916
One of the most common diseases that affects the human endocrine system is diabetes. This is a rather dangerous problem that carries with it numerous complications, which together can lead to death. Therefore, research in the field of medicine on this problem is very relevant and is aimed at studying and diagnostic measures to identify a terrible disease, timely recognition of symptoms and determination of associated complications, such as diabetic polyneuropathy , what it is and how this complication arises.
Classification
Based on the type of manifestations and localization of symptoms, the following forms of diabetic polyneuropathies are distinguished:
- Proximal symmetrical polyneuropathy (amyotrophy).
- Asymmetrical proximal neuropathy of large nerves (usually femoral, sciatic or median).
- Neuropathies of the cranial nerves.
- Asymptomatic polyneuropathies.
- Distal types of polyneuropathy.
Distal polyneuropathy is the most common type of diabetic polyneuropathy. It accounts for more than 70% of all types of this disease. The word distal indicates damage to parts of the extremities remote from the body (hands, feet). The lower extremities are more quickly affected. Depending on the nature of the lesion, the following forms are distinguished:
- Sensory.
- Motor.
- Vegetative.
- Mixed (sensorimotor, motor-sensory-vegetative, sensory-vegetative).
Diabetic polyneuropathy what is this diagnosis?
This disease is most often accompanied by pain and loss of sensation in the legs or arms. Diabetic polyneuropathy is the most common complication of diabetes. Its development is observed in almost 50% of people susceptible to this disease, regardless of its type: 1 or 2.
Despite the fact that there are no effective treatments for polyneuropathy, by normalizing blood sugar levels and achieving the correct body weight and certain HbA1 levels, its development can be slightly reduced and pain can be reduced.
Symptoms
The clinical picture of the disease depends on the form of polyneuropathy, the degree of nerve damage, and blood sugar levels.
- Proximal polyneuropathies are characterized, first of all, by the development of impaired muscle trophism, weight loss of the entire limb, and a decrease in its strength. Autonomic and sensory functions are affected to a lesser extent.
- Diabetic cranial nerve neuropathies vary depending on the extent of the individual pair's involvement. Thus, the most common lesion is the oculomotor nerve, which often manifests itself in the form of acutely developing painful ophthalmoplegia. Damage to the optic nerve is characterized by a pronounced decrease in vision, blurred vision, and impaired twilight vision. Less commonly, the trigeminal, trochlear, and facial nerves are affected. The most common cause of cranial nerve damage is acute ischemia, and timely therapy usually leads to good results.
- Asymptomatic polyneuropathies are usually discovered incidentally during a routine neurological examination. They manifest themselves as a decrease in tendon reflexes, most often knee reflexes.
- Distal forms of polyneuropathy usually manifest themselves quite clearly. Thus, the presence of sensory disorders manifests itself in the presence of a crawling sensation in the patient, a painful burning sensation, and numbness in the limb. A person may also notice a pronounced disturbance of sensitivity, perhaps in which he does not feel support and his gait is disturbed. In the distal form of diabetic polyneuropathy of the lower extremities, painful cramps often develop. Gait disturbances can lead to the development of foot deformities and, subsequently, the development of diabetic foot.
Autonomic disorders can lead to the development of tachycardia, hypotensive orthostatic reactions, dysfunction of the intestines and bladder, decreased potency, and impaired sweating. The risk of sudden cardiac death also increases.
Motor disturbances in the distal form of polyneuropathy are rare, especially in the isolated form. They are characterized by the development of hypotrophy of distal muscle groups and a decrease in their strength.
What is diabetic polyneuropathy
The structure of the human peripheral nervous system includes two sections.
- Somatic allows you to control the functioning of your body quite consciously.
- Vegetative monitors the autonomous activity of internal organs and systems.
How does diabetes develop?
Polyneuropathy has all the prerequisites to affect both of these departments.
As a result of diabetes, the nerve endings of a person’s internal organs are subject to extensive damage, leading to the development of this disease.
From the point of view of defining this concept, we can say that this is a type of neuropathy in which the normal functioning of the sensory and motor nerves is hampered.
Read in more detail: Diabetic neuropathy of the lower extremities: timely treatment of a dangerous disease
What happens to nerve endings
- Sensory nerves are responsible for carrying stimuli from the external environment to our central nervous system (i.e. the brain and spinal cord). They control the feelings of touch, pain, cold or heat.
- In this case, the motor nerves are responsible for responding to stimuli. For example, with the contraction of the corresponding muscles that provide movement of the arms and legs.
Diagnostics
Diagnosis of the disease is based on the clinical picture, neurological examination and documented fact of the presence of diabetes mellitus for a long time. In difficult situations, it is necessary to conduct electroneuromyography, which allows identifying initial changes in the conduction of nerve impulses along the fibers, and additional consultation with an endocrinologist.
Clinical picture
At the onset of the disease, diabetic polyneuropathy is manifested by the following first signs:
- numbness of the lower extremities;
- swelling of the feet and legs;
- severe muscle and joint pain syndrome;
- tingling sensation in the legs;
- muscle weakness;
- motor function disorder;
- decreased sensitivity in the lower extremities.
Since patients with diabetes are more likely to have sensory diabetic polyneuropathy, in which the pathological process usually affects the long sensory nerves that go to the hands and feet, the first symptoms of the disease occur in the lower extremities. With the inclusion of small sensory nerve fibers in the pathological process, the following symptoms occur:
- Burning and tingling sensation;
- Loss of skin sensitivity to temperature changes;
- Numbness of the limbs;
- Pain that occurs at night;
- Edema;
- Feeling of chilliness in the feet and hands;
- Redness, dryness and flaking of the skin;
- Long-term non-healing trophic ulcers, wounds;
- Bone calluses.
When long sensory fibers are damaged, skin sensitivity increases, coordination is impaired, and the sense of balance is lost.
Changes occur in the joints, and the motor ability of the fingers deteriorates. Damage to sensory nerves is manifested by complete or partial loss of sensation in the limbs. The patient does not experience pain from burns or frostbite, or mechanical damage to the skin. Wounds do not heal for a long time, and if they become infected, gangrene can develop. In such a situation, surgeons are forced to amputate part of the limb. Patients whose small nerve fibers are affected experience pain in the feet and calf muscles. It can have a different character - be stabbing, dull, aching or tugging. The pain syndrome intensifies in the evening or at night. Sometimes pain begins to bother a patient with diabetes mellitus at the onset of treatment for the disease. As blood glucose levels decrease, the pain usually goes away. If the pain syndrome disappears with high glucose levels, this indicates the progression of the pathological process. When motor nerves are damaged, the patient's muscles weaken and decrease in volume.
If the patient develops extensive damage to the sensory and motor nerves, he feels chilliness or coldness in the extremities, regardless of the ambient temperature. Patients whose small fibers are affected cease to distinguish between hot and cold. This greatly increases the risk of frostbite and burns. The most common symptom of diabetic polyneuropathy, and often the only one, is a feeling of numbness in the lower extremities.
Make an appointment
Treatment
Treatment of diabetic polyneuropathy should be comprehensive and carried out jointly with an endocrinologist and therapist. The first thing you need to do is control your blood sugar levels. Correct diet and basic therapy for diabetes. It is also imperative to exclude the presence of micro- and macroangiopathies and, if necessary, carry out appropriate treatment.
To relieve neurological manifestations, thioctic (alpha-lipoic) acid preparations (berlition and its analogues) are most widely used. Drug therapy is carried out in adequate dosage (the initial dose should be at least 300 mg per day) and in long courses (at least 1.5 months). Symptomatic therapy can also be supplemented with ipidacrine hydrochloride drugs (Axamon, Ipigrix, Neuromidin). B vitamins are also widely used.
In the presence of painful cramps, anticonvulsants (relief of neuropathic pain), antidepressants, opioid drugs can be used (you can read more in my scientific article).
Exercise therapy, physiotherapy, and massage play an important role in the treatment of diabetic polyneuropathy. If there are signs of foot deformation, orthopedic selection of insoles and shoes is necessary. In all cases, the most important role is played by careful skin care and prevention of microdamage.
Patient examination
Neurologists at the Yusupov Hospital make a diagnosis of “diabetic polyneuropathy” based on the patient’s complaints and neurological symptoms.
Clinical examination of the foot includes assessment of vascular status, biomechanics and structure of the foot, and integrity of the skin. Endocrinologists and neurologists recommend that patients with diabetes undergo examinations for the presence of diabetic polyneuropathy once a year, even in the absence of complaints. If there is a suspicion of peripheral nerve damage, examination should be performed at least once every 6 months. Regular examinations make it possible to detect the disease at an early stage and begin adequate therapy in a timely manner. Since it is impossible to identify diabetic polyneuropathy using one research method, doctors at the neurology clinic conduct a comprehensive examination. It includes visual examination, laboratory and instrumental diagnostic methods. Typically, the patient undergoes a comprehensive examination by a therapist, endocrinologist, neurologist and vascular surgeon. Doctors study the following indicators:
- blood pressure level in the extremities;
- severity of reflexes;
- skin sensitivity;
- presence of edema;
- condition of the skin.
In some cases, the disease is asymptomatic, but this does not mean that patients with diabetes do not have damage to peripheral nerve fibers. To identify the pathological process at the preclinical stage, neurologists at the Yusupov Hospital prescribe electromyography and quantitative sensory testing. The latter method allows you to most accurately determine the condition of the sensory nerves, taking into account the weight, height and age of the patient. Laboratory tests for diabetic angiopathy include the following tests:
- determination of glucose levels in blood plasma;
- cholesterol test;
- identifying the level of toxic substances that are in the body.
Also at the Yusupov Hospital, neurologists conduct the following instrumental studies:
- magnetic resonance imaging;
- electroneuromyography;
- nerve biopsy.
Analysis of research results makes it possible to establish an accurate diagnosis before the appearance of clinical signs of diabetic polyneuropathy or at the onset of the disease.
Types of diabetic angiopathy
Diabetic nephropathy develops when the small arteries of the kidneys are damaged and leads to disruption of their function, up to the development of severe renal failure. Diabetic nephropathy is manifested by the appearance of protein in the urine, severe arterial hypertension, and increased levels of creatinine and urea in the blood.
Diabetic retinopathy develops when the retinal arteries are damaged. It is characterized by changes in the vessels of the fundus and hemorrhages in the retina. Can lead to retinal detachment and complete blindness.
Angiopathy of the lower extremities in diabetes mellitus develops through four stages:
- The first stage has no clinical symptoms, however, when examining the vessels, thickening of the arterial walls and their calcification can be detected.
- The second stage is manifested by the appearance of pain when walking over a certain distance (intermittent claudication)
- The third stage is characterized by the appearance of pain in the legs at rest, especially when lying horizontally. If you lower your legs, the pain decreases significantly.
- The fourth stage is manifested by the appearance of trophic ulcers and necrosis on the legs, and diabetic gangrene often develops. This condition is called diabetic foot syndrome.
Focal or multifocal diabetic neuropathy syndrome
The third is the syndrome of focal or multifocal diabetic neuropathy: tunnel neuropathy, cranial neuropathy, amyotrophy, radiculoneuropathy, as well as chronic inflammatory demyelinating polyneuropathy.
Central neuropathy and its types are also distinguished:
- diabetic encephalopathy;
- acute cerebrovascular disorders;
- acute mental disorders.
Even in the clinical classification, several stages of development are distinguished:
- subclinical neuropathy;
- clinical neuropathy (chronic form, acute painful form, form without pain and at the same time too low or complete loss of sensitivity);
- the stage of late complications such as diabetic foot is a specific change in the tissues of the foot that occurs as a result of metabolic disorders in patients with diabetes mellitus. The disease manifests itself as pain in the legs, cracks in the skin and ulcerative lesions, necrosis of soft tissues. At the last stage - gangrene of the foot or lower leg.
Differences between type 1 and type 2 diabetes
In insulin-dependent diabetes mellitus, neuronal processes and capillaries are predominantly affected. This leads to a slowdown in conductivity and a decrease in the strength of the response. Neuropathy is most often partially reversible with early stages and adequate treatment.
In type 2 diabetes, the myelin sheath and large vessels are destroyed, because of this the formation and conduction of impulses is significantly reduced, and the contractility of muscle fibers also decreases. The neurological complications that arise have a continuously progressive course in most patients and there is practically no reverse development.
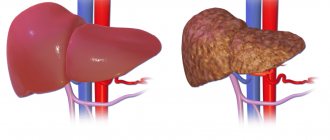
Causes and risk factors
The main role in the pathological mechanism of diabetic neuropathy belongs to microangiopathies, that is, damage to the smallest blood vessels that feed both the vascular walls themselves and the peripheral nerves. Insufficient blood supply to the nervous tissue causes metabolic disorders in it and contributes to the accumulation of oxidative stress products. As a result, the nervous tissue swells and the conductivity of electrical impulses deteriorates. Ultimately, the nerve fiber atrophies.
Diabetic neuropathy is caused by damage to the smallest blood vessels
Factors that increase the risk of developing diabetic neuropathy:
- elderly age;
- arterial hypertension;
- decompensated hyperglycemia;
- long-term diabetes mellitus;
- smoking;
- obesity.
Prevention
To prevent the development of diabetic neuropathy you need:
- control of glucose concentration in blood serum;
- dietary nutrition;
- moderate but regular physical activity;
- strict adherence to the regimen of insulin therapy or taking antihyperglycemic drugs prescribed by the doctor;
- timely treatment of concomitant diseases;
- regular preventive examinations by an endocrinologist, neurologist and other recommended specialists.
Video from YouTube on the topic of the article:
Forecast
Diabetic neuropathy is the most common complication of diabetes. About 50% of people with diabetes have some form of neuropathy. In most cases, it lasts for a long time, about 20 years, and may not show obvious symptoms. However, it is worth noting that the condition will worsen as the disease progresses.
A cure for the disease is impossible, but early diagnosis and prevention allow the patient to live a long and full life. Timely treatment, as well as prevention of risk factors, makes it possible to survive for 20 years. Proper nutrition, a healthy lifestyle, moderate physical activity, and following the doctor’s recommendations will prolong life with diabetic neuropathy.