Author's rating
Author of the article
Shutofedova Ksenia Yurievna
General practitioner
Articles written
578
about the author
Acute nasopharyngitis is an inflammatory lesion of the mucous membranes of the pharyngeal and nasal cavities, which is often diagnosed in preschool children. It is a complication of a prolonged runny nose. If left untreated, the disease becomes chronic and will worsen under the influence of the slightest adverse factors.
Nature of origin
Among adults, this form of rhinitis often appears after poorly treated treatment or an advanced stage of acute respiratory disease, which most often occurs in the autumn-winter season or early spring. Rhinopharyngitis can appear in the area of the nasopharynx, tonsils or in the lymphatic ring as a complication in people with weak immunity: in old age, with long-term use of antibiotics or with chronic inflammation of the nasopharynx.
According to the nature of origin (etiology), inflammation can be caused by:
- infection (viruses, bacteria or fungi);
- an allergic reaction of the body, when the inflammatory process begins in the presence of negative factors: animal hair, mold, dust, pollen, household chemicals, etc.
The main cause of nasopharyngitis is always an infection (ARVI or influenza), its pathogens attack the back wall of the mucous membrane. However, other factors also have an impact:
- severe hypothermia of the body;
- poor blood supply to the tissues of the nasopharynx;
- exposure to chemicals;
- the influence of allergenic factors in people with hypersensitivity;
- the body's reaction to a strong smell or cold air.
General description of the disease
Rhinopharyngitis occurs in both acute and chronic forms. The disease is diagnosed quite often. In almost 80% of cases it occurs when viruses enter the body. It is one of the manifestations of respiratory viral infections of the respiratory tract (ARVI) or influenza. Most often, people suffer from nasopharyngitis in the autumn-winter period, when the body's protective functions are weakened.
It is observed in people of any age, but most often affects children, which is due to age-related underdevelopment of the ENT organs. According to medical statistics, children get nasopharyngitis 4 to 6 times a year. The favorite age of the disease is up to 10 years. In adolescents, the incidence rate is noticeably lower.
In most cases, the pathology does not occur in isolation, but affects both the nasal cavity and the pharyngeal mucosa. The chronic form of rhinopharyngitis is much less common and difficult to treat. The transition to this stage occurs when acute rhinitis and pharyngitis are not fully treated.
Signs of the disease
The first symptoms of posterior rhinitis are difficult to recognize on your own due to symptoms similar to the classic cold in acute form.
The main signs of rhinopharyngitis:
- dryness and burning sensation on the nasopharyngeal mucosa;
- painful sensations and sore throat;
- when lying down, there are difficulties with normal breathing through the nose due to swelling of the mucous membrane;
- thick, mucopurulent nasal discharge, congestion;
- when mucus drains down the back wall of the nasopharynx, a cough appears;
- standard respiratory symptoms: lacrimation, sneezing, inflammation of the palate;
- dry crusts in the nose, which may cause bleeding when removed;
- fever is observed less often in adults than in children;
- "nasal" voice;
- pain when palpating the cervical lymph nodes;
- poor general health: drowsiness, headache, weakness, etc.
If the patient does not reverse the changes in the body in time and does not begin treatment, then there may be deterioration in hearing, sense of smell, cough and ear pain.
Necessary examinations
To confirm the diagnosis, you will need to consult an otolaryngologist. The specialist interviews the patient about characteristic complaints.
Then examines the oral and nasal cavity with instruments or using endoscopic equipment.
After the examination, additional studies may be prescribed:
- X-ray of the paranasal sinuses to exclude sinusitis;
- a general blood test to confirm the inflammatory process and its severity;
- allergy tests if an allergic nature of the disease is suspected;
- sowing for flora and sensitivity. To clarify the pathogen and its response to antibiotics.
After establishing the diagnosis and its cause, the doctor prescribes the necessary treatment. At the same time, factors that contribute to the maintenance of the inflammatory process are eliminated.
Differentiation with other pathologies
What diseases should be used in the differential diagnosis of rhinopharyngitis:
- Flu. A viral infection that begins with fever, runny nose, and sore throat. Later, symptoms of general intoxication, weakness, and cough appear. Often causes serious complications on the heart, kidneys and other organs.
- Diphtheria. An infectious pathology, the development of which is caused by the bacterium diphtheria bacillus. Thanks to routine vaccinations (DTP), the disease is rare. When infected, it affects the mucous membranes of the nose and pharynx with the formation of dirty gray films. In childhood, it can cause the development of false croup and suffocation.
- Angina. Infectious and inflammatory disease of the lymphoid apparatus of the pharynx. It manifests itself as a sharp pain in the throat, a rise in temperature and the appearance of plaque on the tonsils. Unlike nasopharyngitis, the nasal mucosa is not affected, but in children, nearby adenoids may become inflamed.
Types of rhinitis
There are 2 main forms of posterior rhinitis, the symptoms and treatment of which depend on the intensity of the pathology:
- acute - manifests itself sharply, in adults it occurs more easily than in children, lasting an average of 5-7 days;
- chronic - can last several months, the symptoms are less pronounced.
In the chronic form, complications may develop and the disease may progress to other types:
- subatrophic - the mucous membrane dries out, which causes its thinning;
- atrophic - destruction of the nasopharyngeal mucosa occurs; in severe cases, damage to cartilage and bone tissues is possible.
Posterior rhinitis in adults differs in the nature of the inflammatory process and is divided into:
- catarrhal, in which copious discharge of clear mucus occurs from the nose;
- purulent, when the snot has a yellow or yellow-green tint.
Peculiarities
Different forms of rhinitis can affect the patient’s well-being in different ways:
- In the acute phase of the disease, a sharp jump in temperature is possible, and in the chronic phase it can be normal, but during an exacerbation it can fluctuate between +37.0…+37.5°C
- Discharge from the nasopharynx is initially clear, accompanied by swelling and redness of the nose, and difficulty breathing. When the mucus secreted becomes thick and yellow-green in color, this indicates a chronic form of rhinitis. When dry crusts form on the lining of the nasal cavity, the sense of smell may decrease; after rinsing, breathing is restored.
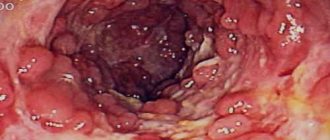
- Pain in the throat, especially when swallowing, is often acute; in the throat, upon examination, you can notice redness of the walls and swelling of the tonsils, often with the presence of purulent plaque. In the chronic form, there is a soreness in the throat, causing a slight cough. In advanced cases, in the absence or improper treatment of rhinitis, granulosa areas form on the back wall of the throat.
- The cough is unproductive, attacks of which often worsen at night, and occasionally end in vomiting. In the chronic form, separation of mucopurulent sputum is observed, which is accompanied by chest pain.
- With a bacterial infection, a symptomatic manifestation is possible in the form of an unpleasant odor of discharge and mucus; a cough occurs in an attack in the morning, after the patient wakes up. The reason for this is the flow of secretions down the back wall of the nasopharynx, which causes irritation of the cough receptors. Immediately after expectoration, relief occurs.
Preventive actions
To avoid infection with nasopharyngitis, you need to carefully monitor your health. Carry out hygienic procedures to cleanse your nose regularly. The above-mentioned medications are suitable for this. You also need to humidify the air in the room you are in. Do not allow the mucous membranes of the nasal passages and larynx to dry out, drink more clean water. Don't forget about nutrition. The benefits of fruits and vegetables are undeniable. Through these products you can get a lot of vitamins and beneficial microelements. Create your own routine. Wake up at the same time, walk more in the fresh air. This will help prevent a runny nose and its consequences - nasopharyngitis.
During epidemics, try not to visit crowded places. If forced contact with an infected person, use antiviral agents for prevention purposes. However, this topic should first be discussed with your doctor.
If you feel the onset of the disease, then you should not try to carry it on your feet. Be sure to use medications and stay in bed. Sport also increases the body's resistance, but exercise should be moderate. At the first symptoms of the disease, do not try to eliminate it yourself. Remember that timely contact with a specialist is a guarantee of a quick recovery. Do not be ill!
How to treat
The symptoms of nasopharyngitis are very similar to the symptoms of other colds and infectious diseases: sore throat, tonsillitis, mononucleosis. However, the treatment of such diseases is very different, so for a correct diagnosis of the disease it is necessary to consult your doctor. Self-therapy can be erroneous and contribute to the deterioration of the condition, the transition to a chronic form of nasopharyngitis.
Treatment methods for posterior rhinitis include medications and herbal decoctions and folk remedies.
It is also important to distinguish the allergic form of nasopharyngitis, which is often seasonal or manifests itself sharply under the influence of negative factors. Symptoms of the allergic form:
- nasopharyngeal congestion, watery and profuse discharge;
- frequent sneezing and itchy nose;
- sore throat, hoarseness.
Exacerbation of allergic rhinitis can lead to angioedema or suffocation, which requires emergency medical attention.
Symptoms of nasopharyngitis
The acute form of nasopharyngitis develops against the background of existing ARVI. The incubation period of the disease ranges from 1 to 4 days. The first signs of the disease are weakness, general malaise, headache, fever. Next, a feeling of itching in the nose appears, accompanied by sneezing. The nose is stuffy, there may be liquid mucous discharge.
Signs indicating inflammation of the pharynx: a feeling of dryness, soreness and rawness, coughing without mucous discharge, sore throat. The disease is characterized by the reflection of pain in the area of the ear or lower jaw. When examining the pharynx, you can see redness and swelling in the areas of the back of the pharynx, tonsils and palatine arches. The degree of redness is determined by the severity of the inflammatory process and can vary from mild to bright red inflammation with a purulent coating. Simultaneously with these phenomena, enlargement of regional lymph nodes is possible.
Symptoms of nasopharyngitis have a similar clinical picture to sore throat and diphtheria, which requires differential diagnosis of these ailments. Only a doctor can determine exactly what pathogen caused the inflammation by conducting a bacteriological culture of the plaque present on the mucous membrane of the pharynx.
Do not forget that the symptoms of acute nasopharyngitis may be the first symptoms of measles, rubella or scarlet fever. This is relevant not only in childhood, but also for adults who have not previously suffered from these infections.
Treatment of acute forms of the disease
When diagnosing acute nasopharyngitis, the doctor prescribes complex therapy lasting about 10 days. In this case, the causes of the disease, its form and possible concomitant pathologies are taken into account.
Drug treatment is prescribed to cleanse the nasopharynx of mucus and secretions and destroy pathogenic bacteria that cause the disease. In this case, local and general drugs and physiotherapeutic procedures are used.
Topical medications for the treatment of the posterior wall for rhinitis in adults:
- solutions with antiseptic action: Furacilin, Chlorhexidine, Chlorphyllipt;
- lozenges that suppress the growth of bacteria in the throat and anesthetize: Strepsils, Neo-Angin, Lisobakt, Septolete, etc.
For a runny nose, posterior rhinitis can be treated in both adults and children using nasal rinses and drops, for which the following is used:
- isotonic solutions with sea water or sodium chloride: No-Sol, Aquamaris, Humer;
- inhalations with medicinal solutions and herbal decoctions;
- vasoconstrictor drops or sprays to ease breathing (no more than 2 times a day for 3-4 days);
- preparations with oxymetazoline: Nazol and Nazol Advance (contains eucalyptus and heel oil), Nazivin;
- oil-based nasal drops that help avoid drying out the nasal tissues: Pinosol, etc.
If necessary, the doctor prescribes antiviral medications, vitamins, antibiotics and immunity boosters. To remove toxins and improve general well-being, the patient is recommended to drink plenty of fluids: compotes, juices, still mineral water, decoctions of rose hips, raspberries, linden, etc.
Treatment of rhinopharyngitis in children
If your baby is ill, to make the disease easier, do not neglect the advice of the famous pediatrician Komarovsky. He believes that on such days the baby needs:
- Maintaining the room temperature no more than 20 degrees;
- Mandatory ventilation, 2-3 times a day and air humidification;
- Maintaining bed rest;
- Drink plenty of fluids (natural fruit drinks, jelly, vitamin teas);
- Carrying out daily wet cleaning using disinfectants.
Under no circumstances treat the baby yourself; consult a doctor. Children are usually treated on an outpatient basis. But if inpatient therapy is recommended, you should not refuse it.
Treatment of the chronic form
In the chronic course of the disease, destructive changes (hypertrophy or atrophy) and disruption of local immunity occur on the surface of the mucosa, as a result of which the body itself cannot cope with the negative effects of viruses and bacteria. Therefore, immunostimulants are added to the treatment regimen for posterior rhinitis in adults: tinctures of echinacea or eleutherrococcus (Immunal), complexes of multivitamins and microelements.
For instillation into the nose, the doctor recommends using drops with essential oils or silver components: Collargol, Protargol, Pinosol, Evkazolin. These medications reduce the concentration of viruses and bacteria in the nasal cavity, and when flowing down the back wall, they form a protective film that helps restore the mucous membrane and prevents the proliferation of infections.
In advanced forms of nasopharyngitis, antibiotics from the aminopenicillin or cephalosporin groups are prescribed, which the otolaryngologist selects after bacteriological culture of nasal mucus.
Diagnostics
Diagnosis of the disease begins with rhinoscopy - an external examination of the nasal cavity and pharynx. In this case, redness and swelling of the mucous membranes will be observed. In the chronic course, signs of atrophy and hypertrophy are observed.
Next, a general laboratory blood test is prescribed, which determines the indicators of ESR and leukocytes. In addition, a swab from the nose and throat may need to be examined to determine the type of pathogen (PCR).
If a diagnosis of “chronic nasopharyngitis” is made, or the disease is complicated by ENT pathologies, then the following examinations are prescribed:
- X-ray of the paranasal sinuses and chest organs;
- endoscopy;
- CT scan of the paranasal sinuses.
Allergic rhinopharyngitis requires an allergy test to identify the irritant.
Physiotherapy
During the recovery period or after an exacerbation of nasopharyngitis, physiotherapeutic procedures are recommended:
- instillation (pouring a solution of drugs into the nasopharynx);
- inhalation through a nebulizer or thermal;
- UV rays (possibly during exacerbation);
- laser and cryotherapy.
When treating nasopharyngitis in adults, the attending physician also recommends general strengthening measures: playing sports, hardening. Nutrition correction is also necessary: remove spicy, salty, smoked foods, chocolate, coffee, citrus fruits (excluding lemons), and spices from the diet. Such products are allergens, irritate the nasopharyngeal mucosa and interfere with the relief of inflammation and recovery.
Drug therapy
The need for drug treatment for nasopharyngitis will disappear if you follow these recommendations.
- The temperature in the room should be between 18-22 ͦC. It is unacceptable for the patient to be in a hot room. This will lead to drying out of the mucous membranes, increasing the viscosity of mucus and difficulties with its removal. In addition, keeping a patient in a hot room will worsen his condition and reduce the chances of a quick recovery.
- The same applies to indoor humidity. It should be within 50-60%. During the heating season, it is recommended to use electric humidifiers.
- Ventilation of the room.
- Avoiding loud conversations and shouting.
- Regular wet cleaning.
In addition, the patient should drink more water. An ideal option for nasal diseases and colds is rosehip decoction, warm tea with lemon. Be sure to include foods rich in vitamin C in your diet. It helps strengthen the immune system and, as a result, prevent the development of infectious diseases. Most ascorbic acid is found in:
- black currant;
- bell pepper;
- parsley
During illness, it is recommended to remain in bed.
Medicines used for nasopharyngitis:
- Aerosols based on sea water - products wash the nasal passages up to 6 times a day. This will moisturize the mucous membrane, remove swelling, and restore nasal breathing. You can buy a saline solution at a pharmacy (Aquamaris, Humer, Dolphin) or prepare it yourself (half a teaspoon of salt per glass of warm water). They can also be used by expectant mothers and children.
- Vasoconstrictors. They quickly relieve swelling, reduce the amount of mucus produced, and restore nasal breathing. They are not medicinal products, they are used only to eliminate a runny nose. In addition, using drops for more than 5 days can lead to chronic swelling and drying out of the mucous membrane. You can buy Nazivin, Noxprey, Galazolin, Rinozolin at the pharmacy. For children, drugs are produced with a lower content of the active ingredient. Pregnant women are allowed: Tizin, Vibrocil, Ximelin.
- For allergic rhinopharyngitis, antihistamines are prescribed - Suprastin, Zyrtec, Cetrin, etc.
- Drops based on vegetable oils - Pinosol - will help moisturize the nasal cavity and facilitate the process of removing mucus.
- For swelling and sore throat, use Antiangin, Grammidin. For children - Tantum Verde, Hexoral in the form of a solution. During pregnancy, it is recommended to treat the throat walls with collargol or a 5% solution of tannin-glycerol and use Ingalipt or Tantum-Verde for irrigation.
- For gargling, antiseptics are used - Chlorhexidine, Miramistin, Furacilin solution. The same drugs can be used for infectious processes developing in the oral cavity. You can also use the products during pregnancy. Be sure to read the instructions, as some of them must be diluted with water so as not to burn the mucous membrane. Young children are not recommended to gargle with antiseptics due to the risk of ingestion.
- At elevated temperatures and heat, it is recommended to take Ibuprofen and Paracetamol. For children and pregnant women - Nurofen, Panadol.
- If the culprit of nasopharyngitis is a viral infection, then the doctor may prescribe antiviral drugs - Cycloferon, Arbidol, Toff Plus, Anaferon. Pregnant women can use Acyclovir. For children, Tsitovir and Viferon are prescribed in the form of rectal suppositories.
- For bacterial infections, extended-spectrum antibiotics (Erythromycin) are prescribed.
For chronic nasopharyngitis and a protracted form of the disease, physiotherapy is prescribed - electrophoresis with drugs, UHF, magnetic therapy, mud applications.
The inflammatory process in the nasopharynx is nasopharyngitis. The acute form of the disease is especially dangerous, which can lead to complications and, if left untreated, become chronic. To avoid this, it is necessary to start treatment on time.
Traditional methods
The most commonly used home remedies to help relieve sore throat are gargles. To rinse the nose, it is recommended to use a special kettle (Dolphin or Aquamaris), when the solution is injected into one nostril under slight pressure, and it comes out of the other.
Treatment of rhinitis with home methods and traditional folk remedies is carried out according to the following recipes:
- inhalations with herbs and oils: 2-3 drops added to boiled water;
- decoction of medicinal herbs: sage, chamomile, thyme;
- instilling honey solution into the nose (three times a day), beetroot, cabbage juice, Kalanchoe (no more than 5 times a day) helps not only to clear the nasal passages, but also improve immunity due to the content of vitamin C, which promotes tissue restoration;
- soda solution for rinsing: 1 tsp. baking soda per 0.5 liters of warm water, it is better to put ½ tsp. sea salt, which will help relieve inflammation and moisturize the mucous membrane of the oropharynx, remove accumulated mucus;
- to soften and moisturize the nasal mucosa, use drops with essential oils: tea tree (3 drops), eucalyptus (2), geranium (1), mint, menthol, etc., which are diluted in 1 tsp. any vegetable oil (olive, sunflower);
- tinctures for gargling: propolis, eucalyptus, Rotokan.
In the room where the patient is located, it is recommended to maintain high air humidity and ventilate more often. This will help avoid drying out the nasopharyngeal mucosa.
Are antibiotics allowed for nasopharyngitis?
Antibiotics for nasopharyngitis are allowed if the disease is bacterial or accompanied by complications. Possible complications due to nasopharyngitis are pneumonia, bronchitis, sinusitis. In this case, it is advisable to prescribe antibiotics of the penicillin series, cephalosporins, and macrolides.
The best antibiotics used in the treatment of nasopharyngitis include:
- Amoxicillin. Russian antibiotic of the synthetic penicillin group. Contains the substance amoxicillin trihydrate. Promotes inhibition of cell wall synthesis. Used in the treatment of infectious diseases of the respiratory tract.
Available in tablet form. It is prescribed as a tablet three times a day. Price - about 70 rubles for 20 tablets (500 mg).
- Amosin. Another powerful Russian antibiotic based on the substance amoxicillin trihydrate. It is used in the treatment of bacterial diseases of the upper and lower respiratory tract caused by pathogenic microorganisms sensitive to amoxicillin.
It goes on sale in the form of tablets. The optimal dosage is one tablet three times a day. The cost is within 75 rubles for 10 tablets (500 mg).
- Azithromycin. Belongs to the group of macrolide antibiotics. Made in Russia, based on the substance azithromycin. In high concentrations it helps to provide a powerful bactericidal effect. It is a broad-spectrum antibiotic. Marked by high efficiency in the treatment of infectious lesions of the respiratory tract.
Available in tablet form. It is prescribed as a tablet once a day. The maximum permitted duration of treatment is 3 days. You can buy an antibiotic for about 100 rubles (3 tablets of 500 mg each).
It is unacceptable to use antibiotics for self-medication! It is also forbidden to take them for a long time (longer than 5-7 days), since antibiotic drugs destroy the beneficial intestinal microflora.
Complications and consequences
Advanced nasopharyngitis, which was improperly treated and became chronic, can manifest itself as periodic exacerbations. Over time, pathological processes in the nasopharynx lead to complications such as granulosa pharyngitis, sinusitis, sinusitis, tracheobronchitis, etc.
Considering the possible negative consequences and complications, prevention of posterior rhinitis should be aimed at strengthening the body's defenses through hardening, maintaining a proper diet, avoiding hypothermia, and avoiding the influence of allergenic and toxic substances. This will help avoid the negative effects of viruses and infections, the consequence of which is nasopharyngitis.
Reasons for development
Pathologies develop when foreign microorganisms or allergens enter the upper respiratory tract. In addition, nasopharyngitis can be a consequence of exposure to chemical and mechanical irritants.
The main causes of the development of inflammatory processes in the nasopharynx.
- Viruses. The main culprit is the rhinovirus. An exacerbation in half of the cases is observed in the autumn and spring periods. In addition, adenoviruses (peak incidence occurs in the winter), parainfluenza viruses, influenza viruses, coronaviruses, MS (respiratory syncytial viruses) and enteroviruses can influence the development of the disease. Microorganisms, after contact with the mucous membranes, begin to rapidly multiply and cause an acute inflammatory process, which almost instantly spreads to the nasopharynx and pharynx.
- Bacteria. In the overwhelming majority, inflammation of the nasopharynx is caused by chlamydia, beta-hemolytic streptococcus type A, Staphylococcus aureus, Haemophilus influenzae, mycoplasma, and rarely meningococci. Sometimes there is a combination of several types of bacterial agents. The proliferation of pathogenic microorganisms occurs when the body’s protective functions are weakened.
- Allergens. Allergic rhinitis can also cause nasopharyngitis. It develops when various allergens come into contact with the mucous membranes of the upper respiratory tract - dust particles, waste products of insects, animals, birds, pollen, etc.
- Sometimes damage to the pharynx - pharyngitis - occurs due to chemical and mechanical irritants (hot or too cold drinks, inhalation of frosty or contaminated air, smoking).
Predisposing development factors are:
- hypothermia;
- recent history of other infectious diseases;
- air pollution;
- adenoiditis;
- chronic diseases of the ear, nose, throat, internal organs;
- difficult nasal breathing.
Nasopharyngitis can also be provoked by poor nutrition, lack of vitamins and microelements in the foods consumed.
Virus penetration
This happens because the path of these infectious agents begins through the nose or throat.
Getting with droplets of saliva from a sick body to a healthy one, viruses settle on the mucous membrane inside the nose and throat.
Primary reproduction
The initial stage of reproduction takes place here. The first symptoms of the disease will be symptoms of damage to these organs. Then, at the height of the disease, damage to the deeper structures of the respiratory system is possible. And it all usually starts with a simple runny nose and sore throat. And these are manifestations of acute nasopharyngitis.
Immune response
If the immune system is able to give a worthy rebuff, and this is often what happens, then the entire disease ends at the level of these manifestations from the respiratory tract and manifestations of intoxication. General symptoms are usually moderate. Because the activity of the virus is countered by reliable protection.
And the virus is most likely weak.
Treatment of allergic pharyngitis
Treatment of allergic pharyngitis is reduced mainly to conservative therapy:
- Stopping contact with the allergen;
- Medication correction;
- Specific allergen immunotherapy.
Once the allergen has been identified, it is necessary to limit contact with it as much as possible. It should be taken into account that even maximum isolation of the allergen will give a positive result only after several months. However, it is not always possible to completely limit the patient’s contact with a pathogenic agent, so drug therapy has to be intensified.
A modern method of treating allergic pharyngitis is allergen-specific immunotherapy. It comes down to treating the patient with increasing doses of the allergen, which is most often administered subcutaneously.
This procedure is carried out only by an allergist in a specialized office and for the following indications:
- Ineffectiveness of drug correction;
- Patient refusal to take medications;
- Negative effects of drug treatment;
- Clear identification of the allergen and achievement of stable remission of the disease.
Causes and risk factors of pathology
Initially, swelling of the nasal mucosa develops; narrowed nasal passages force the child to gasp for air. If the weather is cold and the air is dry, then inflammation and swelling of the pharynx occurs.
Other factors and causes of nasopharyngitis:
- Penetration of adenoviruses into the child’s body.
- The presence of a foreign body in the nasopharynx.
- Being in a room that smells of tobacco smoke or chemicals.
- Allergy to food or any substances.
- Untreated infectious diseases that have become chronic.
- The presence of staphylococci, streptococci, candidal fungi, pneumococci in the body.
- The disease can be provoked by other ailments (for example, with posterior rhinitis) or a deviated nasal septum.