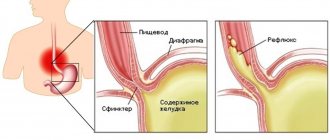
A hiatal hernia (HH) is a protrusion of the lower part of the esophageal opening of the diaphragm, through which both the esophagus and the upper part of the stomach begin to move.
This provokes reflux (reverse movement of gastric or intestinal contents), inflammation of the gastrointestinal tract tissue, peptic ulcers and cicatricial stenosis (narrowing of the lumens). All of these complications are dangerous, so you can’t do self-treatment at home.
If symptoms of a hernia appear, you should go to a gastroenterologist, who will draw up a drug therapy plan or refer you to a surgeon.
Classification
If a person has a hiatal hernia, symptoms and treatment should be determined as soon as possible. But the disease cannot be identified without the help of a specialist, as it comes in several types.
In medicine, there are three main forms of hiatal hernia:
- axial or sliding shape. Diagnosed in 90% of all cases. In this situation, the cardia is located above the place where it should be located;
- shortened esophagus. The reason lies in a congenital anomaly. Often combined with a sliding type of hernia. It can also occur as a result of an inflammatory process or injury to the walls of the esophagus;
- paraesophageal form. Diagnosed in 5% of all cases with hiatal hernia. The cardia does not change its original position. If there is a violation, an enlargement of the esophageal opening occurs. The stomach passes through it.
The type of disease can only be determined through a thorough examination.
Forms of the disease
Depending on the anatomical features, the following forms of esophageal hernia are distinguished:
- sliding (axial, axial) – free penetration of the fundus of the stomach, cardia and abdominal part of the esophagus through the esophageal opening of the diaphragm into the chest and independent return to the abdominal cavity;
- paraesophageal - the distal part of the esophagus and cardia are located under the diaphragm, part of the stomach is displaced into the chest cavity and is located next to the thoracic esophagus;
- mixed;
- congenital short esophagus - the length of the esophagus does not correspond to the height of the chest, while part of the stomach is located above the diaphragm in the chest cavity, the lower esophageal sphincter is absent.
Sliding esophageal hernias, depending on the area being displaced, are divided into total gastric, subtotal, cardiofundal or cardiac.
Paraesophageal hiatal hernias can be antral or fundic.
Source: myshared.ru
Causes of hernia development
A diaphragmatic hernia of the esophagus can be diagnosed in both an adult and a very young child. A newborn may have a congenital hiatal hernia, which is caused by a short esophageal tube and a number of other defects in the intrauterine development of the gastrointestinal tract.
The possibility of developing a hiatal hernia in an adult is determined by the following groups of factors:
- change (decrease) in the elasticity and strength of the muscle and connective tissue structure of the diaphragm;
- prolonged and significant increase in pressure inside the abdominal cavity;
- change in the motor function of the esophageal tube.
Changes in the main respiratory muscle, or more precisely in the connective tissue ring surrounding the esophagus and ensuring the tightness of the chest and abdominal cavities, of the human body are associated with age-related characteristics (a decrease in the elasticity of the ligamentous apparatus and a decrease in muscle strength is observed in most middle-aged and elderly people); a number of diseases, hereditary factors.
A person may have a pathology of the nervous system that determines disturbances in the innervation of the diaphragm and, accordingly, increases the likelihood of developing a hiatal hernia. Similar processes are also observed in weakened, asthenic people, patients with certain hereditary diseases (Marfan syndrome).
Under normal conditions, the pressure inside the abdominal cavity exceeds that in the chest. Under certain conditions, the pressure increases even more and the organs inside the abdominal cavity put significant pressure on the diaphragm. In the place of least resistance - the connective tissue ring in the area of the esophageal opening - a gate for a hiatal hernia is formed. A significant increase in pressure inside the abdominal cavity is observed with:
- repeated episodes of vomiting;
- persistent cough (COPD, asthma, recurrent bronchitis);
- ascites;
- pathological and physiological pregnancy;
- significant physical activity (weight lifting);
- obesity 3-4 degrees.
Changes in esophageal motility are one of the significant components of a hiatal hernia. The most important are dyskinesia of the hypermotor type, that is, accompanied by excessive movements of the esophagus in its upper parts. In this case, the esophagus seems to be pulled up - a hiatal hernia is formed. This situation can be either an independent disease or a manifestation of combined gastrointestinal pathology. Such situations include, for example, the Saint triad (colon diverticulosis, cholecystitis, hiatal hernia) and the Castaing triad (the same hiatal hernia, peptic ulcer, cholecystitis).
The above possible causes of hiatal hernia do not necessarily lead to the formation of this disease, but significantly increase the risk of its development.
What it is?
To clearly answer what a hiatal hernia is in simple words, you should remember human anatomy. The esophageal tube is a hollow organ 25–30 cm long; when connected to the stomach, it passes through a special opening in the diaphragmatic bridge, which divides it into the thoracic and abdominal sections.
The diaphragm is essentially a muscular transverse partition that participates in the act of breathing due to the pressure difference created in the intra-abdominal space. The esophageal tube, large blood vessels and nerve trunks run through the opening of the diaphragm. When the ring is overstretched and weakened, the following protrudes into the chest cavity: the lower part of the esophagus along with the sphincter, the fundus of the stomach, and other organs. The occurrence of such a protrusion is called a hernia.
The disease is classified in ICD 10 as K 44.0 - patent hernia and K 44.9 - hernia with obstructed patency. The next question is how to treat the emerging pathology depends on the severity of the disease, which means that correct diagnosis plays an important role.
Symptoms
At the first stage, the disease usually does not manifest itself in any way. The chest area begins to hurt only when a large hole is formed and part of the stomach passes through it.
Gradually, a hiatal hernia makes itself felt and is manifested by the following symptoms:
- Heartburn that occurs on an empty stomach or after eating, while lying down. Leaning your body forward can make heartburn worse;
- Feeling short of air;
- At night, there is an increased secretion of saliva, coughing attacks are accompanied by a feeling of suffocation.
- Dysphagia. It is characterized as the appearance of difficulties when moving both solid and liquid food through the esophagus. This sign appears
- stronger when eating hot or cold food, as well as during rapid absorption;
- Painful sensations. This is the most characteristic sign of the disease. The pain can occur suddenly and very strongly. Places of occurrence: behind the sternum, “under the stomach”, in the hypochondrium on the left side. Can increase significantly with physical activity and movement;
- Difficulty swallowing, feeling of a lump in the throat. When trying to “swallow” its pain may increase, creating unpleasant sensations behind the sternum;
- Regurgitation, belching of bitter air, can be produced either by air or by food. Upon completion, the patient’s well-being improves;
- Hoarseness of voice. Its appearance is explained by the release of part of the stomach contents into the oral cavity and larynx;
- Cough. It appears due to pinching of the vagus nerve. It is often associated with suffocation attacks and abnormal heart rhythms;
- Hiccups. It can be quite long, which causes a lot of inconvenience for patients;
- Burning tongue. It is observed quite rarely due to gastric contents entering the mouth.
Some patients may suddenly experience increased blood pressure and hoarseness.
Signs of infringement
One of the dangerous complications is a strangulated hernia. This process occurs not only during a long course of the disease, but also when the first signs appear.
A pinched hernia is indicated by:
- sudden sharp or shooting pain in the lower chest;
- painful sensations spreading to the shoulder blade or collarbone. Their intensification is observed with increased motility of the intestinal tract. The pain syndrome manifests itself quite strongly, which often leads to a state of shock;
- gagging that does not stop for a long time;
- severe bloating and increased gas formation.
If such a symptomatic picture occurs, it is necessary to urgently call an ambulance and hospitalize the patient in the hospital.
Complications
The main complications that provoke hernias include the following conditions:
- gastritis, as well as an ulcer in the area of the part of the stomach in which the hernia is located (about 8% of cases);
- anemia, bleeding (up to 20% of cases);
- intussusception of the esophagus or penetration of its lower part into the hernial sac;
- shortening of the esophagus (with cardiaesophageal hernias);
- prolapse (i.e. retrograde prolapse) into the esophagus of the gastric mucosa (a complication observed in very rare cases);
- strangulated hernia (the most serious complication caused by this formation).
Forecast
In the absence of timely diagnosis and treatment, a paraesophageal hernia can lead to diseases associated with erosive and/or ulcerative lesions of the esophagus and upper segment of the stomach:
- peptic ulcer;
- perforation of the esophagus;
- esophagitis of catarrhal, ulcerative or erosive form.
In some cases, cicatricial stenosis of the esophagus , strangulation of the hernial sac, and angina of reflex etiology develop. A long-term absence of appropriate therapy in 30% of cases provokes the occurrence of esophageal cancer, while adequate treatment in 80% of cases leads, if not to a complete recovery, then to a noticeable improvement in the patient’s condition, and relapses are recorded extremely rarely.
Diagnostics
The secrecy and lack of specificity of some symptoms characteristic of a hiatal hernia often leads to patients wasting time and being unsuccessfully treated for other diseases. This can be dangerous; everything related to diagnosing internal organs requires not only the participation of professionals, but also special medical equipment. Diagnosis of a hiatal hernia is quite simple. The doctor prescribes a series of tests and, based on the results obtained, confirms or excludes the presence of pathology.
From instrumental studies, for the accuracy of the diagnosis, the following data may be needed:
- X-ray examination. Without this procedure, confirmation of the diagnosis is almost impossible. An examination is prescribed for all patients with suspected hernia. The study allows you to assess the condition of internal organs. During the procedure, ulcers, narrowing and inflammatory processes in the esophagus may be revealed. This diagnostic method is considered quite effective. It becomes uninformative only in cases of fixed pathologies, when the hernia is localized near the esophagus. In such cases, pH measurement is performed.
- Fibrogastroduodenoscopy (FGDS). Using a fiber gastroscope, the doctor examines the esophagus, stomach, and duodenum. The diagnostic procedure is prescribed to almost everyone who suffers from intestinal and stomach diseases. If during the interview the patient indicated at least one of the characteristic symptoms, an FGDS becomes mandatory for diagnosis.
- pH measurement of the esophagus and stomach. The study is prescribed to determine the regularity of reflux of stomach contents into the esophagus. To determine the acid-forming gastric function, gastric juice is examined. The procedure is carried out using special equipment. A probe is inserted through the patient's nose and a skin electrode is installed. All changes are recorded on a block attached to the belt. The data is processed using a computer and special programs.
All diagnostic studies are performed on an empty stomach. The patient is advised to quit smoking and stop taking medications that may affect the results.
Treatment
Only a doctor can tell you how to treat a hiatal hernia. You should not allow serious complications to arise. If a person feels discomfort in the chest, then you need to visit a doctor, otherwise irreversible processes will begin.
In the initial stages, treatment is carried out at home and involves:
- taking medications;
- performing therapeutic exercises;
- following a strict diet;
- use of traditional methods.
Treatment for a hiatal hernia always begins with conservative measures. The patient is recommended to normalize weight and stop using tight belts. You should sleep with your head raised. You need to eat often, in small portions, and include a sufficient amount of fiber in your diet.
Drug therapy is aimed at preventing and treating the main complication – GERD. For this purpose, proton pump inhibitors are used in gradually decreasing dosages over a course of up to two months, followed by a transition to a short-term course of antacids. Treatment must include prokinetics (domperidone).
Surgical treatment of a hiatal hernia is indicated for the development of severe forms of gastroesophageal reflux disease; torpid reflux esophagitis, not amenable to conservative treatment; Barrett's esophagus (a precancerous condition that appears against the background of GERD).
Exercise therapy
Therapeutic gymnastics is aimed at strengthening the muscles of the anterior abdominal wall. The exercises are built on the same principle. All movements must be done while inhaling or exhaling. For example, the starting position is standing. Hands to the sides. The width of the legs is arbitrary. As you inhale, you should stick your stomach out. Don't overdo it. As you exhale, relax the front wall of the abdomen.
One more example. Lying position. As you inhale, turn your torso in one direction, and as you exhale, turn your body to the other. It is advisable to carry out such exercises every day. Accordingly, with severe symptoms, exercise therapy alone will not have the desired effect . Therefore, it is important to seek specialized medical help.
Treatment at home and lifestyle
The mechanisms of occurrence of hiatal hernia were described above. Taking them into account, we can provide recommendations that, if followed, will help reduce the risks of exacerbations:
- After any meal, you should not lie down for at least 1.5-2 hours. A reclining position on chairs is also excluded.
- Bend over should be avoided. If possible, it is better to put on your shoes using a stool and footrest. Washing floors - using a mop, excluding deep bends.
- Too heavy weights should be avoided. During the period of remission, it is permissible to carry a small weight, but always before meals or 40-60 minutes after meals.
- It is recommended to sleep on a bed with a raised headboard. If necessary, you can use a second pillow, but it is better if these are supports under the legs of the bed. This will allow you to completely raise the head end of the bed, and not just your head.
- Excess weight, flatulence, constant constipation, persistent cough - all those diseases, in the presence of which it will not be possible to effectively treat a hiatal hernia. Getting rid of diseases that increase intra-abdominal pressure will reduce the frequency of hernia exacerbations.
- Some medications relax the sphincter and make symptoms worse. Their use for esophageal hernia should be limited: Nifedipine, Diltiazem, Aspirin, Diclofenac.
Prevention
It is difficult to prevent the development of a hiatal hernia, but there are useful recommendations and advice from a gastroenterologist that will help reduce the risk of developing pathological changes:
- Control your weight, get rid of extra pounds.
- Do not lift too heavy loads yourself.
- Engage in moderate exercise that works your abdominal muscles.
- Do not strain during bowel movements.
- Do not tighten the straps too tightly.
It is necessary to strengthen the abdominal muscles, treat constipation in a timely manner, eat properly and rationally, and get rid of bad habits. If a patient has been diagnosed with a disease, clinical observation is recommended.
Medicines
Treatment of a hiatal hernia without surgery includes taking the following medications:
- Treatment with H-2 histamine receptor blockers (Nizatidine, Cimetidine, Roxatidine, Famotidine). They reduce acid production, which protects the esophagus from damage.
- Taking antacid medications (Rennie, Topalcan, Maalox, Gastal, Relzer, Almagel) or proton pump inhibitors (Omez, Emanera, Rabeprazole, Dexrabeprazole, Omeprazole, Esomeprazole). They bind acid from the stomach, reduce its irritating effect, and eliminate the symptoms of a hernia (including heartburn and pain).
- Treatment with prokinetic drugs (Cisapride, Motilium, Eglonil, Metoclopramide). They prevent reflux and normalize esophageal motility.
If concomitant complications of the gastrointestinal tract develop, the patient may be prescribed additional treatment methods. For example, if a complicated hiatal hernia is accompanied by internal bleeding, then hemostatic and antianemic drugs are prescribed.
Nutrition and diet
An increase in intra-abdominal pressure can provoke mechanical damage to the esophagus. All this is accompanied by intestinal obstruction and chronic constipation. These conditions can be corrected with proper nutrition. Diet for a hiatal hernia is a very important component of conservative treatment. It is also prescribed in cases where the patient is being prepared for surgery. The purpose of the diet is to reduce the acidity of gastric juice and protect the mucous membranes of the stomach and esophagus.
Meals should be fractional. It is best to eat small meals throughout the day. Last dose 3 hours before bedtime.
Products should not irritate the walls of the esophagus and cause heartburn. It is prohibited to eat very hot and, conversely, too cold food. Foods that cause stomach upsets and bloating are excluded from the diet.
| For hiatal hernia, the following are recommended: | Prohibited products include: |
|
|
A therapeutic diet and following a diet have a positive effect on the well-being and condition of the patient. The risk of developing complications dangerous to health is significantly reduced.
Folk remedies
Alternative medicine methods relieve the symptoms of a hernia and prevent its complications.
- The simplest remedy is chamomile or mint tea, which eliminates a burning sensation in the throat. The discomfort will disappear if you drink a cup of the drink after eating.
- A solution of apple cider vinegar will also relieve discomfort. It is prepared from 100 ml of water and 2 tsp. fruit component. Linden honey will enhance the effectiveness of the resulting composition.
- The mucous membrane will calm down under the influence of an infusion of 300 ml of water and 1 tsp. carrot seeds. The mixture must be brought to a boil, but not boiled. Drink warm once a day after breakfast. The course of treatment is a month.
- When the disease worsens, you can eat a handful of almonds.
- Heartburn will go away under the influence of ginger.
Folk remedies help cure the disease, but only mildly and at the initial stage. Their use must be coordinated with your doctor.
Useful video
How to cure a hiatal hernia? You can learn more about this issue using this interesting video.
Physiotherapy and traditional methods
All methods of physiotherapeutic treatment are symptomatic. These include the following:
- Pulsed electrotherapy . It is aimed at regulating the tone of the sphincter between the stomach and esophagus.
- Relief of inflammatory changes in the esophagus and stomach. UHF therapy is used as a method in this area.
- The methods are aimed at improving blood circulation and regenerative abilities. These include laser therapy .
- Methods that have an antispasmodic effect. Electrophoresis and galvanization are distinguished here .
Physiotherapeutic methods should only be used in a comprehensive manner.
How to treat a hiatal hernia at home? This can only be done in case of mild symptoms. Read about this in the article about non-surgical treatment of this disease.
Traditional methods are aimed at eliminating symptoms. If pain is severe, you should go to the hospital. Because complications may develop.
In case of severe heartburn, use a mixture of licorice. To do this you need to make a solution. Take boiled water, add licorice, and let it sit.
For pain syndrome, you can use chamomile flowers or plantain. Prepare everything according to instructions. If the pain does not go away, you should go to the hospital. Read more about traditional methods of treating diaphragmatic hernia here.
Source of the article: https://gastritunet.online/bolezni-pishhevoda/gpod/gryzha-pishhevoda-lechenie.html
Operation
Surgery for esophageal hernia can be performed either open or laparoscopically. Among the surgical methods of treatment, the most widespread are surgical interventions that are aimed at suturing the hernial orifice and strengthening the diaphragmatic-esophageal ligament (crurorrhaphy), fixing the stomach in the abdominal cavity (gastropexy), eliminating gastroesophageal reflux (fundoplication), and restoring the acute angle of His.
Contraindications to surgical treatment of esophageal hernias are concomitant pathologies that can cause severe complications in the postoperative period (for example, chronic cardiovascular diseases in the decompensation stage).
Since paraesophageal hiatal hernias are relatively rare, treatment tactics for this form of the disease have been less developed. In general, preference is given to surgical treatment of such hernias (primarily in young and middle-aged patients). For elderly people, especially in the presence of complications, it is recommended to adjust their lifestyle (in particular, limiting certain types of physical activity) and following a diet (excluding foods that contribute to the development of flatulence from the diet) in order to reduce the risk of hernia strangulation.
Surgical intervention
When a hiatal hernia is diagnosed, treatment should include surgery. It is indicated for any type of hernia.
There are indications for surgery:
- pronounced clinical picture in the form of pain;
- in case of complications development;
- if in combination with a hernia the patient has reflux that cannot be treated;
- for hernias with complications on the pulmonary system and heart;
- if the junction of the esophagus with the stomach, during biopsy takes on an uncharacteristic appearance of epithelium. That is, dysplasia develops, with subsequent metaplasia and cancer.
All operations are divided into 4 types.
- Surgical intervention according to Harrington and Alison . In the first option, after removing the hernial contents, the excess hernial sac is removed. In this case, a strip of peritoneum of about two centimeters remains on the esophagus. The esophagus is fixed to the corresponding hole in the diaphragm. Sutures are also placed on the legs of the latter. The cardia is also fixed to the diaphragm.
- The second option involves strengthening the diaphragmatic-esophageal ligament and the closing function of the cardia.
- Gastrocardiopexy . This method involves fixing the stomach and esophagus. The attachment itself occurs to the formations of the subphrenic space.
- Restoring the Hiss angle. All aspects of the operation are aimed at recreating a normal cardioesophageal area.
- Another direction is fundoplication. It is used in patients with GERD and a diagnosis of wandering hiatal hernia, the treatment of which, as you can see, is not easy.