Tularemia is one of the acute zoonotic infections (a group of diseases transmitted from animals to humans). In this regard, tularemia was previously called mouse or rabbit disease, minor plague, etc.
More than one hundred and fifty species of animals can serve as the source of the causative agent of tularemia. On the territory of the Russian Federation, the main reservoirs of tularemia bacteria are rodents (rabbit, hamster, mouse, etc.).
The disease is contagious. According to experts, up to 88% of diseases are associated with direct (that is, without protective equipment) contact with rodents infected with tularemia. Removing the skin from a sick animal with bare hands and without respiratory protection is a direct 100% risk of getting health problems. How can you tell if an animal is sick or not?
The result of such contact can result in damage to the lymph nodes and even the mucous membrane of the eyes.
What is tularemia
The disease is an infectious and potentially fatal disease. The initiator of the virus is the Francisella tularensis strain, which lives in animal organisms. Otherwise, tularemia is also called “deer fly” or “rabbit fever”. Tularemia affects rabbits and small rodents, although it can also occur among domestic animals: cats, dogs, sheep or hamsters.
People can also get tularemia from their animals. Infection can occur in several ways:
- close proximity and contact with a sick animal;
- through insect bites.
Susceptibility to infection in humans is almost 100%, which means that through tactile contact with a sick animal, anyone can contract tularemia. Its manifestation is observed depending on the season, but more often it is active in the summer and autumn periods of the year.
Tularemia activity is noted in areas located closer to the north. For example, in Russia this infection can be found everywhere, but more often in the northern and central regions. Every year, up to 75% of the population is infected here, and 70% are residents of cities who have not previously been vaccinated. The mortality rate from the disease is 1%.
There are several types of forms of infection. Let's get acquainted with them:
- The bubonic form of tularemia occurs due to infection through the skin. Localized lymphadenitis may already develop here. Sometimes with this type of disease, viral strains enter the lymph nodes located in the groin, armpits, and thigh. With the active development of tularemia, a secondary bubonic form occurs;
- Lymph nodes become too large after infection with the virus. In some cases, they reach the size of a chicken egg and have distinct contours. At first, they cause inconvenience and pain. After a couple of months, the tumors resolve, the pain decreases, and the area begins to rot, abscesses are observed, followed by the formation of a fistula;
- Bubonic form with the presence of ulcers;
- When the bacilli enter the bloodstream, this form of tularemia occurs. In the place of the skin through which the infection entered the body, an ulcer immediately forms. Its top is covered with a darkish crust, the edges are raised slightly upward. In parallel, the development of localized lymphadenitis is observed;
- Oculobubonic form. With this type of tularemia, the eye is affected by an infection and ulcerative-purulent conjunctivitis and localized lymphadenitis develop. The eye swells, turns red, and hurts a lot. After infection, papules form, which progress and festering ulcers. Tularemia does not affect the cornea. This is a rather rare, severe form of tularemia, which drags on for a long time;
- Anginal together with the bubonic form. Infection in this type occurs through the laryngeal region. It is enough to consume water or food contaminated with bacilli. The following clinical manifestations may occur:
- painful sensations in the larynx;
- difficulty swallowing food;
- swelling and redness of the tonsils; a gray necrotic coating may form on them, which is difficult to remove;
- enlarged lymph nodes in the neck, near the ears, under the jaw;
- Abdominal clinical form. The virus affects the small loop of the intestine (mesentery), causing abdominal pain, gag reflex, diarrhea, and in some cases even anorexia;
- Pulmonary form. Infection with the strain occurs through inhalation of dust microparticles that contain tularemia bacilli. There are two types:
- The pneumonic type lasts a very long time with the characteristic features of focal pneumonia. Complications may include pleurisy, cavity abscesses, and sometimes pulmonary gangrene;
- With the bronchial type, the bronchi and mediastinal lymph nodes are often affected. The patient has a dry cough, a gag reflex, and moderate pain in the chest. Recovery occurs in a couple of weeks.
With the generalized type, there may be remitting chills, intense poisoning of the body, muscle pain, the person hallucinates, feels dizzy, and consciousness is confused.
Possible complications
The vast majority of patients with tularemia can be cured without consequences. But in approximately 1-2% of cases of the disease, complications are observed, mainly related to the generalized form of tularemia.
Common complications include:
- meningitis and meningoencephalitis,
- secondary pneumonia,
- infectious psychosis after tularemia,
- chronic joint damage - polyarthritis,
- progressive heart disease - myocardial dystrophy,
- chronic course with frequent relapses.
Mortality with tularemia is less than 3%, with a generalized form - 30-60%.
The causative agent of tularemia
As already stated above, the causative agent of tularemia is the pathogenic microorganism Francisella tularensis. The causative agent of tularemia is hardy, it is able to survive for about a month in one space at temperatures up to +4C, and in secluded places (grain or straw stacks) up to 0C for about six months. In the skin of an animal that has died from disease, bacteria live even longer. They die from disinfection treatment and boiling. There are several ways of infection. Let's look at them:
- The strain is transmitted through a transmissible method. The source of tularemia disease spread is mainly small mammals, rodents, domestic animals or birds. For example, any animal can bite an infected ixodid tick, midge, or mosquito and infect it. Animals can infect people. People don't infect each other;
- Respiratory method of infection. A person or animal can become ill by inhaling contaminated grain pollen. If he works at a meat processing plant, is involved in the processing of plant materials, killing cattle and other agricultural production;
- The contact method is found among the rural population, where tularemia most often breaks out. The risk group consists of fishermen, people running farms or households, hunters, and slaughterhouse workers.
Popular Just a scratch can cause tetanus in a child
The greatest risk of infection occurs when slaughterers or hunters cut up animal carcasses and process their skins. With this method of infection with a tularemia strain, a bubonic form with ulcers or a bubonic type of disease is observed.
Tumors primarily appear on the hands, where contact with the harmful microorganism occurred. The ocular bubonic form will appear when touching the eyes with dirty hands. Here the virus settles on the mucous membrane of the eye;
4. Alimentary route of infection and through water. Abacillation by the viral strain can occur if a person consumes water or food containing the bacilli. Tularemia bacilli enter open water bodies from the excrement and urinary fluid of small rodents that suffer from tularemia. The same applies to fields with grain crops, straw and hay stacks. With this type of infection, the abdominal type of disease also appears.
Epidemiological factors of the disease
Tularemia is part of the group of classic natural focal diseases.
For reference. The source of tularemia in humans can be hamsters, rabbits, sheep, all types of mouse-like rodents, etc. In rare cases, frogs, fish and birds can act as a source and reservoir of tularemia.
Tularemic bacteria are released into the environment in the feces of infected animals.
The main carriers of tularemic bacteria are blood-sucking insects (ixodid and gamas ticks, mosquitoes, horseflies). Due to the activity of blood-sucking insects, constant circulation of the causative agent of tularemia is maintained in natural foci.
Attention. Tularemic bacteria can enter the human body through lesions on the skin. Also, tularemic bacteria can overcome intact mucous membranes of the oropharynx, gastrointestinal tract, eyes and respiratory tract.
The pathogen enters the human body:
- contact (during contact with infected rodents, when cutting carcasses or processing the skins of infected animals, while swimming in infected bodies of water, etc.);
- nutritionally (tularemic bacteria enter the human body with infected and thermally untreated meat, milk, water);
- aerosol (infection occurs by inhaling bacteria with infected dust particles);
- transmissible (tularemic bacteria enter the body through the bites of insects that carry tularemia).
The form of tularemia that develops after infection directly depends on the mechanism of infection. Symptoms of pulmonary forms of tularemia develop when aerosol mechanisms of infection occur; the anginal-bubonic form of tularemia and abdominal forms develop when tularemic bacteria enter the body from alimentary sources.
Main foci of infection
Tularemia flares up mainly at certain times of the year, usually in summer and autumn, less often in spring. In the spring, bubonic and bubonic diseases with ulcers can be observed more often. That is, in spring local forms of the disease are more common. During this period, they hunt rats living in the water.
Autumn is characterized by the manifestation of tularemia in anginal and pulmonary forms. This is explained by the fact that wild rodents during this period are too susceptible to infection. At the end of summer, the maximum peak occurs in the transmissible form of the disease tularemia. It is at this time of year that grain harvesting and haymaking take place.
The main natural foci of tularemia infection are forests, meadows, fields, swamps, areas near streams, and steppes. In these places, outbreaks are especially persistent due to the fact that the virus strain is constantly transmitted by small rodents, blood-sucking insects and other types of animals.
In some cases, infection can occur through the use of raw materials that were imported from epidemiologically unfavorable places. In this case, human infection occurs 100%.
Epidemiology
The reservoir and source of infection are numerous species of wild rodents, lagomorphs, birds, dogs, etc. Bacteria were isolated from 82 species of wild animals, as well as from domestic animals (sheep, dogs, artiodactyls). The main role in maintaining infection in nature belongs to rodents (water rat, common vole, muskrat, etc.). A sick person is not dangerous to others.
The transmission mechanism is multiple, most often transmission. The pathogen persists in nature in the tick-animal cycle and is transmitted to farm animals and birds by ticks and blood-sucking insects. Specific vectors of tularemia are ixodid ticks.
A person becomes infected with tularemia as a result of direct contact with animals (skinning, collecting dead rodents, etc.), as well as through the nutritional route through food and water infected with rodents. Infection often occurs through blood-sucking vectors (ticks, mosquitoes, fleas, horseflies and other arthropods). Infection through the respiratory route is also possible (by inhaling infected dust from grain, straw, and vegetables).
Cases of human diseases have been registered in industries associated with the processing of natural raw materials (sugar, starch-molasses, alcohol, hemp factories, elevators, etc.), in meat processing plants, during the slaughter of sheep and cattle, which had infected ticks, in outskirts of cities located near natural centers. There are known cases of infection being imported during the transportation of products and raw materials from areas unfavorable for tularemia.
The natural receptivity of people is high (almost 100%).
Main epidemiological features
Tularemia is a common natural focal disease, found mainly in the landscapes of the temperate climate zone of the Northern Hemisphere.
The wide distribution of the pathogen in nature, the involvement of a large number of warm-blooded animals and arthropods in its circulation, and the contamination of various environmental objects (water, food products) also determine the characteristics of the epidemic process.
There are various types of foci (forest, steppe, meadow-field, name-swamp, in river valleys, etc.). Each type of outbreak corresponds to its own species of animals and blood-sucking arthropods that take part in the transmission of the pathogen.
Adults predominate among the cases; often the incidence is associated with the profession (hunters, fishermen, agricultural workers, etc.). Men get sick 2-3 times more often than women.
Anthropurgic foci of tularemia arise during the migration of infected rodents from their habitats to populated areas, where they come into contact with synanthropic rodents.
Symptoms of tularemia
After the pathogen enters the body, the incubation period begins, which lasts 1-30 days, but most often a week. Let's look at the main symptoms of tularemia that are characteristic of tularemia:
- Increased body heat up to 38-40C;
- Manifestation of weakness in the body, the presence of fever (constant or remitting, wavy, intermittent), pain in the muscles and temporal part;
- Intoxication, gag reflex;
- Conjunctivitis, scleral damage;
- Hyperemia of the facial surface, nasal and oral cavity;
- Skin rash, exanthema;
- Low blood pressure.
The fever lasts up to two to three weeks. After this, the person may develop hepatosplenomegaly. All clinical forms depend on the route of origin of infection.
Forecast
With proper treatment, almost all patients recover. If left untreated, mortality rates range from 6% in people with ulcerative glandular tularemia to 33% in those with typhoid, pulmonary or septic forms. Death usually occurs due to severe infection, pneumonia, meningitis, or peritonitis.
Relapses are rare, but do occur if not treated properly. People who have had tularemia are immune against reinfection.
Diagnosis of tularemia
To make a correct diagnosis, it is necessary to collect an anamnesis about the primary signs of the disease, inflammatory processes characteristic of tularemia, and the results of examinations (urine, blood). It is necessary that the primary diagnosis of tularemia be as accurate as possible; therapeutic therapy will depend on this. The sequence of actions is as follows:
- It is necessary to tell the doctor whether there have been any insect bites in recent days, where the person was, what he ate. Every small detail matters for treatment;
- This is followed by bacteriological studies. A puncture is taken from the bubo, and the contents of the ulcer or affected areas near the eye are sent for analysis. If the animal has already died from the disease, test smears are taken from its internal organs and examined under a microscope;
- Serological research methods are carried out - RA and RPGA. This is the most sensitive test for diagnosing tularemia. Primary diagnosis is recommended using PCR.
The earliest method of diagnosing the disease is considered to be an allergic skin test, in which tularemia antigen is taken for analysis. To do this, take 0.1 ml of the substance and inject it subcutaneously. After two days, the result is evaluated. An infected or previously vaccinated person or animal who has had the disease may develop a papule, which means that the test is positive.
At the onset of the disease, the presence of the virus can be detected in neutrophilic leukocytosis, which subsequently reduces the total number of leukocytes. In parallel with this, the concentration of lymphocyte and monocyte particles increases.
Etiology
Francisella tularensis is the causative agent of infection. This is a small gram-negative bacterium, highly pathogenic and having characteristic morphological, physiological, tinctorial, cultural, antigenic, and biochemical properties. Thanks to special phenotypic characteristics, intraspecific differentiation of the microorganism is carried out - division into subspecies and biovars. The intracellular parasite lives in phagocytes, suppresses their ability to kill foreign agents and reduces the body's immune defense. The tularemia bacillus is a fairly tenacious microbe.
Francisella tularensis is a non-motile aerobic rod that does not form flagella or spores, and has a capsule that ensures its resistance to environmental factors. A characteristic feature of bacteria is pronounced polymorphism: they can take the form of small coccobacilli.- The bacterial cell is susceptible to various dyes - Ziehl fuchsin, methylene blue. For diagnostic purposes, it is stained according to Romanovsky-Giemsa.
- The microbe does not grow on simple media - MPA and MPB. It needs vitamins, glucose and other special nutrients. Francisella tularensis is a strictly aerobic microorganism. In oxygen-free environments it dies. The tularemia bacillus is grown in complex solid and liquid media with yolk, blood, cysteine, tissue extracts and other stimulants. In laboratory conditions, Francisella grows very slowly.
- The pathogen is resistant to most environmental factors. It is well preserved in water bodies, soil, grain, and skins of dead animals. The bacteria are resistant to high humidity and hypothermia: at 0 degrees they remain active for 10 months, at −30 °C for about a year. Microorganisms are sensitive to boiling, ultraviolet radiation and some disinfectants - phenol, formalin, sublimate, ethanol, Lysol, chloramine, bleach. In laboratory conditions, the culture is neutralized by keeping it in a disinfectant solution for 24 hours, autoclaving and burning. Tularemia bacteria are sensitive to a number of antibiotics: Streptomycin, Erythromycin, Levomycetin, Tetracycline, Rifampicin, and are resistant to penicillin drugs.
- The causative agent of tularemia is a biochemically active microorganism. It has a wide range of different enzymes that ensure invasion and adhesion, penetration of microbes into macrophages, pathogenicity and virulence. These include neuraminidase, lipase, hyaluronidase, DNase, protease and others. They destroy receptors on the surface of cells, penetrate and attach to them. Many of the enzymes have antigenic properties.
- Pathogenicity factors ensure the introduction of microbes into the human body and their rapid spread. The capsule protects the cell from the effects of disinfectants and drying, promotes its adhesion to the host epithelial cells, contains nutrients, has antigenic properties, activates the immune system and stimulates the antimicrobial response. Outer membrane proteins have a modulating effect on the activity of macrophages - they penetrate phagocytes and disrupt their functions, bind to antibody fragments and deactivate the complement system. Lipopolysaccharide is the main factor and the main antigen. It plays the role of endotoxin, provokes intoxication, and causes infectious-toxic shock. Due to its pronounced antigenic properties, it stimulates humoral immunity and provides the phenomenon of attenuation - the transition of the active form of the bacterium to an inactive one when attempting to cultivate in laboratory conditions. Francisella tularensis has O and Vi antigens.
Treatment of tularemia
The treatment course for this disease is carried out strictly in hospital conditions: from the onset of the disease until complete recovery. The person is prescribed a course of antibacterial drugs, antipyretic tablets and drugs to relieve inflammatory processes. For complete recovery, treatment for tularemia should include vitamin complexes and antihistamines.
Sometimes it may be necessary to prescribe several types of antibiotics to a patient at once to combat harmful microorganisms. For example, this is a tetracycline type medicine that must be taken for at least a week. If a relapse occurs, the patient is prescribed a different type of antibiotic. If the fever has decreased, but the treatment has been delayed, the medication is extended for a few more days. It is recommended to combine antibiotics with a vaccine to help the body fight the tularemia pathogen.
Popular Prevention of tick-borne encephalitis and treatment in children
Sterile dressings are applied to the inflamed lymph nodes, which must be changed daily. Buboes containing purulent discharge are opened and drained. When treating tularemia, it is important to first eliminate intoxication in order to quickly remove harmful bacteria and toxins from the body. The following drugs are used to treat intoxication of the body:
| Medicine | Mechanism of action on the body | How to use |
| Reamberin | Due to the reduction in the total number of free radicals, there is a detoxifying effect. The antihypoxic effect is removed. The alkaline and acid balance returns to normal. | It is recommended to take one dose equal to 500 ml per day. The dropper is prepared so that 1 ml of solution enters in one minute. |
| Vitamin C | Thanks to this vitamin, oxygen starvation in cells is eliminated and inflammation is reduced. | In acute cases of the disease, the vitamin is administered intravenously. It is added to saline solutions when a patient is given IVs. When the patient feels better, the vitamin should be injected intramuscularly for a week. |
| Polividon | The medicine is able to bind toxins due to its molecular structure. They are then eliminated from the body through urination. | The drug is given in one dose, which is 200-400 ml. The dropper should drip at a rate of 40 drops/minute. |
| Vitamin B6 | Metabolic processes in the body are significantly improved. Energy processes in nerve endings improve. | The patient is prescribed either 50-150 ml intravenously, or 1-3 ampoules intramuscularly. |
The following drugs are used for antibiotic treatment:
| Medicine | Mechanism of action on the body | How to use | |
| Streptomycin | The drug is able to penetrate into the cellular space of the bacillus and destroy protein synthesis. | The medicine is injected into the buttocks 500 ml twice a day. Treatment lasts two weeks. | |
| Gentamicin | |||
| Tetracycline | The drug penetrates deep into the cell and selectively inhibits protein synthesis, as a result of which the cell dies. | Four times a day, the drug is injected into the buttocks in a dose of 500 ml, and 1 tablet is given. twice a day. | |
Vaccination for the population is carried out for preventive purposes against infection by pathogenic microorganisms of the disease. Vaccinations are especially necessary for those who live in areas where infection with the tularemia bacillus is often observed.
Contraindications for vaccination against tularemia:
- The presence of chronic diseases that are in the acute stage;
- The person has an immune deficiency;
- Acute infectious and non-infectious diseases;
- Malignant tumors.
- Allergy;
- Pregnancy.
Surgical medical therapy is used only when a person’s buboes are too festered and do not open on their own. Therefore, operations of this nature are rarely performed. During surgery, local anesthesia is used for pain relief.
With spontaneous breakthrough and bleeding, the wound gets rid of purulent accumulation. After this, it is recommended to treat the open wound with an antiseptic solution. Then, tetracycline ointment is first applied to the treated area, and a sterile bandage is applied on top.
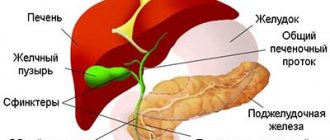
Pathogenesis of tularemia development in humans
Tularemic bacteria are able to penetrate the human body through damaged skin and intact mucous membranes.
At the same time, for infection through damaged skin or aerogenic infection, a smaller number of tularemic bacteria is required than for the implementation of the nutritional mechanism of infection. At the site of introduction of pathogenic microorganisms, the process of active reproduction of pathogenic microorganisms and the formation of primary affects begins (due to purulent-necrotic inflammation, a vesicle, pustule, necrotizing tonsillitis, necrotizing pneumonia, severe damage to the conjunctiva, etc. develop at the site of introduction of bacteria).
Subsequently, the pathogen spreads throughout the body and penetrates into the lymph nodes, accompanied by the development of a primary bubo (a specific form of lymphadenitis).
Partial death of pathogenic microorganisms occurs in the lymph nodes. As a result, there is an active release of endotoxins, which enhance inflammatory and intoxication processes.
For reference. In cases where the causative agent of tularemia manages to overcome lymphatic barriers, it enters the blood, leading to the development of generalized forms of tularemia (secondary buboes appear, damage to internal organs occurs, etc.).
When the pathogens of tularemia circulating in the blood are destroyed, intoxication symptoms increase.
It should also be noted that tularemic bacteria are capable of causing pronounced sensitization and allergization of the body, aggravating the course of the inflammatory and infectious process.
Also, due to the ability of tularemic bacteria to remain intracellularly in a latent form, the development of relapses of the disease is possible.
Features of the inflammatory process in tularemia
For reference. A specific feature of inflammation in tularemia is the formation of granulomas formed by epithelial cells, leukocytes and lymphocytes. Specific tularemic granulomas resemble tuberculosis granulomas in appearance.
Granulomas are localized mainly in the lymph nodes, liver, spleen, lungs, etc.
Granulomas often suppurate and become necrotic. Subsequently, the granuloma cavity is scarred by connective tissue.
Prevention of tularemia
For the purpose of prevention, the following precautions are taken:
- Suppression of methods of infection;
- Disinfection using disinfectants of sources of spread of the virus;
- Compliance with sanitary standards in agriculture, in home food and in enterprises;
- Carrying out disinsection/disinfection and deratization in epidemiological areas.
Other preventive measures:
- Prevention of tularemia also includes individual protective measures. If a person is interested in hunting or fishing, he may come into contact with wild animals and small rodents infected with the strain. In the case of alimentary infection, it is necessary to either wear gloves, or after being close to such animals, then thoroughly wash your hands with a disinfectant;
- Subject to observance of preventive measures against tularemia, immunization with a tularemic vaccine is used for the population. This is especially true for those areas where epidemic cases have been detected. Protective immunity is developed for 5-7 years. The population is subject to revaccination five years after the initial vaccination;
- In emergency forms of preventive measures, antibiotics are administered intravenously. As a preventive measure, all belongings of an infected person must be disinfected.
Let's look at what clothes to wear when spending time outdoors:
- If walking in natural conditions is expected in those areas where the risk of infection with the tularemia bacillus is increased, then you should select things that are as closed as possible;
- In summer, it is better to prefer long-sleeved shirts and blouses, trousers, and sportswear;
- Put a hat on your head;
- Shoes should be high, for example boots, high-top sneakers or boots with thick socks;
- A suitable type of clothing is an anti-tick suit, which provides maximum protection against insects;
- Clothing models combining chemical and mechanical protection methods. They have special traps that can catch any insects that are carriers of infections.
Classification
Depending on the course and form, tularemia can be ulcerative-bubonic, conjunctival-bubonic, anginal-bubonic, abdominal (intestinal), broncho-pneumonic with a bronchilitic and pneumonic type of course, generalized (primary septic).
Depending on the area of distribution, the infection can be of different types:
- A - Nearctic, widespread in North America, is highly pathogenic for the human population, as well as rabbits, bacteria are capable of fermenting glycerol and producing citrulline ureidase ;
- B - Holarctic, was registered in Europe and Asia, has moderate pathogenicity for humans and various rodents, bacteria are not capable of fermenting glycerol, there is no citrulline ureidase in the structure, it can be isolated from water or its inhabitants, this type is most typical for areas of the Russian Federation;
- C - Central Asian - the infection is low-pathogenic for rabbits; bacteria are capable of fermenting glycerol and citrulline .
How do you feel about mandatory vaccination?
- Positively, it prevents many diseases. 61%, 2321 votes
2321 votes 61%2321 votes - 61% of all votes
- Negatively, these are all government schemes to make it easier to manage us. 25%, 964 votes
964 votes 25%
964 votes - 25% of all votes
- Neutral, I don’t think it has any effect on my health. 13%, 500 votes
500 votes 13%
500 votes - 13% of all votes
Total votes: 3785
Voted: 3764
January 17, 2018
×
You or from your IP have already voted.