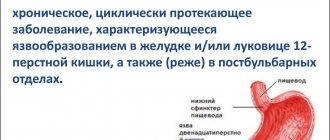
An ulcer, or gastric ulcer, is actually an open wound on the mucous membrane of the organ. When the phrase “stomach ulcer” is uttered, they most often mean peptic ulcer - a chronic disease that lasts quite a long time, can recur and lead to serious complications.
Our expert in this field:
Ozdoeva Tamara Akhmetovna
Gastroenterologist
Call the doctor
Some facts and figures:
- Most often, peptic ulcer disease develops between 20 and 40 years of age.
- A twentieth of adults worldwide suffer from stomach or duodenal ulcers.
- Urban residents get sick more often than rural residents.
- Men get sick about 6 times more often than women.
Why and how does an ulcer develop?
| Helicobacter pylori infection | The main reason for the development of the disease. This spiral-shaped bacterium causes 45-75% of all cases of stomach ulcers. The source of infection is a sick person or a bacteria carrier. The microbe can be transmitted through:
|
| Due to taking medications | The second most common cause of pathology. These medications include:
|
| As a complication of various chronic diseases |
|
| As a result of acute diseases and conditions (so-called “stress ulcers”) |
|
| Social reasons |
|
What are the types of stomach ulcers?
| By localization they distinguish: | According to the number of ulcerative lesions: | By defect size: | By stages of development: |
|
|
|
|
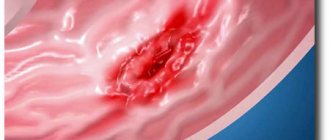
Symptoms of a stomach ulcer
Signs of pathology can be quite varied; they depend on the size and location of the defect, individual sensitivity to pain, the phase of the disease (exacerbation or remission), the presence of complications, the age of the patient and concomitant pathology.
Pain is the main symptom of a stomach ulcer. The pain syndrome has some features:
- pain can be early (in the first couple of hours after eating, if the defect is located in the body or cardia of the stomach), late (more than two hours, usually when localized in the pylorus), fasting or hungry (disturbed before meals) and night (usually appear during second half of the night);
- pain may appear and disappear, depending on the activity of the inflammatory process;
- pain tends to worsen in spring and autumn;
- by nature it can be sharp, cutting, pulling, stabbing, blunt, and so on;
- the pain goes away after taking antisecretory medications and antacids;
- its intensity varies, from mild discomfort to unbearable sensations;
- usually experiences pain in the epigastrium, left side of the chest, behind the sternum, left arm or back. Atypical localization of pain is the right hypochondrium, lumbar region, pelvis.
It should be remembered that about 20% of patients do not have pain. This usually happens in old age, with diabetes, or taking NSAIDs.
Other signs of peptic ulcer:
- heartburn is a burning sensation in the epigastric region. The reason for its appearance is the entry of aggressive acidic gastric contents into the lumen of the esophagus;
- nausea and vomiting are caused by impaired gastric motility. Vomiting occurs a couple of hours after eating and causes relief;
- belching is a sudden involuntary reflux of a small amount of gastric juice into the oral cavity. It is characterized by a sour or bitter sensation in the mouth. Belching occurs due to disruption of the cardiac sphincter.
- loss of appetite - appears due to a violation of the motor function of the gastrointestinal tract, or a person consciously refuses to eat for fear of pain;
- constipation – delay in bowel movements for more than 2 days. Occurs due to increased secretion of hydrochloric acid and retention of food in the stomach;
- a feeling of heaviness in the stomach that occurs after eating;
- fast saturation;
- feeling of bloating.
Anticholinergics
In this group of medications, the most commonly prescribed medications are:
- Gastrocepin. Synthetically produced drug. Does not affect the functioning of the myocardium, salivary and sweat glands. During treatment, there is a decrease in the activity of receptors in the gastric mucosa, which is expressed in a decrease in the volume of pepsin.
- Buskopan. Blocks the processes of choline production in the stomach. It does not have a negative effect on other organs. At the same time, it has an analgesic effect.
- Platyfillin. It has a vasodilator, antispasmodic and sedative effect. Blocks cholinergic receptors. In large dosages, it inhibits gastric secretion. Side effect: tachycardia.
Complications
Like many other diseases, stomach ulcers can have complications, sometimes quite dangerous. These include:
Penetration
Penetration is the destruction of the stomach wall, with the bottom of the ulcer becoming a nearby organ. This is usually the pancreas. Hydrochloric acid and pepsin destroy its structure, causing acute destructive pancreatitis. The first symptoms of penetration are sharp girdling pain in the abdomen, fever and an increase in alpha-amylase in the blood.
Perforation
Perforation is the destruction of the wall of an organ and the entry of its contents into the abdominal cavity or retroperitoneal space. Occurs in 7-8% of cases. Violation of the integrity of the wall can be caused by lifting weights, heavy physical labor, eating fatty and spicy foods, and drinking. The clinical picture is characterized by all the signs of general peritonitis (general weakness, abdominal pain throughout, intoxication, and others).
Plain radiography of the abdominal cavity in a vertical position helps to diagnose gastric perforation! On it you can see a disc-shaped clearing (gas) under the dome of the diaphragm.
Malignancy
Malignancy is the degeneration of an ulcer into stomach cancer. This complication occurs infrequently, in approximately 2-3% of patients. It is noteworthy that duodenal ulcers never transform into a malignant tumor. As cancer develops, patients begin to lose weight, they develop an aversion to meat foods, and their appetite is reduced. Over time, symptoms of cancer intoxication appear (fever, nausea, vomiting), pale skin. A person can lose weight up to cachexia (complete exhaustion of the body).
Pyloric stenosis
Pyloric stenosis occurs if the ulcerative defect is localized in the pyloric region. The pylorus is the narrowest part of the stomach. Frequent relapses lead to scarring of the mucosa and narrowing of the pylorus. This leads to disruption of the passage of food into the intestines and its stagnation in the stomach.
There are 3 stages of pyloric stenosis:
- compensated - the patient has a feeling of heaviness and fullness in the epigastric region, frequent sour belching, but the general condition remains satisfactory;
- subcompensated - patients complain that even a small meal causes a feeling of fullness and heaviness in the abdomen. Vomiting occurs frequently and provides temporary relief. Patients lose weight and are afraid to eat;
- decompensated – the general condition is severe or extremely severe. The food eaten no longer passes into the intestines due to complete narrowing of the pylorus. Vomiting is profuse, repeated, and occurs immediately after eating foods. Patients are dehydrated, they experience weight loss, electrolyte and pH imbalance, and muscle cramps.
Bleeding
Gastrointestinal bleeding occurs due to destruction of the vessel wall at the bottom of the ulcer (see causes of bleeding from the anus). This complication is quite common (about 15% of patients). Clinically, it manifests as coffee-ground vomiting, melena, and general signs of blood loss.
“Coffee grounds” vomiting gets its name due to the fact that blood, entering the lumen of the stomach, enters into a chemical reaction with hydrochloric acid. And in appearance it becomes brown-black with small grains.
Melena is tarry or black stool (see causes of black stool). The color of stool is also due to the interaction of blood with gastric juice. However, it should be remembered that some medications (iron supplements, activated carbon) and berries (blackberries, blueberries, black currants) can turn the stool black.
Common signs of blood loss include general pallor, decreased blood pressure, tachycardia, and shortness of breath. The skin becomes covered with sticky sweat. If the bleeding is not controlled, the person may lose too much blood and die.
Active ingredient: Levofloxacin
Trade name of the drug:
- Eleflox (Ranbaxy)
Features of the drug that are important for the patient to know about
Broad-spectrum antibiotic. In anti-Helicobacter therapy regimens, it is usually used as a “reserve drug” in cases where a person cannot tolerate other antibiotics or previous treatment for Helicobacter pylori infection has proven ineffective. When taken, nausea, vomiting, diarrhea, decreased appetite, abdominal pain, decreased blood pressure, dizziness, weakness, drowsiness and other side effects are possible. During the course of treatment with the drug, you should not sunbathe (including in a solarium). Contraindicated in epilepsy, pregnancy, breastfeeding and children under 18 years of age.
Protect your baby's stomach! Why gastritis occurs even in the smallest Read more
How to identify the disease?
The patient's complaints and medical history help the doctor suspect a peptic ulcer. However, in order to accurately diagnose the disease, therapists prescribe a number of special procedures.
Methods for detecting stomach ulcers:
- Complete blood count - Decreased number of red blood cells and hemoglobin (anemia), increased ESR
- Fibroesophagogastroduodenoscopy (FEGDS) - Using a special rubber tube with a camera (fibrogastroscope), the doctor can see with his own eyes the condition of the mucous membrane of the digestive tract. This method also allows you to perform a biopsy of the organ wall, that is, pinch off a small piece from it.
- X-ray of the stomach with contrast - The technique is currently somewhat outdated. Its essence is as follows: the patient drinks a barium contrast mixture. The radiologist then takes a series of pictures that show how the contrast moves through the mucosa. The presentation of a peptic ulcer is usually described as a “niche symptom.”
- pH-metry and 24-hour monitoring of gastric juice pH - This is an invasive and painful technique that allows you to assess how aggressive gastric juice is in relation to the mucous membrane.
Methods for identifying Helicobacter:
- Serological - Detection of antibodies in the blood to H. pylori
- Radionuclide urease breath test - Based on the release of urea by a microbe, which comes out with the air. The technique is safe; to detect Helicobacter, you only need to breathe into a special container.
- Stool test - Detection of Helicobacter antigen in stool, used to determine the effectiveness of treatment
- Rapid urease test - Performed after fibrogastroscopy. The resulting piece of mucous membrane is tested with a special indicator that detects H. pylori
Harm from self-medication
Doctors strongly do not recommend self-medication. This measure is due to the fact that:
if the patient guesses his diagnosis, then there is a very high probability of prescribing himself the wrong treatment regimen and the wrong drugs that are required;- in most cases, the patient misdiagnoses himself, hence the ineffective treatment (at best);
- drugs that the patient prescribes to himself may react with other drugs taken by patients;
- Taking the drug “blindly” can mask the symptoms of the true disease.
The main danger of such treatment is the loss of time. Even minor health problems, which with adequate treatment may go away within a few days, can develop into a real problem.
Spontaneous use of certain medications often leads to the development of complications.
Treatment of stomach ulcers
Therapy for this disease is multicomponent. It is mandatory to eradicate (destruct) Helicobacter pylori, reduce the acidity of gastric juice, eliminate unpleasant symptoms (heartburn, nausea) and prevent complications.
Antibiotic therapy
When the connection with Helicobacter pyloris peptic ulcer has been proven, treatment cannot be accomplished without the use of antibiotics. Previously, it was believed that treatment should last until the microbe completely disappeared, which was confirmed by:
- blood test for antibodies
- sowing
- urease test for FGDS
Then it turned out that not all types of Helicobacter cause the disease, and their complete destruction cannot be achieved, since when they die in the duodenum and stomach, it moves lower into the intestines, leading to inflammation and severe dysbiosis. Re-infection is also possible when using shared utensils and during the FGDS procedure, which should be performed only according to strict indications.
Today, it is advisable to carry out 1 or 2 courses of antibiotic therapy, if after the first course the bacteria are not killed, a different treatment regimen is selected, the following drugs are used:
- Macrolides (Clarithromycin)
- Semi-synthetic penicillins (Amoxicillin)
- Tetracycline
- Nitroimidazole derivatives (Metronidazole) for proven Helicobacter infection
Antisecretory drugs
- Antacids - Almagel, Maalox, sucralfate, queal. They envelop the mucous membrane, also neutralize hydrochloric acid and have an anti-inflammatory effect.
- H2-histamine receptor blockers - Ranitidine, rhinitis, famotidine, quamatel. Histamine receptor blockers interfere with the action of histamine, interact with parietal cells of the mucosa and increase the secretion of gastric juice. But they have practically ceased to be used because they cause withdrawal syndrome (when symptoms return after stopping therapy).
- Proton pump blockers - Omeprazole, omez, pantoprazole, rabeprazole, esomeprazole, lansoprazole, controloc, rabeloc, nexium (see a more complete list of duodenal ulcers). They block the H+/K+ ATPase or proton pump, thereby preventing the formation of hydrochloric acid.
- Synthetic analogs of prostaglandin E1 Misoprostol, Cytotec. Inhibits the secretion of hydrochloric acid, increases the formation of mucus and bicarbonates.
- Selective blockers of M-cholinergic receptors (pirencipin, gastrocepin) reduce the production of hydrochloric acid and pepsin. They are used as an auxiliary therapy for severe pain; side effects include dry mouth and palpitations.
Agents that increase mucosal protection
- Sucralfate (Venter) – creates a protective coating at the bottom of the ulcer
- Sodium carbenoxolone (biogastron, ventroxol, kaved-s) helps speed up the restoration of the mucous membrane.
- Colloidal bismuth subcinate - De-nol. Forms a peptide bismuth film that lines the stomach wall. In addition, bismuth ion has a bactericidal effect against Helicobacter.
- Synthetic prostaglandins (enprostil) stimulate cell restoration and mucus production.
Other drugs
- Sedatives (Tenoten, valerian), antidepressants (amitriptyline). tranquilizers (seduxen, elenium, tazepam).
- Prokinetics - Domperidone, motilium, metoclopramide, cerucal, itopride, primer. Improves the motility of the digestive tract, facilitating the passage of food into the intestines.
- Antispasmodics - Mebeverine (duspatalin), drotaverine, no-spa. Eliminate spasm of muscle cells of the stomach wall, reduce pain.
- Probiotics - Enterozermina, bifiform, linex (see list of probiotics). Prescribed for antibiotic therapy.
The course of treatment for stomach ulcers is 2-6 weeks, depending on the general condition and size of the defect.
Possible side effects of drugs
If you take certain medications incorrectly, side effects may occur. Most often they are associated with stomach disorders, such as flatulence, bloating, headaches and dizziness. Side effects can also manifest themselves in the form of allergies, for example, redness of the skin, itchy pimples, fever, cough, runny nose, etc.
Quite rarely, drugs aimed at treating gastrointestinal diseases can have an adverse reaction in the form of decreased libido, impotence, and mastopathy.
Treatment regimens
The destruction of H. pylori promotes better scarring of the ulcer. This is the first step in treating peptic ulcers. There are two main regimens of antibacterial therapy. They are prescribed step by step, that is, the first-line medications did not work, then they try the second regimen.
1st line of eradication (within a week):
- Proton pump inhibitors 20 mg twice a day.
- Semi-synthetic penicillins (Amoxicillin) 1000 mg twice a day or nitroimidazole derivatives (Metronidazole) 500 mg also twice a day.
- Macrodids (Clarithromycin) 500 mg twice a day.
In case of failure, a 2nd line of eradication is proposed (1 week):
- Proton pump inhibitors 20 mg twice a day.
- Nitroimidazole derivatives (Metronidazole) 500 mg also three times a day.
- Bismuth subcitrate (De-nol) 120 mg 4 times a day.
- Tetracyclines (Tetracycline) 0.5 g 4 times a day.
Currently, doctors are developing new methods for treating pathology. A vaccine against Helicobacter is already being tested. For better healing of the mucosal defect, cytokine preparations, trefoil peptides and growth factors are used.
For details, see Diet for stomach ulcers, menu, products.
Active ingredient: Bismuth tripotassium dicitrate
Trade name of the drug:
- De-Nol (Astellas)
- Novobismol (Pharmproekt)
- Pantoderm (ointment)
Features of the drug that are important for the patient to know about
It has antibacterial, anti-inflammatory and astringent effects. Increases the resistance of the mucous membrane of the stomach and intestines to the effects of enzymes and hydrochloric acid. Nausea, vomiting, increased bowel movements or constipation may occur during use. These effects are temporary. Contraindicated in cases of severe renal impairment, pregnancy and breastfeeding.
Nutrition of the sick
There are two main requirements for food: it must be complete and protect the mucous membrane from chemical and physical damage. It is recommended to eat 5-6 times a day, in small portions. Dishes should be finely ground or liquid, not hot or cold, boiled or steamed (see the detailed article on nutrition - what you can eat with ulcers and gastritis).
What can you eat? | What should be strictly excluded? |
|
|
Treatment with folk remedies
Fresh milk, soda, calamus root decoction, all types of nuts, pea powder and carrot juice will help relieve heartburn (see medicines for heartburn). To neutralize the hydrochloric acid contained in gastric juice, use fresh potato juice. To do this, you need to grate the root vegetable and strain the resulting mass through cheesecloth. Take half a glass of potato juice an hour before breakfast for a week.
Herbal treatment also promotes recovery. Doctors recommend infusions of fireweed, yarrow, marsh cudweed, strawberry and apple leaves, flax seeds, aspen buds, and birch chaga mushroom.
A special herbal mixture also has healing properties, which includes elecampane rhizome, chamomile flowers, yarrow, celandine, marsh cudweed, flax seed, licorice root, rose hips. All herbs need to be washed well, dried and poured with boiling water. It is advisable to take a tablespoon 10 minutes before meals. A positive result will not be long in coming.
Author:
Selezneva Valentina Anatolyevna physician-therapist
Ganglioblockers
Ganglion blockers help reduce the secretion of digestive juice, while simultaneously relaxing the smooth muscles of the stomach and gastrointestinal tract. This combination of effects provides functional rest to the ulcerated mucosa. The following medications are prescribed.
Benzohexonium
Blocks the transmission of signals from one major nerve ganglion to another. Used to eliminate the pathological symptoms of ulcers.
Dimecoline
Relieves symptoms of peptic ulcer. Has antispasmodic properties.
Kamphonium
Has powerful analgesic properties. Used to treat patients in whom the use of drugs that tonic the vascular system is prohibited. Allowed for hypertensive patients.
Quateron
It has the ability to temporarily disrupt the transmission of nerve impulses, which helps relieve pain. Additionally, treatment can be carried out with medications such as:
- Sucralfate. Forms a protective film on the surface of the mucosa, which eliminates the negative impact of aggressive digestive enzymes on damaged areas. The peculiarity of the product is that it exclusively covers the area of ulceration, without interfering with the flow of digestive processes.
- Biogastrol. Herbal medicine. The main active ingredient is licorice root extract. Its intake promotes active tissue regeneration over the entire surface of the mucous membrane of the digestive tract.
It is recommended to treat exacerbations of ulcers under medical supervision. Independent selection of medications is unacceptable, since unreasonable use of medications can cause a deterioration in the general condition.
( 1 ratings, average: 5.00 out of 5)