setting):
- clinical blood test - repeat once every 10 days;
- general urine analysis;
- fat microscopy of stool (scatology);
- bacteriological examination of stool;
- histological examination of the biopsy;
- serum immunoglobulins (Ig A, Ig G, Ig M);
- total protein and protein fractions, albumin, cholesterol, total lipids, triglycerides, glucose, bilirubin, AST, ALT, calcium, phosphorus, serum iron, zinc, potassium, sodium, chlorides;
- Gluten-sensitive enteropathy tests - GSE (Gluten-sensitive enteropathy):
antigliadin antibodies (AGA, AGA) IgA – AGA, IgG – AGA;
endomysial antibodies (EMA, EMA) IgA – EMA, IgG – EMA;
tissue transglutaminase antibodies (tTG, tTG) IgA - tTG, IgG - tTG);
anti-reticulin antibodies (ARA);
Anti-actin antibodies (AAA).
Additional laboratory tests:
- elastase-1 feces;
- determination of bone age and bone density;
- genetic analysis – HLA-DQ2 (DQA1*0501, DQB1*0201) HLA-DQ8 (DQA1*0301, DQB1*0302);
- stool lipid profile;
- excretion of plasma protein in feces;
- determination of antibody titer to food antigens (for young children!);
- stress test with D-xylose and gluten;
- cortisol, TSH, T3, T4, STH.
Mandatory instrumental research methods:
- anthropometry (weight, height, head circumference, chest, abdomen);
- Ultrasound of the liver, biliary tract and pancreas;
- EGD with targeted biopsy of the mucous membrane from the distal duodenum or the initial part of the jejunum (no later than 2-3 months from the start of a gluten-free diet).
Additional instrumental research methods:
- detection of antibodies to glutenin and deamidated gliadin; instant test for tissue transglutaminase (TSG) using test strips;
- CD Medics chip system – determination of several types of AT, Ig A, HLA DQ2/DQ8 status.
Mandatory consultations with specialists
: geneticist.
Additional specialist consultations
: allergist, endocrinologist, orthopedist, dentist.
Nuances of serological diagnosis of celiac disease
1) Antigliadin antibodies
(AGA, AGA) IgA - AGA, IgG - AGA. Currently not recommended for the diagnosis of celiac disease in adults and used only for the diagnosis of celiac disease in children under two years of age due to insufficient maturation of the components of the complement system responsible for the production of autoantibodies (12%).
2) Tissue transglutaminase antibodies
(tTG, tTG) IgA – tTG, IgG – tTG). They are not specific enough and, in addition to diagnostic markers of celiac disease, can be used as indicators of the activity of inflammatory processes and destruction in other inflammatory bowel diseases.
The main microscopic signs of celiac disease:
atrophy and decrease in the height of the villous epithelium, deepening of the crypts, an increase in the number of interepithelial lymphocytes over 30-40 per 100 epithelial cells, pronounced plasmacytic infiltration of the stroma of the mucous membrane. Most studies for celiac disease recommend taking 4 pieces of mucosa: 2 from the proximal part, 2 from the distal part.
Problems in the histological diagnosis of celiac disease:
unsuccessful sampling of material, incorrect orientation of the biopsy, lack of clinical information, Brunner's glands in the mucous membrane.
In three situations, the histological picture is almost impossible to distinguish from celiac disease:
autoimmune enteritis; exposure to medications, especially non-steroidal anti-inflammatory drugs; Helicobacter gastritis.
N.B !
The initial examination for diagnosis should be carried out during the active period of the disease before prescribing a gluten-free diet!
The final diagnosis is established on the basis of two mandatory signs :
a) characteristic clinical manifestations and anamnesis data
b) specific morphological data of the upper mucous membrane of the small intestine (“gold standard of diagnosis”)
and one of
research
methods :
a) serological examination,
b) HLA – typing.
Diagnosis
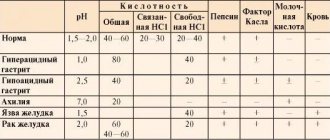
The diagnosis is made on the basis of the clinical picture, X-ray and biochemical studies. One of the characteristic diagnostic signs is the development of disease symptoms after eating foods containing gliadin. An X-ray examination reveals uneven expansion of the loops of the small intestine, alternating areas of spasm with areas of atony; When conducting a study on an empty stomach, multiple horizontal fluid levels, a change or complete absence of relief, and uneven, often accelerated, passage of barium suspension through the small intestine are determined.
A biochemical blood test reveals extremely low levels of total lipids, unesterified and unsaturated polyester acids, cholesterol, a large amount of free fatty acids in the feces, and the presence of plasma proteins in the intestinal contents, detected using immunoelectrophoresis (see) and immunoprecipitation (see Precipitation) of filtrates stool in agar with normal human antiserum.
A gliadin load test is also used to detect celiac disease. To do this, a small amount of flour is mixed with a large amount of water, then the excess water is removed, and ethyl alcohol is added to the dough. The alcohol extract contains gliadin, and insoluble glutenin remains in the sediment. The extract is evaporated, and the gliadin obtained in this way is given to the child orally at the rate of 300-350 mg/kg, preferably with sugar mixed with milk or kefir. After 3-5 hours, the content of gliadin in the blood plasma is determined using chromatography. In healthy children, the content of gliadin after exercise increases by no more than 40% from the initial level, in case of celiac disease - by more than 100%.
To diagnose the disease and assess the absorption function of the small intestine, as well as to assess the effectiveness of treatment, a test with a load of D-xylose is used. D-xylose (see Xylose) is highly soluble in water, actively absorbed in the small intestine, up to 40% of it is excreted unchanged in the urine, most of it within 5 hours. By the amount of D-xylose excreted, one can judge its absorption in the small intestine and the severity of the process. The highest content of D-xylose in urine is observed after 60 minutes. after load. In healthy children, this value is 30-35% of the administered amount, with celiac disease - on average 20%. When conducting a test for young children, D-xylose is prescribed at a dose of 0.3 g per 1 kg of body weight (mass). With a body weight of 17 kg and above, the load of D-xylose is 5 g. Determination of D-xylose in urine is carried out according to the method of Roe and Rice (J. H. Roe, EW Rice, 1948). The method is based on the transformation of D-xylose when treated with glacial acetic acid into furfural, which gives a red color with parabromo-aniline in the presence of thiourea, the intensity of which is proportional to the content of D-xylose in the urine.
Differential diagnosis
carried out with cystic fibrosis (see), primary exudative enteropathy (see Exudative enteropathy), disaccharide intolerance (see Malabsorption syndrome), with Hirschsprung's disease (see Megacolon), tuberculosis of mesenteric lymph nodes (see Extrapulmonary tuberculosis). It is based on data from a multilateral study and includes the determination of sodium and chlorine in sweat fluid and nail plates, as well as the severity of steatorrhea (to exclude cystic fibrosis), scatological examination and identification of serum and fecal proteins (to exclude exudative enteropathy), various stress tests , with the help of which disaccharide intolerance is detected, X-ray and histological examination of the intestine (when differentiating from Hirschsprung's disease), tuberculin diagnostics (to exclude tuberculosis), etc. Improvement in the child's condition when prescribing an agliadine diet is of great importance for differential diagnosis.
Celiac disease treatment
And now about the treatment of celiac disease.
Key points in the treatment of patients with celiac disease:
1) Consultation with a skilled dietitian.
2) Education about the disease.
3) Lifelong adherence to a gluten-free diet.
4) Diagnosis and treatment of nutritional deficiencies.
5) Access to an advocacy group.
6) Continuous long-term followup by a multidisciplinary team.
Prevention
Prevention of exacerbations of ciliacia is the exclusion of foods containing gluten from the diet, proper diet, and avoidance of stressful situations.
For relatives of the patient and people at risk (with diabetes, autoimmune thyroiditis, lymphocytic colitis, irritable bowel syndrome), it is advisable to conduct genetic analysis for early detection of the disease and prevent complications. When planning pregnancy, patients with celiac disease are recommended to consult a genetic specialist.
Malabsorption syndrome: symptoms and treatment Intestinal dysbiosis Irritable bowel syndrome Intestinal cancer Intestinal colitis Increased gas formation in the intestines
Celiac disease: diet
Gluten-free products
Currently not recognized as gluten-free by
products with a gluten content level of 200 ppm (mg/kg) for products from which gluten is removed during production - based on wheat starch (the so-called “Scandinavian standard”).
The ADA and the National Food Authority (USA) gluten-free
products in which
gluten is absent
, i.e., not determined by modern methods, the sensitivity threshold of which is 1.5 mg/kg, and products containing <200 ppm are called
“low-gluten products.” gluten content"
Gluten containing products
Let's look at gluten-containing foods. This
: Rye, wheat, barley, oats and their processed products (flour and bread from corresponding cereals, bakery, pasta and confectionery products, cereals - wheat, semolina, bulgur, couscous, oatmeal, pearl barley, Hercules, oatmeal, pearl barley , barley, “Artek”, “Poltavskaya”, “7 grains”, “4 grains”, etc., bran, “Muesli”, baby cereals, bread, confectionery, pasta, pancakes, dumplings, manti, cutlets , breaded dishes, etc.)
Gluten Free Products
The following products do not contain gluten.
- Cereals:
rice, buckwheat, corn, millet (millet), Italian millet (chumiza), sago, sorghum, amaranth, quinoa, montina, teff.
- Roots
: potatoes, sweet potatoes, yams, tapioca, cassava.
- Legumes:
soybeans, peas, beans, lentils, chickpeas, mung beans.
- Nuts, chestnuts, carob gum.
- Vegetables and fruits.
- Meat, fish, eggs.
- Milk and natural fermented milk products (kefir, yogurt, fermented baked milk, yogurt, etc.).
- Hard cheeses, butter and vegetable oil.
Products with hidden gluten
Products containing “hidden” gluten:
- Sausages, frankfurters, semi-finished products from minced meat and fish.
- Canned meat and fish, especially in tomato sauce.
- Canned vegetables and fruits, especially tomato pastes and ketchups.
- Ice cream, yoghurts, processed cheeses, margarines with gluten-containing stabilizers.
- Some types of vinegars and salad sauces, mayonnaises.
- Some types of soy sauces.
- Concentrated dry soups, bouillon cubes.
- Instant coffee, cocoa mixtures, teas for “quick preparation”.
- Multi-component dry seasonings and spices.
- Corn flakes when using barley molasses.
- Imitation seafood: “crab” sticks, “crab” meat.
- Caramel, soy and chocolate candies with filling, oriental sweets, industrial jam.
- Kvass and alcoholic drinks - beer, whiskey, vodka, gin.
- Some types of toothpaste, lipstick. Some medications (in excipients).
- Nutritional supplements:
dye annatto extracts E 160b, caramel colors E150a-E150d, oat gum E 411, maltol E 636, ethyl maltol 637, isomalt E953, maltitol and maltitol syrup E965, mono- and diglycerides of fatty acids E471.
Drug treatment in the acute period of celiac disease
- Correction of digestion processes with preparations of highly active microencapsulated pancreatic enzymes (Creon 1000 U for lipase/kg per day).
- Infusion therapy - for severe diarrhea with dehydration and electrolyte disorders.
- IV albumin – for severe nutritional disorders, which are accompanied by anorexia and metabolic disorders (hypoproteinemia, hypoglycemia)
- Enterosorbents – against the background of severe diarrhea (smecta, enterosgel, filtrum, lactofiltrum, etc.)
- The use of loperamide (Imodium) is not indicated
- Correction of intestinal microflora disorders - the use of lactose-free probiotics (Primadophyllus, Linex)
- Calcium malabsorption is corrected by administering calcium (per os or intravenously, depending on the severity) and prescribing vitamin D3 supplements.
- Treatment of anemia - with severe iron deficiency and diarrhea syndrome - parenteral iron supplements, folic acid (per os).
- In case of severe symptoms of hypovitaminosis, additional preparations of fat-soluble vitamins (A, E), C and group B are prescribed.
- For hemorrhagic syndrome, Vicasol (vitamin K) is prescribed parenterally
- The use of glucocorticoid drugs for celiac disease is indicated in cases of severe disease with significant impairment of physical development, for example, with grade III malnutrition with anorexia, and as replacement therapy for the correction of adrenal insufficiency. The drugs are prescribed in standard doses of prednisolone 1 mg/kg body weight, for a short period (2-3 weeks) followed by gradual withdrawal.
Clinical picture
Primary celiac disease usually appears between ages 6 months and 14 years. Artificial feeding promotes earlier development of the disease. The disease is characterized by persistent diarrhea after eating foods containing gliadin (bread, pasta, semolina and oatmeal porridge, cookies and other flour confectionery products, pates, sausages, meat soups, meat sauces). As the disease progresses, malabsorption develops, accompanied by loss of appetite, loss of weight, height and other symptoms (see Malabsorption syndrome), followed by metabolic disorders, exhaustion and dehydration. Children are lethargic, adynamic, irritable, poorly adapt to the environment, and have sleep disorders. The intestines are swollen. When palpating the abdomen, a splashing noise and fluctuation (pseudoascites) are detected. The feces are copious, foamy, whitish, with an oily sheen. The weight of feces per day reaches 1-1.5 kg or more (at a norm of 80-100 g). In the coprogram, fatty acids and soaps predominate. With celiac disease, phenomena of secondary exudative enteropathy are observed - the release and loss of plasma proteins through the intestinal wall, hypoproteinemia and the development of edematous syndrome (see Edema). Together with plasma proteins, the child loses a significant amount of fatty acids, which is accompanied by impaired fat metabolism, impaired absorption of fats and fat-soluble vitamins. More often, the absorption of vitamin D is impaired, as a result of which the child develops rickets-like skeletal changes, osteoporosis, and dental caries; Spontaneous fractures of the bones of the lower extremities are observed. There is a decrease in the level of calcium and phosphorus in the blood, and a decrease in the activity of alkaline phosphatase. With celiac disease, carbohydrate metabolism is impaired, as evidenced by low fasting blood glucose levels, as well as a flat sugar curve during a glucose tolerance test (see Diabetes). Due to insufficient absorption of iron, patients develop hypochromic anemia. The exocrine function of the pancreas in celiac disease suffers little and, unlike cystic fibrosis, a decrease in the activity of its enzymes is observed only during an exacerbation.
Celiac disease occurs in waves, with periods of exacerbation alternating with periods of some improvement.
Challenges of following a gluten-free diet
- Insufficient understanding by patients, parents and attending physicians of the need for strict and lifelong adherence to a gluten-free diet for celiac disease
- Traditional in Russia, widespread use of wheat products and other gluten-containing grains
- The inability to provide adequate nutrition for a child with celiac disease in a preschool, school, sanatorium, or summer camp is social deprivation of children.
Lack of production of domestic gluten-free products, low availability and high cost of imported ones
- The presence of “hidden gluten” in prepared foods, semi-finished products, canned food, seasonings and sauces
- Lack of information from patients and treating doctors about the presence of gluten in products
Celiac disease in children. Kindergarten
Kindergarten and celiac disease:
When a child attends kindergarten, maintaining a gluten-free diet is impossible even with the efforts of cooks and teachers, since the child requires a separate menu, separate kitchen utensils for cooking, separate dishes and a table for eating. Organizing a gluten-free diet in kindergarten is only possible if there are specialized groups for children suffering from celiac disease.
The problem with gluten-free catering in the Krasnoyarsk Territory: Catering
(English cater - supply provisions; catering - public catering). In the Krasnoyarsk Territory, there is no well-functioning system for the existence of patients on a gluten-free diet: the choice of gluten-free products in city stores is very limited, there is no list of proven food products from local producers, and there is no special training system for preparing gluten-free dishes. In addition, no person with celiac disease can feel confident in cafes and restaurants in our city. All foreign guests with celiac disease who visit our city are in the same situation. For example, in Finland, where there are 20,000 people with celiac disease, in every cafe and restaurant, even in a very small town, when opening the menu you can see a mark next to the name of some dishes “GF” (Gluten Free) - this means that this dish can be ordered a person who follows a gluten-free diet.
Refractory disease
In rare cases, patients suffer from refractory disease. These patients do not benefit from a gluten-free diet. They are usually prescribed corticosteroids and immunosuppressive drugs.
If celiac disease is left untreated, your risk of developing certain types of cancer may increase. The study found that "celiac disease is associated with intestinal lymphoma and other forms of cancer, especially adenocarcinoma of the small intestine, pharynx, and esophagus." Complications of celiac disease can include small intestinal ulcers. People with celiac disease may have an increased risk of polyneuropathy.