Chronic or acute cholecystitis with the presence of stones in the gallbladder is called calculous. Concretions - stones of any size are formed in varying quantities in the lumen of the bladder or ducts.
With this inflammatory disease, there is a feeling of heaviness and pain in the right hypochondrium. Also characteristic symptoms for it are nausea and bitterness in the mouth.
When stones move to the area of the bladder neck and common bile duct, the patient develops jaundice and attacks of biliary colic begin.
To diagnose calculous cholecystitis, radionuclide, x-ray, and ultrasound methods of examining the gallbladder are used. Calculous cholecystitis is treated with surgery in the form of cholecystectomy and litholytic therapy. This disease has a long course and always progresses, combining periods of exacerbation and quiescence.
What it is?
One of the manifestations of cholelithiasis is calculous cholecystitis. Along with signs of inflammation of the gallbladder, this disease may cause the appearance of gallstones - stones in the lumen of the gallbladder or in the bile duct.
In the latter case, the outflow of bile is hampered or completely blocked, which results in attacks of biliary colic.
Forms and types
Calculous cholecystitis can occur in acute and chronic form with a complicated or uncomplicated course. Forms of calculous cholecystitis:
- phlegmonous;
- catarrhal;
- purulent;
- gangrenous.
According to the course, atypical, cardialgic, intestinal, typical, esophagalgic calculous cholecystitis are distinguished. Complications of the disease may include biliary pancreatitis, septicopyemia, gallbladder cancer, obstructive jaundice, and purulent cholangitis.
Stages of development
Calculous cholecystitis develops in 4 stages. At the initial stage of the disease, thick bile, microliths in the gallbladder, and bile stasis appear. In the second stage, stones form in the gallbladder. The third stage is characteristic of chronic calculous cholecystitis, and at the fourth stage all possible complications arise. Gallstones in the gallbladder can have different sizes and shapes: multifaceted, branched, round, ovoid.
Calculous cholecystitis in acute form develops after long-term asymptomatic cholelithiasis. As a result of blockage of the common bile duct by a stone, inflammation of the bladder wall begins. Pus accumulates inside the bladder and bile peritonitis forms. Inflammation in the gallbladder develops more slowly in the chronic form of the disease. In this case, it is not infectious in nature.
Prevalence and significance
Approximately 10% of the adult population has calculous cholecystitis. In women it occurs 5 times more often than in men. This disease is usually diagnosed in people over 40 years of age. But sometimes it is detected in childhood.
Risk factors:
- chronic gastritis;
- pancreatitis;
- biliary dyskinesia;
- helminthiases;
- cirrhosis of the liver;
- duodenitis;
- diet high in animal fats;
- long-term use of hormonal contraceptives;
- heredity;
- restriction of motor mode;
- irregular meals;
- injuries of the bladder and ducts.
Description
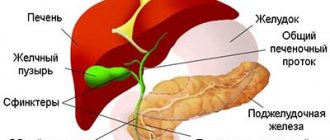
What is it - acute calculous cholecystitis? This is an acute inflammatory process of the walls of the gallbladder, which sometimes spreads to the bile ducts and adjacent organs (usually the pancreas and duodenum). This disrupts the secretion and complete separation of bile, which in turn interferes with the digestion process as a whole.
The pathology disrupts the digestion of fats, the absorption of vitamins, the neutralization of harmful microorganisms in the small intestine (bile has bactericidal properties) and contributes to constipation (bile stimulates intestinal motility).
The course of calculous cholecystitis depends on the size of the stones. Small stones in the body of the gallbladder, not prone to movement, may not appear for a long time. When large enough stones lodge in the bile ducts, they can block them (partially or completely) and prevent the flow of bile.
Stones measuring 3-4 mm are considered relatively safe. Larger stones can cause obstruction (blockage of the duct) and an attack of cholecystitis. If the bile duct is completely blocked, emergency surgery may be required.
The clinical picture and prognosis of calculous cholecystitis differs from the type of stones, which can be:
- cholesterol (X-ray negative);
- lime (calcium);
- pigmented;
- mixed.
Stones can be irregular or round in shape and have sharp edges. The walls of the gallbladder are injured by the sharp edges of the stones, which causes constant inflammation.
Reasons for appearance
The formation of gallstones is associated with stagnation of bile, changes in its composition and the presence of an inflammatory component. As a result of errors in nutrition, infectious diseases, for example, hepatitis, diabetes, obesity, changes occur in the gallbladder. The bile thickens and stagnates, so the gallbladder becomes infected with various pathogenic organisms. Often the development of calculous cholecystitis is associated with acalculous cholecystitis, as a result of which the normal dynamics of gallbladder emptying are disrupted.
Causes of development of chronic calculous cholecystitis.
Among the risk factors for the incidence of chronic cholecystitis, the authors note age, female gender, pregnancy and childbirth, overweight and obesity, rapid weight loss, total parenteral nutrition, fasting, family history (simple dominance of lithogenic genes, enzymatic defects in the synthesis of solubilizers and cholesterol excretion), intake of certain medications (fibrate derivatives, contraceptive steroids, estrogens during postmenopause, progesterone, octreotide and its analogues, ceftriaxone), the presence of diseases such as diabetes mellitus, Crohn's disease, liver cirrhosis, biliary system infections, duodenal and choledochal diverticula.
From a practical point of view, very significant risk factors are the so-called controllable factors - obesity, excess body weight, and the use of low-calorie diets or fasting to reduce weight. It has been established that CCH occurs in 33% of obese individuals. In the USA, a study was conducted for 10 years showing that women with excess body weight (body mass index in the range of 25 - 29.9) have an increased risk of developing CCH, which, along with hypertension, diabetes mellitus and coronary heart disease, increases with age. an increase in the degree of obesity, while a BMI of more than 35 increases the likelihood of developing the disease by 20 times, both in women (relative risk 17.0) and men (relative risk 23.4). The situation is complicated by the fact that the use of diets with a very low total calorie content, as well as a decrease in body weight by more than 24% of the original, at a rate of 1.5 kg or more per week, represents an additional risk factor for the formation of cholelithiasis.
In the mechanism of gallstone formation, important importance is attached to changes in the biochemical composition of bile. For the formation of gallstones, the simultaneous existence and long-term action of such factors as the supersaturation of bile with cholesterol and the formation of a crystallization nucleus, an imbalance between pronucleating and antinucleating factors, a decrease in the evacuation function of the gallbladder, as well as dysfunction of the enterohepatic circulation of bile acids is necessary. The basis for the formation of cholesterol stones is the hepatic secretion of vesicles enriched with cholesterol. The mechanisms of development of the vesicles themselves and the factors that control this process are not well understood and are the subject of active research.
How can it manifest itself?
With acute calculous cholecystitis, acute pain appears in the right hypochondrium and epigastrium. It radiates under the shoulder blade, into the neck, lower back, and shoulder girdle. An attack of colic can begin after drinking alcohol, physical stress, eating fatty or spicy foods, or after stress. The patient develops vomiting and low-grade fever.
With chronic calculous cholecystitis, the patient experiences bitterness in the mouth and nausea. Blockage of the bile duct by a stone causes obstructive jaundice, which also manifests itself in dark urine and discolored stool.
With phlegmonous, gangrenous forms, febrile temperature, severe intoxication, hypotension, severe pain and repeated vomiting appear. The patient’s blood pressure also drops sharply and weakness appears.
Symptoms
In the initial stage of calculous cholecystitis, symptoms often do not manifest themselves by external signs. This significantly complicates differential diagnosis and subsequent therapy.
With the development of an acute inflammatory process, typical signs of the disease appear:
- sharp pains that are localized under the ribs on the right and radiate to the scapula;
- nausea and vomiting of bile;
- increased body temperature (up to 38 degrees);
- a sharp decrease in blood pressure;
- general weakness, cold sweat;
- feeling of dry mouth;
- heartburn, belching;
- dark urine;
- light stool;
- signs of obstructive jaundice.
Diagnostic methods
In case of acute cholecystitis, hospitalization in a hospital is required, as urgent surgery may be necessary. Surgical treatment of chronic cholecystitis is performed in a clinic or hospital setting.
Diagnosis of the disease is based on the following methods:
- palpation of the right hypochondrium;
- analysis of laboratory and instrumental research results;
- Ultrasound of the gallbladder;
- study of liver blood samples and pancreatic enzyme levels;
- echography;
- transhepatic cholangiography;
- cholecystography: oral or intravenous;
- coprograms-stool analysis;
- duodenal intubation;
- examination of general blood and urine tests;
- MRI;
- radionuclide diagnostics;
- ECG in the cardialgic form of calculous cholecystitis.
Medical educational literature
Metabolic disorders in the body are manifested by disturbances in the metabolism of cholesterol, bile pigments and calcium metabolism. Back in 1862, Thudichum noted that the precipitation of cholesterol is prevented by taurocholic acid, as well as a certain balance between the content of cholesterol and bile acids in bile. The content of bile acids in the human body depends on protein metabolism. A decrease in the content of bile acids occurs during fasting, when the total amount of bile secreted by the liver decreases, as well as with toxic damage to the liver.
Normally, the concentration of bile in the gallbladder increases 4-6 times, which is accompanied by an increase in the amount of cholesterol in it to 400 mg% with a simultaneous increase in the amount of bile acids contained in bile to 1-10 g%. A decrease in the amount of bile acids in bile while maintaining a high concentration of cholesterol in it promotes stone formation. The fact that an increase in cholesterol concentration occurs in the gallbladder explains the formation of gallstones in the gallbladder.
In 1972, Admirand and Small, who studied the pathophysiological mechanisms of the formation of cholesterol stones, found that the formation of gallstones is facilitated by the oversaturation of bile with cholesterol and a decrease in the content of bile acids and phospholipids, which is defined as an increase in the “lithogenicity” of hepatic bile.
The fact that the formation of gallstones requires the presence of metabolic disorders is supported by the fact that hypsarbilirubinemia was detected in patients whose gallstones were based on pigmented formations.
Stagnation of bile is an important factor contributing to the formation of gallstones. This is convincingly proven by the works of Aschoff (1906), in which it was noted that in all cases, in the presence of stones in the gall bladder, an inflammatory process was found in the wall of the gallbladder, leading to a violation of its contractile function and stagnation of bile in it. At the same time, there are indications in the literature that gallstones are found in patients with preserved contractile function of the gallbladder.
Morphogenesis of calculous cholecystitis.
It is now well known that morphologically “primary acute cholecystitis” occurs as a casuistry, and where the clinical picture corresponds to acute cholecystitis, microscopic examination almost always reveals the presence of an exacerbation of a chronic inflammatory process. It has also been established that age-related changes in the vessels of its wall contribute to the development of pathological changes in the gallbladder.
To study the morphogenesis of the gallbladder in calculous cholecystitis, gallbladders were studied in the corpses of people who did not suffer from cholecystitis, as well as gallbladders removed during surgery and containing stones (V.V. Vinogradov, S.I Levina, 1970). At the same time, attention was paid to changes in the wall of the gallbladder depending on the age of the patient.
Histological studies have shown that in the area of the neck of the gallbladder, which does not contain stones, there is no muscle layer. Its mucous membrane does not have mucous glands, it does not have the so-called Rokitansky-Aschoff sinuses, and the outer fibrous layer is more pronounced than the muscular layer.
With age, in patients without cholelithiasis, an increase in the collagen fibers of the middle layer is noted in the wall of the gallbladder, trophic changes appear in the muscle layer, which is expressed by the formation of fibrosis in the form of fibrous layers. Moreover, the older the patient is, the more pronounced are the dystrophic changes in the wall of the gallbladder. The listed changes can undoubtedly contribute to disruption of the motor function of the gallbladder, stagnation of bile in it, as well as creating a background for the development of the inflammatory process in the wall of the gallbladder and the formation of stones in it.
A histological study of gallbladders in people of different age groups who did not suffer from cholelithiasis also showed that with age, significant changes are also found in the vascular system of the gallbladder: arterial, venous and lymphatic. And if we take into account that gallstone disease occurs mainly in elderly people, then we can assume that the changes that occur in the vascular system of the gallbladder are the background for stone formation.
A study of the gallbladder wall in patients with cholelithiasis showed that muscle elements described by Lütkens and called the Lütkcns sphincter appear in it in the area of the bladder neck. The appearance of these muscle elements during inflammation of the gallbladder can be considered as a compensatory-adaptive reaction to preserve the contractile function of the gallbladder, which is impaired during inflammation.
The study of biopsy material of the gallbladder in case of cholelithiasis made it possible to establish that the morphological changes in its wall, characteristic of calculous cholecystitis, develop over a long period of time. Therefore, cases that are usually interpreted as acute cholecystitis should refer to exacerbation of chronic cholecystitis and should be regarded as a complication in the course of the disease.
Since the pronounced morphological changes in the gallbladder wall present in calculous cholecystitis do not depend on the type and nature of gallstones, it is more correct to assume that gallstones are not a cause, but a consequence of cholecystitis. This provision is of a fundamental nature. Considering the cause of the formation of stones in the gall bladder to be an inflammatory process in it, and not gallstone diathesis, it should be recognized that a complete cure of a patient with calculous cholecystitis and elimination of the possibility of recurrence of suffering can be achieved with timely and correctly performed surgical intervention.
Based on the above, three stages of gallstone disease can be distinguished.
The first stage is physical and chemical. At this stage, the liver produces bile oversaturated with cholesterol, with a decrease in the content of bile acids and phospholipids (lithogenic bile). There are no clinical manifestations.
The second stage is latent asymptomatic stone carriage. This stage is characterized by the same physicochemical changes in the composition of bile as in the first stage, as well as the formation of gallstones. The process of stone formation at this stage is associated not only with physicochemical changes in bile, but also with the development of conditions for stagnation of bile in the gallbladder, changes in the permeability of its mucous membrane, as well as with the occurrence of an inflammatory process in the wall of the gallbladder. There are no clinical manifestations of the disease at this stage, and gallstones are discovered accidentally during routine examinations of patients or at autopsy.
The third stage is marked clinical manifestations. At this stage, clinical signs associated with the development of complications of calculous cholecystitis arise: acute inflammation in the gallbladder, choledocholithiasis, stenosis of the major duodenal papilla, acute cholangitis, acute pancreatitis. Signs of acute inflammation can be mild and occur in the form of mild attacks of “biliary colic,” which characterizes the chronic course of calculous cholecystitis.
Clinical picture of calculous cholecystitis.
In surgical practice, we have to deal with patients with the third stage of cholelithiasis, which occurs in the form of chronic calculous cholecystitis or manifests itself as complications.
Chronic calculous cholecystitis is usually manifested by the presence of unpleasant sensations or constant, aching pain in the right upper quadrant of the abdomen. In some cases, there are recurrent attacks of pain in the right hypochondrium associated with eating fatty or fried foods. However, these attacks are short-lived, often go away on their own and cause little concern to the patient.
Often the clinical picture of chronic calculous cholecystitis is expressed by symptoms characteristic of diseases of the stomach or intestines (gastritis, colitis). Patients complain of belching with bitterness and air, nausea, flatulence, constipation or diarrhea.
A special place among patients with chronic calculous cholecystitis is occupied by patients whose leading symptom of the disease is pain of a spasmodic nature, localized behind the sternum and radiating to the left scapula and shoulder girdle, which is commonly called “reflex angina.” Patients with the cardiac form of cholecystitis are usually treated for chronic coronary insufficiency, since during an attack of pain the ECG shows signs of impaired myocardial nutrition. These changes disappear after the pain disappears, and a correctly collected history of the disease and examination of the biliary system allows one to diagnose calculous cholecystitis.
Painful forms of chronic calculous cholecystitis occur with typical attacks of pain in the right hypochondrium (biliary colic), often radiating to the right shoulder and the area of the right scapula, as well as to the neck area. These pains usually occur after an error in diet and are accompanied by nausea and vomiting. In this case, catarrhal inflammation develops in the gallbladder, there are no signs of a purulent process.
Biliary colic occurs as a result of an increase in pressure in the lumen of the gallbladder or in the entire biliary system, caused by sudden blockage of the neck of the gallbladder or cystic duct with a stone, as well as a sharp spasm of the sphincter of Oddi muscles or blockage of the bile duct in the area of the large duodenal papilla with a small stone when passing through it. duodenum.
Examination of the patient reveals pain and moderate muscle protection in the right hypochondrium upon palpation of the abdomen. With a soft abdomen during biliary colic, it is possible to palpate an enlarged, tense and painful gallbladder. Tapping along the right costal arch causes increased abdominal pain (positive Ortner-Grekova symptom). There are no signs of peritoneal irritation, and body temperature usually does not rise.
After injection of antispasmodic drugs, the attack of biliary colic subsides and the patient's condition improves.
Outcomes of chronic calculous cholecystitis. A chronic inflammatory process in the gallbladder, occurring against the background of a blockade of the neck of the gallbladder or cystic duct when the absorption function of the mucous membrane of the gallbladder is impaired, can result in the development of hydrocele of the gallbladder.
As a result of frequent exacerbations of the chronic inflammatory process in the wall of the gallbladder, it sharply thickens, takes on a cartilaginous consistency, the gallbladder itself shrinks, and its cavity decreases. All this contributes to the formation of a sclerotic gallbladder.
In 5-7% of patients suffering from chronic calculous cholecystitis, gallbladder cancer occurs.
Complicated calculous cholecystitis. The chronic course of the inflammatory process in the gallbladder is often accompanied by the development of various complications, which can be divided into two groups (Scheme 7).
Complication of calculous cholecystitis
This division is arbitrary, since in clinical practice there are often cases where there are combined lesions of the gallbladder and bile ducts.
Peritoneal forms of cholecystitis are characterized by the spread of the inflammatory process throughout the thickness of the gallbladder wall and its transition beyond its limits.
Phlegmonous cholecystitis.
The occurrence of this form of cholecystitis is facilitated by microbial factors and impaired evacuation function of the gallbladder. The inflammatory process quickly covers the entire thickness of the gallbladder wall, which leads to purulent impregnation of it and the infection spreading beyond the gallbladder.
The clinical picture of phlegmonous cholecystitis is characterized by an acute onset of the disease. After an error in diet, a patient experiences severe pain in the right hypochondrium with typical irradiation along the right phrenic nerve. The pain is accompanied by repeated vomiting and an increase in body temperature to 38-390 C.
Patients with phlegmonous cholecystitis behave restlessly. Their tongue is dry and coated. The upper abdomen lags behind in the act of breathing. When palpating the abdomen, severe pain and muscle tension in the right hypochondrium are noted. The Ortner-Grekov symptom is sharply positive. There is a positive Mussy symptom (pain when pressing with a finger above the collarbone on the right between the anterior legs of the sternocleidomastial muscle). Despite the presence of muscle protection, in many patients it is possible to palpate an enlarged, tense and painful gallbladder or perivesical infiltrate. An increased (up to 15,000-18,000) number of leukocytes with a shift in the leukocyte formula to the left is detected in the peripheral blood.
The disease, as a rule, progresses with an increase in the phenomena of local or general peritonitis.
Gangrenous cholecystitis is the most severe form of acute cholecystitis, accompanied by the development of local or general peritonitis. This form of cholecystitis often occurs as a result of the progression of phlegmonous inflammation in the wall of the gallbladder. According to some authors, necrosis of the gallbladder wall is promoted by thrombosis of the main trunk or individual branches of the cystic artery. Other researchers consider gangrene of the gallbladder wall to be a consequence of severe infection due to hyperergic allergic sensitization of the patient’s body.
The clinical picture of gangrenous cholecystitis is in many ways reminiscent of the clinical picture of phlegmonous cholecystitis, but with more pronounced intoxication of the body: pointed facial features, high body temperature, repeated vomiting, dry tongue. When examining the abdomen in the right hypochondrium, a symptom of peritoneal irritation is revealed (Shchetkin’s symptom - Blumberg).
If, with gangrenous cholecystitis, a delimiting infiltrate does not have time to form around the gallbladder, the Shchetkin-Blumberg symptom is detected in all parts of the abdomen.
Outcomes of acute cholecystitis. When an acute inflammatory process in the gallbladder occurs against the background of a blockade of the cystic duct, acute empyema of the gallbladder (accumulation of pus in the lumen of the gallbladder) may develop. In patients with acute empyema of the gallbladder, despite anti-inflammatory treatment, high body temperature remains, accompanied by chills and increased sweating. Slight yellowing of the skin and sclera is often detected, nausea and vomiting continue. An enlarged, tense and painful gallbladder or inflammatory infiltrate is detected in the right hypochondrium. The Ortner-Grekov symptom is sharply positive. The picture of white blood indicates a purulent inflammatory process (severe leukocytosis, increased ESR), protein, casts, and red blood cells appear in the urine - signs of toxic nephritis.
Perforated cholecystitis is a consequence of phlegmonous or gangrenous inflammation of the gallbladder wall. As a result of necrosis of the gallbladder wall, its infected contents leak out. In this case, the contents of the gallbladder can exit into the free abdominal cavity, causing the development of general peritonitis, or into a cavity limited by an inflammatory infiltrate, or into the lumen of a hollow organ fused to the gallbladder.
The clinical picture of gallbladder perforation largely depends on the phase of development of the inflammatory process in the gallbladder, the period from the onset of the disease and the degree of formation of adhesions around the gallbladder (on the formation of a delimiting infiltrate). Perforation of the wall of the gallbladder and the entry of its contents into the free abdominal cavity is manifested by a sudden increase in pain in the upper abdomen with a simultaneous deterioration in the general condition of the patient. The clinical picture of acute general peritonitis comes to the fore.
If perforation of the gallbladder wall occurs in the conditions of a formed infiltrate delimiting the abdominal cavity, a picture of limited peritonitis and subhepatic abscess develops.
Perforation into a hollow organ (stomach, duodenum or colon) leads to the formation of an internal biliary fistula. In some cases, the entry of a stone into the lumen of the duodenum and its movement through the intestine can cause the development of acute intestinal cholelithiasis.
Obstructive forms of cholecystitis are characterized by the presence of partial or complete obstruction of the main bile ducts, the cause of which may be a gallstone released into the hepatobiliary duct from the gallbladder (choledocholithiasis), or an inflammatory (scarring) process that occurs in the distal bile duct due to damage to its mucous membrane by small particles. a calculus passing into the duodenum (stenosis of the major duodenal papilla). The clinical picture of obstructive forms of cholecystitis is manifested by the development of jaundice and acute cholangitis. Since blockage of the distal bile duct can lead to an inflammatory process in the pancreas, some cases of cholecystitis accompanied by blockage of the bile duct occur as cholecystopancreatitis.
The most common symptom of obstruction of the main bile ducts is jaundice (icterus) - a condition of the body accompanied by yellow staining of the sclera, mucous membranes and skin, resulting from an increase in the amount of bilirubin in the patient’s blood. Since hyperbilirubinemia in complicated calculous cholecystitis occurs due to obstruction of the bile ducts, jaundice is mechanical in nature; which is characterized by an increase in the total amount of bilirubin in the blood due to its direct fraction.
Obstruction of the main bile ducts leads to stagnation of bile in them (biliary hypertension) and expansion of their diameter (cholangiectasia). Stagnation of bile in the biliary system is accompanied by morphological changes in liver tissue and disruption of its function. Liver failure is still considered the most common and severe complication of mechanical obstruction of the bile ducts and in 50% of cases is the cause of death in patients in the postoperative period.
Jaundice in cholelithiasis, as a rule, appears after an attack of pain in the right hypochondrium, which is characteristic of painful forms of cholecystitis. When examining patients, they reveal a clinical picture of acute cholecystitis.
A violation of the outflow of bile into the duodenum, which occurs against the background of an acute inflammatory process in the gallbladder, leads to the development of inflammation in the bile duct system - acute cholangitis. Morphological changes in the wall of the bile ducts in acute cholangitis can be represented by catarrhal, phlegmonous or gangrenous inflammation.
The clinical picture of acute cholangitis is characterized by the presence of signs of general intoxication of the body. The main symptom of acute cholangitis is high temperature (up to 39-40°C), which is accompanied by chills and profuse sweating at night. Patients complain of nausea, vomiting, and lack of appetite. In the peripheral blood, leukocytosis is detected with a shift in the leukocyte formula to the left, and the ESR increases.
The close anatomical and functional relationship of the biliary system and the pancreas contributes to the fact that in acute cholecystitis the pancreas is involved in the inflammatory process. There are three points of view on the mechanism of development of the inflammatory process in the pancreas during acute cholecystitis (cholecystopancreatitis):
- reflux of infected bile into the pancreatic duct when the large duodenal papilla is blocked by a stone, with swelling or stenosis of the large duodenal papilla in patients with a common ampulla for the bile and pancreatic ducts;
- spread of the inflammatory process from the gallbladder to the pancreas through the blood and lymphatic vessels;
- impaired evacuation of pancreatic juice due to blockade of the major duodenal papilla.
The clinical picture of acute cholecystopancreatitis is represented by symptoms of damage to both the gallbladder and bile ducts, and the pancreas. Patients complain of pain in the right hypochondrium or epigastric region, often radiating to the back and having a girdling character. Often the pain radiates to the left shoulder - a left-sided phrenicus symptom. Vomiting with cholecystopancreatitis is persistent and painful. Body temperature 38-39° C.
When palpating the abdomen, patients feel pain both at the point of the gallbladder and in the area where the pancreas is located - the navel. With deep palpation to the left and above the navel, it will often be possible to detect a weakening of the pulsation of the abdominal aorta - a positive Voskresensky sign. Involvement of the tail of the pancreas in the inflammatory process is manifested by the appearance of the Mau-Robson symptom (the appearance of pain on palpation in the area of the left costovertebral angle).
Already in the first hours of the disease in patients with cholecystopancreatitis, an increase in the level of blood amylase and urine diastase is detected. In the peripheral blood there is high leukocytosis and aneosinophilia.
Diagnosis of calculous cholecystitis and its complications is based on a comprehensive examination of the patient using special research methods used in the preoperative period and during surgery.
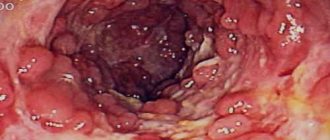
Recently, the main special research method for identifying pathological processes in the gallbladder, extrahepatic bile ducts and pancreas is ultrasound tomography. Using this study, it is possible to detect stones in the gallbladder and determine the form of inflammation of the gallbladder (Fig. 44).
Ultrasound tomograms for acute cholecystitis
It reveals a pathological process localized in the hepatobile duct, in the large duodenal papilla and in the pancreas (Fig. 45).
Rice. 45. Ultrasound tomograms for choledocholithiasis (A), stenosis of the bile duct (B), bile duct stricture (C): a - stone; b - bile duct; c — zone of stenosis: d — zone of stricture
The pathological process in the gallbladder and bile ducts can be identified using x-ray examination, which is carried out using a number of techniques:
I. Indirect contrasting of the biliary system.
- Plain plain radiography of the liver and extrahepatic bile ducts.
- Excretory cholecystocholangiography:
- oral;
- intravenous.
II. Direct contrast of the biliary system.
- Percutaneous cholecystocholangiography under laparoscopic control.
- Percutaneous transhepatic cholangiography under X-ray control.
- Percutaneous transhepatic cholangiography under ultrasound guidance.
- Endoscopic retrograde cholangiography.
- Fistulocholecystocholangiography.
- Operative cholecystocholangiography.
X-ray examination techniques based on indirect (excretory) contrasting of the organs of the biliary system are currently practically not used, since their information content is low. As for X-ray examination methods, which are based on direct contrasting of the organs of the biliary system, they are used in patients with mechanical obstruction of the biliary tract (obstructive jaundice). 25-30% solutions of water-soluble iodide preparations (cardiotrast, diodone, biligrafin, bilignost, etc.) are used as contrast agents.
Percutaneous puncture of the organs of the biliary system with subsequent injection of a contrast solution into them can be performed under laparoscopic control (percutaneous transvesical cholecystocholangiography - Fig. 46); under X-ray or ultrasound control (percutaneous transhepatic cholangiography - Fig. 47, Direct contrasting of the extrahepatic bile ducts is possible by retrograde injection of a contrast solution into them during endoscopic examination of the duodenum (endoscopic retrograde cholangiography - Fig. 47, b).
Percutaneous laparoscopic cholecystocholangiography
In cases where in the preoperative period it is not possible to clearly determine the condition of the extrahepatic bile ducts, to identify choledocholithiasis and stenosis of the major duodenal papilla, the extrahepatic bile ducts are examined during surgery (operative cholangiography - Fig. 47, c).
Radiographs with direct contrast of the bile ducts
During surgery, the bile duct can be examined using special fiberscopes. This research method allows you to identify the inflammatory process in the wall of the bile duct (cholangitis), as well as detect stones that were not removed during choledocholithotomy.
If you find an error, please select a piece of text and press Ctrl+Enter.
Pages: 2
Treatment
During remission of chronic calculous cholecystitis, you need to adhere to a diet and limit physical activity. Litholytic drug therapy or shock wave therapy to break up the stones may also be prescribed.
In the treatment of all types of cholecystitis, conservative therapy only temporarily brings relief to the patient and reduces the symptoms of inflammation. To prevent further formation of gallstones, it is necessary to eat properly and normalize metabolism.
Drugs
Hospitalization of the patient in a surgical hospital is necessary in case of exacerbation of the chronic form of the disease and acute calculous cholecystitis. The patient is prescribed antibacterial, antiemetic, antispasmodic and anticholinergic drugs. Inpatient detoxification is also carried out with special solutions.
With this disease, it is forbidden to self-medicate, as this threatens the death of the patient. Litholytic therapy is prescribed when the symptoms of the disease decrease. For this purpose, medications are used that dissolve gallstones. These include Henofalk, Litofalk, Ursosan and others. The use of antispasmodic drugs is also recommended.
Surgery
Surgical treatment is carried out as planned after the patient’s condition has stabilized. Removal of the gallbladder with stones is called laparoscopic cholecystectomy, which is the least traumatic way to solve the problem. Under the control of a monitor, the patient is given punctures using manipulators in the abdominal cavity.
In complicated forms of calculous cholecystitis, open cholecystectomy is performed. Percutaneous cholecystostomy is sometimes prescribed for elderly patients.
Treatment with folk remedies
It is very dangerous to use decoctions and infusions of herbs with choleretic properties for this disease. They can lead to increased movement of stones, which can cause colic, blockage of the bile duct and exacerbation of the disease.
Diet
A prerequisite for treatment of the disease and good health is adherence to a diet. It leads to dilution of bile and elimination of inflammation due to the content of beneficial substances.
You can eat lean meats, fish, sausages, fruits, vegetables, and herbs. For any cholecystitis, pears are useful, as they help the patient recover faster. It is also useful to eat oatmeal, buckwheat, pasta, low-fat dairy products, and yoghurts with bifidobacteria to prevent intestinal dysbiosis.
For calculous cholecystitis, it is recommended to eat dried or stale bread, bran products, natural unrefined vegetable oils, jam, and marmalade. To reduce the risk of painful attacks with cholecystitis, you can drink beetroot juice.
Sweet fruit compotes, jelly, juices, rosehip infusion, weak tea, coffee with milk, and chicory are also allowed. To reduce inflammation in the gallbladder and enhance bile drainage, you can add turmeric to your food.
With this disease, you should not eat foods that cause irritation to the mucous membranes and complicate the digestion process. It is especially dangerous to eat saturated fats, legumes, mushrooms, sour fruits and berries, smoked foods, canned food, carbonated drinks and alcohol. You should eat less sugar and salt.
Transvaginal laparoscopic cholecystectomy using NOTES technology
In 2007 in France, and since 2008 in Russia, a new unique technique for removing the gallbladder without punctures on the anterior abdominal wall, which does not leave postoperative sutures or scars, appeared - this is transvaginal cholecystectomy using NOTES technology! The essence of this technique is access to the diseased organ through the posterior vaginal fornix (puncture - 1 cm). Through a special device inserted through the posterior fornix into the abdominal cavity, laparoscopic instruments and optics are passed, then cholecystectomy is performed, as in laparoscopic surgery. Then the gallbladder is removed from the abdominal cavity also through the posterior vaginal fornix, on the puncture of which one suture is applied from a synthetic absorbable suture material (resorption period 3-4 weeks).
The advantages of laparoscopic cholecystectomy using NOTES technology are as follows:
- no pain after surgery;
- maximum physical activity;
- hospitalization for only one day;
- excellent cosmetic effect.
The only restriction in the postoperative period is sexual rest for one month. It should be noted once again that transvaginal cholecystectomy does not affect the female genital organs (uterus, appendages, etc.) and does not affect their functioning. After this operation, there are no incisions left on the abdominal wall (maximum one invisible puncture in the umbilical area). The patient is discharged from the hospital the next day and begins work on days 7–10; sports are possible within two weeks.
Prevention and prognosis
To prevent calculous cholecystitis, it is necessary to remove the factors that lead to the formation of gallstones. It is important to follow a low-calorie plant-based diet and reduce emotional and physical overload. It is of great importance to follow all doctor’s recommendations and reduce body weight. To prevent possible serious complications, timely surgical treatment of calculous cholecystitis is necessary.
If diagnosis is delayed, various complications arise that can only be eliminated surgically. Untimely medical intervention leads to the development of peritonitis, sepsis and death. With calculous cholecystitis, the prognosis is generally favorable, but it is necessary to consult a doctor in time and strictly follow all his recommendations.
Types of disease
Inflammation of the gallbladder with the formation of stones is classified into three types:
- Catarrhal. It is characterized by thickening of the walls of the gallbladder as it enlarges and pronounced swelling of the tissues with redness. This is the easiest and most favorable type of this disease. The prognosis for patients with catarrhal form of the disease is good: with timely and correct treatment, there is a chance to get rid of the “sore” forever.
- Phlegmous. With this variant of the disease, the walls of the enlarged gallbladder become even thicker, and the organ cavity is filled with purulent contents. It is this stage that often develops into a chronic disease and provokes serious, sometimes irreversible changes in the bladder.
- Gangrenous. This type of disease is considered the most dangerous. It is accompanied by pronounced changes in the organ and the formation of gangrene with ulcers on the walls of the bladder. This process can lead to rupture of the walls, perforation of a hollow organ, which will result in the pouring of purulent contents into the abdominal cavity and end in peritonitis. In addition to peritonitis, such a disease can provoke other complications such as sepsis, purulent abscesses, and acute cholangitis.
Unlike the catarrhal stage, which may not appear externally, the phlegmous and gangrenous type of acute calculous cholecystitis makes itself felt with obvious symptoms: pain, vomiting, weakness, hyperthermia, dyspeptic disorders and other conditions.
When to see a doctor
Calculous cholecystitis is considered a rather serious disease. If its symptoms appear, you must immediately contact a specialist who will prescribe examination and treatment.
First you need to visit a gastroenterologist who treats chronic pathologies of the digestive tract. However, acute conditions are treated in an inpatient surgical department, so you can also contact a surgeon. It is worth remembering that delaying a visit to a specialist is strongly discouraged.