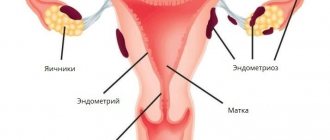
Each organ of the human body is located in a certain place and in a certain position. A woman's uterus is normally located in the pelvis between the bladder and rectum. The body of the uterus is tilted anteriorly, and the cervix, on the contrary, is tilted posteriorly. Thus, an obtuse angle of 70-100 degrees is formed between the body and the cervix. The uterus is a movable organ; it is capable of slightly changing position depending on the filling of the bladder or rectum. This mobility is ensured by its own tone. In addition, the condition of the muscles and ligaments of both the uterus itself and the pelvic floor is of great importance. Under the influence of various factors, this anatomical and physiological position of the organs can change to one degree or another, which is associated with weakening of the muscles or ligaments.
Uterine prolapse is a pathological position of the uterus and its cervix in relation to the anatomical and physiological boundaries where this organ is normally located. In the absence of adequate and timely correction, this condition can be complicated by uterine prolapse, that is, complete or partial prolapse of this organ through the vagina. Anomalies in the anatomical position of organs are rarely an independent pathology; quite often doctors have to note simultaneous prolapse or prolapse of the uterus and displacement of the vaginal walls. This condition causes a woman very significant discomfort and quite unpleasant and sometimes painful sensations.
A condition in which the uterus descends but does not protrude from the genital opening is called uterine prolapse. If the uterus descends so much that it extends beyond the genital slit, then it is customary to speak of uterine prolapse. Such pathological processes are often accompanied by downward displacement of the vagina. Women of all ages suffer from prolapse or prolapse of the uterus. Women over the age of 50 are more at risk, it is less common in women aged 30-40, and only in 10% of all cases do doctors diagnose a similar pathology in women and girls under the age of 30.
Displacement of the organs of the reproductive system often causes a violation of the anatomical location of other internal organs and their functional disorder. In most cases, the rectum or bladder is displaced.
What is uterine prolapse?
Uterine prolapse is a pathology in which the organ moves down into the vagina until it completely falls out, while the cervix remains in its place.
This condition is one of the manifestations of a disease called throughout the world “pelvic organ prolapse.” Uterine prolapse can be found in women of any age.
The uterus is fixed in the pelvic cavity in a normal position by the ligamentous apparatus and the muscles and fascia of the pelvic floor, and the organ’s own tone also plays a significant role in this. As a result of damage to the structures that support the uterus, its prolapse occurs.
Operation
If possible, the doctor tries to preserve the uterus, because when it is removed, the risk of other organs being missed increases.
Groups of operations for the treatment of uterine prolapse:
- Colpoperinelevatoroplasty – strengthening the muscles of the pelvic floor;
- Plastic surgery of the uterine ligaments - shortening and suturing them to the anterior wall of the organ;
- Strengthening the cardinal and uterosacral ligaments that fix the uterus - reproductive function may be impaired;
- Summing the uterus to the walls of the pelvis - to the sacrum, to the pubic symphysis;
- Implantation of endoprostheses;
- Narrowing of the vagina;
- Removal of the uterus if there are compelling reasons.
These operations are performed in several stages, by laparotomy, through the vagina, or by abdominal surgery. In 30% of cases, relapse of the pathology occurs.
Please note: modern surgical methods make it possible to strengthen the vaginal walls and musculo-ligamentous apparatus by installing biologically inert reinforcing devices that reduce the likelihood of relapse.
After surgery, carrying weights over 5 kg, sexual contact, and any physical activity are limited for one and a half months.
Causes of uterine prolapse
The causes of this pathology are numerous. In the etiology of this disease, the main factor is the weakening of muscle tone, the muscles of the perineum and abdominal muscles.
The most common reasons are:
- Mechanical injuries of the perineal muscles.
- Incorrect obstetric care (to avoid a Caesarean section, to help a woman give birth, they use vacuum extraction, forceps) which leads to this disease.
- Consequences of operations performed on the pelvic organs.
- Postpartum perineal ruptures.
- Congenital anatomical anomalies in the pelvic area.
- Hard physical work.
- In old age, it often occurs due to a decrease in the synthesis (production) of estrogen.
- Excess body weight and constipation, for which proper treatment was not carried out.
- Women who have given birth often suffer from this disease more often than those who have not given birth.
One reason is just a risk factor for a pathological process; a combination of several reasons usually leads to its development.
Causes of the disease
Doctors believe that one of the reasons causing uterine prolapse is a hereditary factor. In families where women have a similar pathology, cases of uterine prolapse and prolapse occur with a high degree of probability.
Also on the list of reasons are: gynecological diseases, congenital defects, hormonal changes in the body, injuries, labor and various mechanical influences.
Causes of pathology
One of the main reasons for uterine prolapse is a decrease in the tone of the pelvic floor muscles and relaxation of the ligamentous apparatus surrounding the organ itself. This condition is caused by various factors:
- heredity;
- age-related muscle atrophy and decreased elasticity;
- numerous births, which, due to the powerful pressure created on the pelvic organs and hormonal levels, negatively affect the condition of the muscles and ligaments;
- an initially weak muscle corset, for example, with an asthenic body type.
Physiological causes of uterine prolapse may include: injuries to the pelvic floor muscles, surgical interventions, deep ruptures of various origins, as well as congenital pathology. Injuries often occur during difficult childbirth, when an obstetrician-gynecologist removes the fetus from the uterine cavity through the birth canal manually, using the vacuum method or using obstetric forceps.
Physical labor, which is uncharacteristic for women, with daily weight lifting, can significantly contribute to the development of this condition.
Displacement of the uterus can be provoked by systematically increased intra-abdominal pressure caused by diseases of other internal organs, obesity, etc.
Hormonal changes in the body can also lead to the appearance of this pathology. This happens when the production of estrogen is disrupted and, as a result, the ability of muscle tissue to contract at the same intensity is lost. Gradually they lose their mass and tone.
Uterine prolapse is also common during pregnancy, but this condition is not a pathology. Due to the growth of the fetus, all internal organs are displaced. However, women who have a history of problems associated with normal uterine displacement should pay special attention to such changes during childbirth. In such cases, pregnancy is under special control of obstetricians and gynecologists, since its course can become dramatically complicated, lead to premature birth, or the loss of the child, and threaten the health of the mother herself.
Signs of uterine prolapse
In addition to the appearance of symptoms and clinical picture, there are a number of signs that can be detected during visual examination.
Patients develop a disturbance in their psychoemotional state. Women look prone to hysterics, panic, and the feeling of anxiety worsens.
Deformation changes in the muscles of the abdominal girdle lead to:
- To wrap around the belly.
- Asymmetry of the configuration of the abdominal muscles.
- Excessive appearance of folds on the abdomen.
- Flabbiness of the lumbar muscle corset.
Symptoms
This disease, if not recognized in time, tends to progress rapidly. The clinical picture is supplemented by new symptoms, moving into a more complex stage.
Patients note:
- Vaginal dryness.
- Drawing or aching pain in the pelvic area and lower back.
- Difficulty urinating.
- Complications during the act of defecation.
- The beginning of the menstrual cycle is accompanied by acute painful attacks.
- Young women cannot get pregnant.
- False urge to defecate and urinate.
- Spasmodic pain in the anus.
- Vaginal discharge may appear, in the form of leucorrhoea, and sometimes with admixtures of blood (a sign of an infectious pathology).
- During sexual intercourse, a woman may experience pain.
- In later stages, displacement of the bladder and lower intestines develops, and the body of the uterus may protrude from the vaginal lumen. Under the influence of physical activity and walking, it becomes inflamed and bleeds.
If timely therapy is not carried out, then this pathological process is accompanied by symptoms of stagnation of blood circulation, which results in swelling of the lower extremities and varicose veins.
If pregnancy develops during uterine prolapse, it can pose a threat to the health and life of the mother and fetus.
Classification of uterine prolapse
The body of the uterus is fixed in the pelvis with the help of the muscles of the perineum and its own ligamentous apparatus. Its physiological position is characterized by a slight inclination forward, and the vagina and cervix have a reverse angle of inclination (backwards).
The anterior wall of the uterus is in contact with the bladder, and the posterior wall is in contact with the rectum. If pathological displacement of the uterus occurs, its strangulation develops. This disease is characterized by stages.
There are 4 stages of uterine prolapse:
- The body of the uterus can descend to the genital slit, but does not extend beyond it. During this period of illness, the woman experiences pain (pulling or aching). Their occurrence often coincides with the beginning of menstruation. Therefore, patients in this phase of the disease do not consult a doctor.
- Further prolapse of the uterine body occurs, and it may partially fall out of the vagina during pushing. During this period, pressure occurs on the internal organs, they also change their position, which leads to the following symptoms:
- Urinary and fecal incontinence.
- Cystitis develops.
- Tenesmus (false urge to defecate) appears.
- Pyelonephritis may develop.
- Moving in the pelvic plane , part of the uterus may protrude from the vaginal lumen. At this stage, an infection may join the pathological process, and the woman becomes unable to work. Sexual contacts are not possible.
- This stage occurs if the woman has not undergone any treatment. It is characterized by complete prolapse of the uterine body from the vaginal lumen. And may be accompanied by:
- Development of strangulation of intestinal loops.
- The appearance of bedsores.
- Attachment of infection.
Genital prolapse – what is it?
A strong frame consisting of muscles and connective tissue prevents the uterus, bladder, small intestine and rectum from extending beyond the abdominal cavity. The pelvic floor or pelvic diaphragm is represented by three layers of muscles, which not only support the genital and other muscles within the small pelvis, but also ensure the closure of the genital fissure, narrow the lumen of the rectum, participate in maintaining intra-abdominal pressure and play an important role in the process of childbirth. In addition to the pelvic floor, the uterus is supported by the ligamentous apparatus (various ligaments of the uterus itself).
Uterine prolapse is said to occur when it and its cervix are displaced and are below the anatomical and physiological boundaries, as a result of which the genitals descend to the entrance to the vagina or fall beyond its limits. Thus, genital prolapse is caused not only by the failure of the muscular layer of the pelvic floor, but also by stretching and/or damage to the ligaments supporting the uterus.
Diagnostics
The diagnosis of uterine prolapse is made by a gynecologist during examination of the patient.
At the beginning, anamnesis data is collected and analyzed. It turns out what diseases the woman had, how often she has constipation, what surgical interventions she underwent, and whether she has increased gas formation in the intestines.
After this, a vaginal examination is performed. The position of the uterus and the condition of the vagina are determined, and functional testing is performed.
A rectovaginal examination helps determine the condition of the rectum. After these manipulations, colposcopy is mandatory.
If there is a question about surgical intervention, additional types of examination are prescribed:
- It is necessary to make a diagnostic scraping in the uterine cavity.
- Ultrasound examination of all pelvic organs.
- Examine masks for histology.
- Inoculate the tank for pathogenic microflora.
- To exclude a bladder infection, perform a urine culture.
- Urography is required.
- Computed tomography allows you to clarify the functional state of internal organs.
- Additionally, an examination by a urologist and proctologist is prescribed.
When establishing an accurate diagnosis, this pathology should be differentiated:
- With a vaginal cyst.
- With uterine inversion.
- The appearance of a myomatous node.
Treatment
When treating uterine prolapse, different techniques can be used. To select them correctly, you should consider:
- The stage at which uterine prolapse occurred.
- Pathological processes that accompany uterine prolapse.
- Ways to restore a woman's menstrual and childbearing ability.
- Age indicators.
- Functional disorders that can be observed when the sphincter of the bladder and rectum is damaged.
- The degree of risk during surgery.
After analyzing the patient’s condition, treatment tactics are selected. Therapy can be conservative or performed through surgery.
Conservative method
When choosing this technique (only if the body of the uterus does not extend beyond the vagina) use:
- Exercise therapy . Its action is aimed at increasing the muscle tone of the pelvic corset.
- Increasing the elasticity of the abdominal muscles. For this purpose, effective gymnastics using the Kegel or Yunusov method is used.
- Carrying out therapeutic gynecological massage.
- The use of hormonal therapy with estrogen , which helps strengthen ligaments and muscles.
- Local use of medications based on metabolites.
- Limiting physical activity and giving women easier work.
- In old age, there are many contraindications and restrictions for surgical intervention. Therefore, during this period, vaginal tampons or a pessary are prescribed. The essence of this method is that after its introduction, the cervix is fixed, and its ring creates a fulcrum and does not allow further lowering of its body. The main disadvantage of this treatment is the inadmissibility of keeping the pessary in the vagina for a long time. This can lead to unwanted side effects, such as the development of bedsores. To prevent this from happening, it is necessary to douche the genitals every day, using a decoction of chamomile, potassium permanganate or furatsilin. Twice a month it is necessary to undergo a gynecological examination. The pessary should be used for a month. After which a ten-day break is taken.
In the treatment of uterine prolapse, a very important place is given to a corrective diet. Its goal is to increase muscle tone.
The patient's daily diet must meet the following requirements:
- Intake of fatty foods should be kept to a minimum. Eat more protein foods.
- Food should be rich in vitamins and contain a lot of vegetables and fruits.
- Try to consume more dairy and fermented milk products.
Surgical treatment of uterine prolapse
There are several surgical techniques.
Recently, three areas have been widely used to eliminate the pathology of uterine prolapse:
- A method of strengthening the muscular-ligamentous apparatus , which is carried out by shortening them.
- A technique in which the body of the uterus is attached to the sacral or pubic joint, or the ligamentous apparatus of the pelvis. With this type of surgical intervention, there is a risk of repeated recurrence of uterine prolapse. This is due to the fact that over time, ligaments tend to stretch.
- Method of using alloplasty . To date, this is the most progressive method of treating uterine prolapse. With the help of a special synthetic mesh, the body of the uterus is fixed, and it loses its ability to descend.
If conservative treatment methods do not lead to positive dynamics, then the use of surgery is inevitable.
In addition to the physiological restoration of the genital organs, surgery can eliminate defects in urination and defecation that develop as a result of uterine prolapse.
The operation can be performed using transvaginal access. It does not require an incision and is performed directly through the vagina.
With its help, colporrhaphy is performed (suturing of the vaginal walls), the body of the uterus is fixed, and loop operations are performed.
If during surgery an incision occurs in the abdominal wall, this indicates that the operation was performed using laparotomy. This type of operation allows you to fix the body of the uterus with its ligaments.
In some cases, laparoscopic access is used. This is the least traumatic type of operation. It occurs using general anesthesia.
The big advantage of this type of operation is the short rehabilitation period; the patient can be discharged on the third day. And after 6 weeks, she completely returns to everyday life.
Postoperative period
In the postoperative period, the patient must follow strict rules to avoid the recurrence of uterine prolapse:
- If possible, avoid lifting weights exceeding 5 kg.
- Follow a proper diet and avoid constipation.
- Avoid sexual contact.
- Avoid contracting colds, the main symptom of which is coughing.
- Use hormone therapy only as prescribed by a doctor.
- Avoid cycling and morning jogging.
After surgery, positive recovery dynamics can be observed when using a bandage.
This product is based on a system of elastic bandages that act on the muscles, keeping them in constant tone and helping to quickly strengthen them.
They also correct and restore the original location of the internal organs.
It is best to purchase a bandage from a pharmacy chain, avoiding online stores, since in the latter case you can purchase a low-quality fake.
Treatment at home
Such therapy is possible only in the early stages of this pathology. During its implementation, the use of traditional medicine is allowed.
They contribute to:
- Increased muscle tone.
- Providing an analgesic effect.
- Relieves pressure and excessive tension in internal organs.
The daily diet should be supplemented with the use of infusions and decoctions from:
- Quince fruit.
- Oak bark.
- Datura seeds.
To stop the progression of the pathological process, gynecological massage is used. Its action is aimed at increasing blood flow in the internal organs and relieving pain.
During this procedure, the uterus is lifted using two fingers of one hand, and massage movements are made along the surface of the anterior abdominal wall with the other hand.
During this period, it is very good to wear a bandage and a pessary. Use elements of therapeutic Kegel exercises.
Physiotherapy
Gymnastics according to the Kegel method should be performed daily, and the number of repetitions should start with 5 times, and gradually increase them to 10:
- The woman produces muscle tension, reminiscent of the process of stopping urination (you should start such exercises with 3 seconds, gradually increasing them to 20).
- The patient should quickly tense and relax the same muscle groups.
- A woman imitates movements reminiscent of prenatal attempts.
The following exercises are used to strengthen the muscles of the vagina and pelvic floor:
- “Elevator”, where you need to take a position lying on your back, bending your knees towards your stomach. Gradually, starting from the lower abdomen, muscle tension occurs. Each muscle group should be under tension for 10 seconds.
- "Bag". It is performed in a standing position with your legs spread wider than your shoulders (it is assumed that there is a bag with long handles between the legs), bending your legs at the knee joints, you need to grab imaginary arms by squeezing the genitals. The maximum number of repetitions should be increased to 10.
These are two main exercises, to which you can add:
- "Pushing out." Lying on your back, make movements reminiscent of pushing.
- "Blinking" . First, tension occurs in the muscles of the anus, which is replaced by tension in the muscles of the genital organs.
- "SOS" There is an alternation of rapid tension in the muscles of the perineum. First, three quick compressions are performed, they alternate with 3 long tensions
- "Lighthouse". There is a gradual tension of the muscles of the perineum, followed by slow relaxation.
- "Cat". At the height of inhalation, the stomach is drawn in and the back bends, at the same time the muscles of the perineum are tensed. It is recommended to hold your breath for no more than 10 seconds.
This is a sample list of exercises that are used for uterine prolapse.
Folk remedies
There are several tinctures and decoctions that should help with this disease:
- Alcohol tincture. Pour 1 part of the roots of the astragalus plant, diluted to vodka concentration with alcohol, and leave for 10 days. The resulting tincture is taken one teaspoon after meals in the morning and evening; it must first be diluted with water. Treatment follows the following scheme: 30 days with a break of 14 days, then the course is repeated. In this case, while taking this tincture, you must refrain from driving a car for one hour.
- Herbal collection of several herbs. This decoction requires 70 grams of white claspberry, 50 grams of linden blossom, 30 grams of alder, and 50 grams of mint or lemon balm leaves. All components must be mixed, take this mixture the size of one tablespoon, pour 200 milliliters of boiling water. The duration of taking this decoction is 21 days, followed by a break of two weeks. The number of courses is unlimited.
- Complex decoction. For this product you will need 30 grams of plantain, which are poured with 500 milliliters of water, then boil. Keep on low heat for 20 minutes, add a few tablespoons of honey, boil for another 10 minutes. After straining, add 10 grams of celery seeds to this mixture and mix everything thoroughly. In addition to this decoction, you need to drink a herbal infusion of herbs such as burnet, calendula, St. John's wort. This mixture should be taken three times a day.
These methods are only effective in combination with other treatment methods, since they will only help relieve certain symptoms, but will not cure the disease.
Uterine prolapse and pregnancy
Prolapse of the uterine body and pregnancy are two incompatible concepts.
Pregnancy is considered problematic due to the development of the following reasons:
- Hormonal imbalance in the body makes it impossible to conceive a child.
- If the body of the uterus falls out of the vagina, sexual intercourse becomes impossible.
- When the uterus prolapses, it is constantly in a state of hypertonicity; in this state, the entrance to the cervix closes.
If pregnancy does occur with this pathology, then its course will be constantly in danger of failure:
- Most often, during the first three months there is a threat of fading, failure and miscarriage of the fetus. This occurs due to the fact that constant pressure is exerted on the uterus from the internal organs, which ultimately deforms its walls.
- As a result of inflammatory processes, a uterine abscess may develop. It leads to pregnancy failure, and such a pathology can result not only in the loss of the fetus, but also in the removal of the uterus.
- Due to increased pressure on the bladder and intestines, urinary incontinence develops and involuntary bowel movements appear.
- The pelvic organs cannot withstand such an increase in pressure. Therefore, women diagnosed with uterine prolapse are constantly hospitalized to maintain pregnancy.
- To carry a pregnancy to term when this pathology develops, you can wear a bandage ; it helps strengthen the muscle corset and correct weight distribution.
- If before pregnancy the patient was engaged in therapeutic exercises using the Kegel technique, then it may make sense to continue these exercises (be sure to consult a doctor).
- A pessary can also be used. The most important thing is to install it correctly to eliminate negative effects on the fetus.
- The situation can be normalized by using traditional home medicine recipes , but this is always done with great caution, under the supervision of a gynecologist.
Complications
If the disease is diagnosed in a woman of fertile age, she often has the question of whether it is possible to become pregnant if the walls of the uterus prolapse. Yes, there are no special obstacles to conception in the early stages if the disease is asymptomatic. If the prolapse is significant, then before a planned pregnancy it is better to undergo surgery 1-2 years before conception.
Maintaining pregnancy with proven uterine prolapse is fraught with difficulties . Is it possible to carry a child to term with this disease? Of course, yes, although the risk of pregnancy pathology, miscarriage, premature and rapid labor, and bleeding in the postpartum period increases significantly. In order for the pregnancy to develop successfully, you need to be constantly monitored by a gynecologist, wear a bandage, use a pessary if necessary, engage in physical therapy, and take medications prescribed by your doctor.
What are the dangers of uterine prolapse in addition to possible problems with pregnancy:
- cystitis, pyelonephritis – urinary system infections;
- vesicocele - a saccular expansion of the bladder in which urine remains, causing the sensation of incomplete emptying;
- urinary incontinence with perineal skin irritation;
- rectocele - expansion and prolapse of the rectal ampulla, accompanied by constipation and pain during bowel movements;
- infringement of the intestinal loops, as well as the uterus itself;
- uterine inversion followed by necrosis;
- deterioration in the quality of sexual life;
- decrease in the overall quality of life: a woman is embarrassed to go out into public places because she constantly has to run to the toilet, change incontinence pads, she is exhausted by constant pain and discomfort when walking, she does not feel healthy.
Prevention
Prevention measures are based on recommendations that every woman must follow to avoid the pathological process of uterine prolapse:
- During childbirth (if the size of the pelvis does not allow), strong pushing should be avoided. For this, the Caesarean section method is used.
- Eat right, eat fermented milk products to avoid constipation.
- If estrogen production is low, carry out hormone therapy in a timely manner.
- Strengthen the abdominal and pelvic floor muscles with a set of exercises.
- After childbirth, heavy physical activity should be avoided.
- Before the onset of the menstrual cycle, you should not play sports, visit the solarium or baths.
special instructions
It is very important to know that this pathological process leads to the appearance of various pathologies:
- With it, a full sexual life is impossible.
- Infertility may occur.
- The blood supply to the pelvic organs is disrupted.
- Concomitant diseases (varicose veins) appear, which aggravate the process.
- The prolapsed body of the uterus can become infected and strangulated.
To prevent the appearance of such signs, you must strictly follow all the recommendations of the gynecologist:
- Have medical examinations at least once a year.
- Upon reaching 40 years of age, undergo an ultrasound examination once a year.
- Lead a healthy lifestyle, perform morning exercises (strengthen the muscular corset of the pelvic girdle).
- Follow a proper diet (avoid constipation).