Thyroiditis is an inflammatory disease of the thyroid gland. In an acute condition, abscess formation is possible. Characteristic symptoms of thyroiditis in the early stages are a feeling of squeezing and pain in the neck, hoarseness. Progression of the disease causes dysfunction of the gland. The prognosis with timely diagnosis and treatment is favorable. Thyroiditis is an inflammatory disease of the thyroid gland. In an acute condition, abscess formation is possible. Characteristic symptoms of thyroiditis in the early stages are a feeling of squeezing and pain in the neck, hoarseness. Progression of the disease causes dysfunction of the gland. The prognosis with timely diagnosis and treatment is favorable.
Causes of thyroiditis
The reasons for the development of thyroiditis directly depend on the etiological factors that trigger the process of inflammation of the thyroid tissue. Depending on the types of thyroiditis, it is possible to determine the cause that influenced the appearance of this pathology:
- acute purulent thyroiditis: quite rare. Develops due to infection through the lymphogenous or hematogenous route;
- subacute thyroiditis: has a second name - de Quervain's thyroiditis. It is assumed that the etiology of this disease is related to viral lesions of the thyroid gland (measles, mumps). During the development of subacute thyroiditis, a secondary autoimmune process occurs, the antigen to which is thyroglobulin, which is evacuated into the blood due to a violation of the integrity of the main membrane of the thyroid follicles. The destruction process causes an increase in the level of thyroid hormones in the blood, which provokes the development of signs of thyrotoxicosis. The incidence rate of subacute thyroiditis is 1-2% of all thyroid pathologies. This disease affects women more often;
- chronic fibrous thyroiditis, in the literature its name is often found by the author - Riedel's goiter. The etiology of the disease is currently unknown. The gradation of this pathology is based on the development of a chronic inflammatory process in the thyroid gland, the primary spread of connective tissue, its growth into the capsule of the thyroid gland, nearby nerves, muscles and blood vessels. As a rule, the proliferation of connective tissue is local in nature, but in some cases, total damage to the thyroid gland is possible, which is accompanied by the development of hypothyroidism. Chronic fibrous thyroiditis occurs in 0.05% of cases of all thyroid diseases;
- autoimmune thyroiditis, also known as Hashimoto's goiter. The cause of the development of the disease is dysfunction in the immunological control system, which is congenital in nature. Therefore, there are very frequent cases of the development of this pathology in several generations of the same family, sometimes it is combined with other autoimmune diseases (rheumatoid arthritis, ulcerative colitis, myasthenia gravis). This type of thyroiditis, in turn, is divided into two forms: hypertrophic, which occurs at the beginning of the development of the disease, and atrophic, characteristic of the final stage of the pathology. The incidence of autoimmune thyroiditis is 5% of all pathological changes in the thyroid gland.
Mechanism of development and progression of AIT
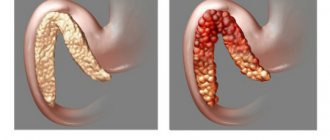
AIT occurs due to dysfunction of the immune system. Instead of protecting the thyroid tissue, immune cells attack it. The activity of these cells can lead to hypothyroidism (insufficient activity of the gland), goiter (increase in size), or both conditions at once. Ultimately, the autoimmune process can even destroy the entire thyroid gland if the disease is not detected or treated.
With AIT, a large number of immune cells (lymphocytes) accumulate in the thyroid gland, which leads to its damage. Lymphocytes produce immune proteins (antibodies) that attack and destroy gland cells.
When too many cells are damaged or die, the thyroid gland can no longer produce enough hormones to regulate body functions. This deficiency underlies the symptoms of thyroiditis.
The destruction process is very slow, which is why many people with AIT do not have any noticeable symptoms.
Acute purulent form
The acute purulent form of thyroiditis is characterized by infiltrative changes in the thyroid gland with the subsequent development of a purulent process (abscess formation). Purulent melting significantly affects the secretory functions of the thyroid gland, however, in some cases it affects a small part of the gland tissue and does not provoke a sharp dysfunction of hormonal secretion.
The development of purulent thyroiditis occurs quite quickly with an increase in the patient’s body temperature to 400C and chills. Subjectively, the patient feels sharp pain on the front surface of the neck, radiating to the jaw, back of the head, ears, tongue, which intensifies with swallowing, coughing and head movements. There is a rapid increase in symptoms of intoxication: fatigue, general weakness, aches in the joints and muscles appear, tachycardia and headache increase. Often the patient's condition is assessed as serious.
On palpation, sharp pain, diffuse or local enlargement of the thyroid gland is determined; the consistency of the gland can be dense (at the infiltration stage) and softened (at the stage of abscess formation). There is also soreness and enlargement of the cervical lymph nodes, local hyperthermia and redness of the skin of the neck.
Characteristic manifestations
During the euthyroid and subclinical phases, there are no signs of inflammation of the gland. The clinical picture unfolds in the thyrotoxic phase with a sharp increase in the level of T3 and T4:
- hand tremors;
- irritability;
- anxiety;
- insomnia;
- interruptions in heart function;
- bulging eyes;
- excessive sweating;
- cardiopalmus;
- temperature increase;
- sudden change of mood.
In the typical course of CAIT, the thyrotoxic phase is replaced by a hypothyroid phase, which is characterized by a slowdown in metabolism.
As glandular tissue atrophies, the content of iodine-containing hormones decreases. First, thyrotoxicosis is replaced by a short euthyroid and then by a hypothyroid phase. A deficiency of T3 and T4 in the blood is indicated by:
- dry skin;
- lethargy;
- weight gain;
- sore throat;
- puffiness of the face;
- cold intolerance;
- fast fatiguability;
- memory impairment;
- hair loss.
Clinical forms of HAIT:
- Latent. There are no signs of thyroiditis yet. Violations are detected only in the laboratory. No compactions or nodular neoplasms are found in the gland.
- Hypertrophic. Thyroiditis is manifested by enlargement of the gland. Symptoms of hyper- or hypothyroidism are mild. In some patients, uniform or focal hypertrophy of the thyroid gland is detected - diffuse or nodular goiter. As thyrocytes become damaged, the symptoms of hypothyroidism increase.
- Atrophic. Due to the destruction of thyroid tissue, the iron decreases in volume. If left untreated, it is accompanied by mucous (myxedematous) edema.
Signs of postpartum thyroiditis appear 3.5 months after delivery. Women complain of weight loss, chronic fatigue, sweating, feeling hot and tachycardia. By the end of 4 months, the symptoms of hypothyroidism increase, which often accompanies postpartum depression.
Cytokine-induced and painless thyroiditis are characterized by a mild course. In 87% of patients, signs of thyrotoxicosis and hypothyroidism are mild.
Subacute form
The process of development of subacute thyroiditis may have signs of pronounced inflammation: an increase in the patient’s body temperature to subfebrile levels (380C and above), a constant increase in symptoms of general intoxication, pain in the anterior surface of the neck, moving to the back of the head, ear, jaw. But most often the disease begins with symptoms of general malaise, a feeling of discomfort and moderate pain in the neck, swelling of the thyroid tissue. The patient feels increased pain while chewing solid food. On examination, an enlargement of one of the lobes of the thyroid gland is often detected. There is no enlargement of the near-regional lymph nodes.
In half of the cases, subacute thyroiditis is associated with the development of moderate or mild thyrotoxicosis. The patient complains of tremors of the limbs, palpitations, increased sweating, insomnia, weakness, joint pain, heat intolerance, and nervousness.
Hypersecretion of thyroid hormones (triiodothyronine and thyroxine) has an inhibitory effect on the hypothalamus and reduces the production of the regulatory hormone - thyrotropin. Deficiency of thyrotropin provokes a decrease in the functions of the undamaged part of the thyroid gland, which causes the transition of the disease to the second phase and the development of hypothyroidism. Typically, hypothyroidism does not last long and disappears as the inflammatory process subsides.
The role of the thyroid gland in the body
The thyroid gland is a butterfly-shaped gland located in front of the trachea and just below the larynx in the neck.
It consists of two lobes connected by a band of tissue called the isthmus. The main role of the thyroid gland is to regulate metabolism through the action of the hormones it produces.
The pituitary gland and hypothalamus (brain structures) control the thyroid gland. When thyroid hormone levels drop too low, the hypothalamus secretes a releasing hormone, thyroid-stimulating hormone (TSH), which alerts the pituitary gland to produce thyroid-stimulating hormone (TRH). The thyroid gland reacts to this chain of events by producing more hormones.
The two main hormones produced and secreted by the thyroid gland are T3 (triiodothyronine) and T4 (thyroxine) . A working thyroid gland typically produces about 80% T4 and about 20% T3, although T3 is the stronger of the pair.
Chronic fibrous thyroiditis
Chronic fibrous thyroiditis may not have clinical manifestations for a long time. The earliest symptom of this pathology is usually a feeling of a “lump” in the throat and difficulty swallowing. The advanced stage of the disease is characterized by disturbances in speech, swallowing, breathing, choking while eating, and hoarseness of the voice.
Palpation reveals a pronounced uneven enlargement of the thyroid gland (tuberosity), its inactivity during swallowing, compactness, painlessness, and a dense “woody” structure. Changes in the affected gland are usually diffuse in nature and are associated with a decrease in its functionality and the development of hypothyroidism.
Pressure on adjacent tissues is expressed by compression syndrome, which is manifested by blurred vision, headaches, difficulty swallowing, tinnitus, breathing problems and pulsation of the cervical vessels.
There are also specific thyroiditis, which include inflammatory processes and structural changes in the thyroid tissue of the thyroid gland with its mycotic, tuberculous and syphilitic lesions. Basically, specific thyroiditis is chronic, but if involved, the process of secondary infection can become acute.
Diagnostic procedures to confirm the diagnosis of AIT
In addition to a physical examination and taking into account individual symptoms, the doctor will use one or more laboratory tests to diagnose AIT.
Blood test for TSH
The hormone that stimulates the thyroid gland is not produced by the thyroid gland, but is produced by the pituitary gland in the brain. When the pituitary gland detects even the slightest decrease in the production of thyroid hormones, it secretes more TSH to stimulate their production.
The purpose of the test is to determine whether TSH levels are within normal limits. In hypothyroidism due to AIT and in primary hypothyroidism for any reason, hormone levels invariably increase.
Higher TSH levels mean the brain thinks the thyroid gland is not producing enough hormones and needs stimulation to produce more.
TSH levels are also elevated in subclinical hypothyroidism and are usually the initial laboratory sign found when the pituitary gland is trying to increase hormone production. T4 usually remains within reference ranges in subclinical hypothyroidism. TSH levels may also be elevated during the recovery phase of euthyroidism.
Free T4 blood test
A free T4 test is usually necessary to correctly interpret TSH levels in some clinical settings. A low total or free T4 level in the presence of an elevated TSH level further confirms the diagnosis of primary hypothyroidism.
Test for antibodies to thyroid gland
The presence of thyroid autoantibodies, usually antibodies against TPO (thyroid peroxidase), as well as against thyroglobulin (precursor of thyroid hormones), determines the cause of hypothyroidism as AIT. However, 10-15% of patients with AIT may test negative for antibodies.
Ultrasonography
Ultrasound is not usually required to diagnose AIT, but it can help identify signs of the disease. Ultrasound helps evaluate the size of the thyroid gland, texture and, most importantly, determine the presence of nodules. The study allows you to confirm the presence of a thyroid nodule, determine its structure (solid or cystic), and also identify signs indicating malignancy (fuzzy edges, poorly defined halo, microcalcification and increased blood supply on Doppler examination).
Diagnosis of thyroiditis
Diagnosis of thyroiditis begins with collecting anamnesis, examination, palpation examination of the patient and performing laboratory tests.
All types of thyroiditis are characterized by changes in clinical blood parameters, which indicate the presence of an inflammatory process in the body and are expressed by an increase in ESR, neutrophilic leukocytosis, and a shift in the leukocyte formula to the left.
In the acute form of thyroiditis, the level of thyroid hormones in the blood does not change. The onset of subacute thyroiditis is characterized by an increase in the concentration of hormones, then during the process of treatment and recovery there is a decrease in the amount of hormones.
In case of autoimmune and fibrous thyroiditis, a morphological analysis of a tissue sample of the altered thyroid gland is indicated, the collection of which is performed through a biopsy. This study makes it possible to exclude the malignancy of the process.
If subacute thyroiditis is suspected, the patient is given a Krail test, which consists of taking 30-40 mg/day of prednisolone, which in this disease significantly improves the patient’s condition (after 24-72 hours).
The main methods for diagnosing thyroiditis include ultrasound examination of the thyroid gland.
In order to clarify the size and nature of the lesion, scintiography of the thyroid gland is performed. In fibrous thyroiditis, scintiography makes it possible to determine the size and altered contours of the thyroid gland.
Diet
There are no special diets for patients with thyroiditis. To restore normal functioning of the thyroid gland, you need to eat 3-4 times a day. A lack of calories will have a bad effect on the patient's condition.
When the functions of the thyroid gland are disrupted, disruptions in metabolism occur, causing the body to be poisoned. To alleviate the condition, include as many vegetables and fruits as possible in the diet. They contain fiber, which binds and removes toxins.
Important for thyroiditis are polyunsaturated fatty acids contained in fish and fish oil.
Carbohydrates should be consumed in the body through cereals, bread, pastries and pasta. Following a strict diet is prohibited. Proper nutrition for thyroiditis involves eating normal amounts of meat, dairy products and eggs.
Since thyroiditis can trigger osteoporosis, it is necessary to eat foods rich in calcium. Drink at least 2 liters of liquid per day.
Complications of thyroiditis
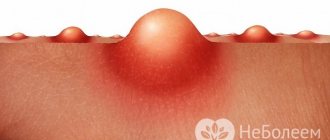
A complication of acute thyroiditis can be abscess formation and perforation of the abscess, at best outward. If pus gets into the surrounding tissues, it can reach the pericardial space, which is a serious complication of thyroiditis. Also, the progression of the purulent process in the tissues of the neck can lead to damage to blood vessels, infection of the meninges and brain tissue, and in the most severe cases, provoke sepsis (general blood poisoning with infection). Therefore, timely therapeutic measures are very important.
If left untreated for subacute thyroiditis, damage to a sufficiently large number of thyroid tissues may develop, which will ultimately lead to the development of irreversible thyroid failure.
Kinds
There are several forms of thyroiditis, differing in the nature of the clinical picture and the speed of development.
Acute inflammation of the thyroid gland occurs when an infectious agent enters the blood and lymph from nearby organs.
This is observed in chronic and acute tonsillitis and pneumonia. The causative agents of the infection are staphylococci and streptococci. The aseptic form of inflammation occurs due to injuries, exposure to radiation, and hemorrhage into tissue. In this case, pathogenic microorganisms are not detected.
Treatment of thyroiditis
Treatment of mild forms of thyroiditis involves dynamic monitoring of the patient, the prescription of symptomatic therapy and non-steroidal anti-inflammatory drugs to relieve pain. In case of development of severe diffuse inflammation, the administration of steroid hormones is indicated.
Acute purulent thyroiditis is an indication for immediate hospitalization in a surgical department. Such patients are prescribed a course of antibiotic therapy, antihistamines, vitamin therapy, and infusions of a large number of detoxification drugs. If an abscess has formed, the patient undergoes surgical treatment, during which the abscess is opened and drained.
Treatment of chronic and subacute thyroiditis involves the administration of thyroid hormones. If a complication develops in the form of compression syndrome, surgical intervention is sought.
In the absence of a positive reaction to hormone treatment (replacement therapy for 3-4 months) in conditions of chronic autoimmune thyroiditis, the patient is prescribed corticosteroids for 2-3 months. This is followed by dynamic observation by an endocrinologist.
The principle of treatment of specific thyroiditis is therapeutic measures aimed at eliminating the underlying disease.
AIT and reproductive function
Too low levels of thyroid hormones can affect the hormonal mechanisms that regulate the menstrual cycle and cause ovulation. This can lead to infertility, which affects up to 50% of women with AIT.
Even with proper treatment for hypothyroidism, there is no guarantee that fertility can be fully restored in women seriously affected by AIT.
If hypothyroidism is not treated during pregnancy, it can lead to preeclampsia (high blood pressure during pregnancy), miscarriage, premature birth, stillbirth, and other congenital problems in the baby.
Medicines containing thyroid hormone used to treat the problem are usually safe during pregnancy.
Prevention of thyroiditis
There are no specific preventive measures to prevent the development of thyroiditis. But an important role in this regard is played by the prevention of viral and infectious diseases, which involves vitamin therapy, hardening, a healthy diet and the elimination of bad habits. It is also necessary to promptly sanitize foci of chronic infections: treatment of otitis media, caries, pneumonia, sinusitis, tonsillitis, etc.
At the slightest suspicion of the disease, you should immediately contact an endocrinologist. Clear and timely implementation of the doctor’s recommendations will significantly increase the chances of success.
Etiology of AIT
Variations in several genes have been studied as possible risk factors for the development of AIT. Some of these genes are part of the human leukocyte antigen (HLA) complex, which helps the immune system distinguish body proteins from foreign proteins. Other genes that are associated with AIT help regulate the immune system or are involved in normal thyroid function.
Most of the genetic variations found are thought to have little effect on the overall risk of developing the disease.
Other, non-genetic factors also play a role in the occurrence of AIT. These factors promote the development of conditions that increase risk, although the mechanism of action is unclear.
Potential precipitating factors are:
- changes in the level of sex hormones (especially in women);
- viral infections;
- some medications;
- exposure to ionizing radiation;
- Excessive iodine intake.
The inheritance pattern of AIT is unclear, as many genetic and environmental factors are involved. But the condition can run in families, and having a close relative with AIT or another autoimmune disorder likely increases a person's risk of developing the condition.