Ovarian rupture or in medical terminology “apoplexy” (apoplexia ovarii) is a sudden outpouring of blood into an organ due to the rupture of a vessel, ovarian tissue, follicular or corpus luteum cyst, accompanied by a violation of the integrity of the organ and bleeding into the abdominal cavity.
Ovarian ruptures most often occur between the ages of 14 and 40, usually between 20 and 35 years. However, there are known cases of hemorrhage in young girls and adolescents. Its frequency among gynecological pathologies is 1-3%, relapse in the absence of adequate rehabilitation and recovery after surgery for apoplexy reaches 40-70%.
Ovaries: anatomy and functions
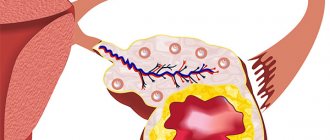
The ovaries are gonads (female gonads) and belong to paired organs. They are located in the small pelvis, in which they are attached by ligaments (mesentery and suspensory ligament of the ovary). One of the ends faces the fallopian tube (the egg released from the ovary immediately enters the tube). In appearance, the ovaries resemble peach pits and are furrowed with scars - traces of past ovulations, the formation and disappearance of the corpus luteum. The organs are small in size: 20–25 mm wide and up to 35 mm long. The weight of the ovaries reaches 5–10 grams. Blood enters the gonads from the ovarian arteries, and the right ovarian artery branches directly from the abdominal aorta, which is why its diameter is slightly larger, and the blood supply to the right organ is better. Accordingly, the right gland is larger in size compared to the left.
The functions of the reproductive gonads include the formation of estrogens and androgens (in small quantities), and most importantly, the production of an egg ready for fertilization.
Eggs are formed from follicles that were laid during the fetal development stage.
The female gonads consist of:
- germinal epithelium (covers the organ from above and delimits it from neighboring organs);
- tunica albuginea (consists of connective tissue and contains elastic fibers);
- parenchyma, which has 2 layers: outer (cortical) and inner (cerebral).
In the cortical layer of the gland there are immature and maturing follicles. Having reached a state of maturity (Graafian vesicle), the follicle protrudes somewhat above the surface of the gland and ruptures, from where the finished egg is released (ovulation phase). As the egg enters and moves through the tube, a corpus luteum is formed in place of the former burst follicle - the second stage of the cycle. The corpus luteum actively produces progesterone, which is necessary to support the onset of pregnancy. If conception does not occur, the corpus luteum undergoes a process of reverse development (involution) and becomes the white body (connective tissue), which eventually disappears completely.
The inner (brain) layer is located in the very depths of the glands and has a well-developed circulatory network and nerve endings.
Incidence rate
At the age of 18-45, women's bodies and ovaries work in a very active way. Therefore, the incidence of ovarian apoplexy occurs precisely during the childbearing period. But women of other ages are included in the statistics of this diagnosis. In terms of numbers, among other common gynecological diseases, ovarian apoplexy occupies 2% of the total. It is worth noting that if a woman has suffered such a disease once, the risk of recurrence increases to 70%. Apoplexy of the right ovary occurs 3 times more often than the left. This is a consequence of the fact that the largest number of blood vessels are located in the right ovary. In addition, the artery of the left ovary comes from the renal artery, and the right one comes directly from the aorta.
Definition of pathology and classification
The term “ovarian apoplexy” means hemorrhage into the ovary, which occurred suddenly against the background of a violation of the integrity (rupture) of the ovarian tissue. The disease is accompanied by progressive bleeding into the abdominal cavity and severe pain. Other names for the pathology are ovarian rupture or hematoma, less commonly, infarction. Hemorrhage into the gonad can occur when a cyst of the corpus luteum ruptures, when the vessels of the Graafian vesicle or the stroma of the organ are damaged.
The disease is divided into:
On forms:
- painful form (also called pseudoappendicular) - characterized by severe pain, which is accompanied by nausea and fever;
- anemic form (or hemorrhagic) - clinically similar to a ruptured tube during ectopic pregnancy, the cardinal symptom is intra-abdominal bleeding.
- mixed - the characteristics of both forms are combined.
Based on the amount of blood loss and the manifestation of clinical signs, the following degrees are distinguished:
- light (the volume of blood shed is 0.1 - 0.15 liters);
- average (blood loss is 0.15 - 0.5 liters);
- severe (free blood in the abdomen exceeds 0.5 liters).
Anemic and painful forms are diagnosed equally often.
Prevention
Prevention of ovarian apoplexy consists of minimizing factors that can provoke epididymal rupture. Women need to undergo gynecological examinations in a timely manner to identify polycystic disease and adnexitis.
You should not engage in strength sports that require heavy lifting; you need to protect yourself from various types of injuries. When prescribing anticoagulants, the dose of the drug should not be exceeded.
Causes and mechanism of development
The mechanism of development of the disease lies in neuroendocrine disorders and inflammatory processes of the internal genital organs. As a result of these factors, sclerotic changes develop in the ovaries, and blood stagnation in the pelvic vessels, which leads to varicose veins of the ovarian veins. Due to various changes in the vessels of the genital gonads (their varicose veins, sclerosis of the vascular wall), hyperemia and inflammation of the ovarian tissue, the formation of many small cysts, the walls of the ovarian vessels become defective, their permeability increases, which provokes further rupture of the vessel/vessels.
First, a hematoma forms in the ovary, which causes sharp pain as a result of increased pressure in the ovary. Then, due to excessive intraovarian pressure, the vessel/vessels burst, which leads to bleeding, often massive (even with a small rupture).
Ovarian apoplexy occurs in any phase of the cycle, but more often in the ovulatory and luteal (second) phases. During this period, blood flow to the gonads increases, the corpus luteum blossoms, and, possibly, the formation of a luteal cyst. The possibility of rupture of the corpus luteum in the first trimester of pregnancy cannot be ruled out.
It is characteristic that the right ovary ruptures more often, which is explained by its better blood supply compared to the left.
Causes
Reasons that create a favorable background for ovarian rupture (endogenous factors):
- inflammation of the ovaries/appendages;
- varicose veins of the ovary (provoked by heavy physical labor, repeated pregnancies, taking hormonal contraceptives, hyperestrogenism);
- anomalies in the location of the genital organs (retroflexion or bending of the uterus, compression of the ovary by a tumor of a neighboring organ);
- adhesions in the pelvis, especially when the ovary is constricted with adhesions;
- diseases of the blood coagulation system;
- sclerocystic ovary (the tunica albuginea becomes too dense, its rupture during ovulation “requires significant effort from the follicle”).
External causes (exogenous) that increase the risk of ovarian apoplexy:
- violent sex or interrupted sexual intercourse (blood flow to the gonads increases and intraovarian pressure increases);
- heavy lifting, sudden movements (bending, turning) or heavy physical work);
- abdominal trauma (blow, fall on the stomach);
- drug stimulation of ovulation (one of the side effects of clomiphene, which stimulates ovulation, is the formation of luteal cysts, which is fraught with apoplexy of the ovarian cyst);
- defecation (increased intra-abdominal pressure);
- horse riding (shaking);
- rough gynecological examination;
- visiting a bathhouse, sauna;
- long-term use of anticoagulants.
Case Study
A young woman, 22 years old, was admitted to the gynecology department at night with signs of intra-abdominal bleeding. Preliminary diagnosis after examination and abdominal puncture through the posterior vaginal fornix: “Apoplexy of the left ovary, mixed form.” The patient had a history of sclerocystic ovary disease and no pregnancies within a year of regular sexual activity (the patient recently got married). She was put on a waiting list for a paid laparoscopic operation for ovarian sclerocystosis at a regional hospital (the operation was scheduled a week after admission to our hospital). During laparotomy, liquid blood with clots up to 900 ml was found in the abdominal cavity, and a rupture of the right ovary of about 0.5 mm. Resection of both ovaries, sanitation of the abdominal cavity and layer-by-layer suturing of the wound were performed. The postoperative period was without complications, she was discharged in satisfactory condition.
The cause of ovarian rupture in this case was sclerocystic disease. The woman experienced, one might say, the first independent ovulation in her life, which led to rupture of the gland and bleeding. On the other hand, the patient did not have to go for a paid operation (resection of both ovaries was planned).
After 5 months, the woman registered for pregnancy in our antenatal clinic.
Clinical picture
Signs of ovarian apoplexy depend on the intensity of bleeding and concomitant (background) gynecological pathology. In the clinical picture, the prevailing symptoms of ovarian apoplexy are intra-abdominal bleeding and severe pain. In the case of a mixed form of pathology, signs of internal bleeding and pain are equally detected.
Pain
In most cases, pain occurs suddenly, its character is sharp, very intense, and often a painful attack is preceded by provoking factors (hypothermia, sudden movements, violent sex). It is also possible that pain may appear against the background of complete well-being, for example, during sleep. Occasionally, on the eve of an acute painful attack, a woman may notice a weak dull/aching pain or tingling in the left or right iliac region. Such aching pain is caused by small hemorrhages (hematoma formation) in the ovarian tissue, or by swelling or redness of the gland. The localization of the patient’s pain is often determined precisely, in the lower abdomen, right or left, and lower back pain is possible. Acute pain is explained by irritation of nerve receptors in the ovarian tissue, as well as blood spilling into the abdominal cavity and irritation of the peritoneum. Pain may radiate to the leg, under and above the collarbone, to the sacrum, anus or perineum.
Signs of internal bleeding
The severity of symptoms during intra-abdominal bleeding depends on the amount of blood spilled into the abdominal cavity, the intensity and duration of the bleeding. In moderate and severe cases (blood loss is more than 150 ml), signs of acute anemia come to the fore, and in severe cases, hemorrhagic shock. Blood pressure drops sharply, the patient feels severe weakness, and fainting is possible. The pulse quickens and weakens, the skin and mucous membranes become pale, nausea/vomiting appears, and signs of peritoneal irritation (peritoneal symptoms) appear. The patient complains of dry mouth, thirst, cold skin, with perspiration.
Other symptoms
Also typical for this pathology, but not always, is the appearance of minor intermenstrual bleeding or bleeding against the background of a delay in menstruation. The patient complains of frequent urination and the urge to defecate (irritation of the rectum due to gushing blood).
Gynecological and general examination
A general examination confirms the picture of internal bleeding (pale, cold and moist skin, tachycardia and low blood pressure, peritoneal symptoms, bloating).
A gynecological examination reveals: pallor of the mucous membranes of the vagina and cervix, a smoothed or overhanging posterior vaginal fornix (with large blood loss), a painful and enlarged right or left ovary. The uterus “floats” in the pelvis upon palpation, and displacement behind the cervix causes pain.
Diagnostics
Only in 4–5% is it possible to make a correct diagnosis, which is understandable. The signs of the disease are similar to the clinical picture of other pathological processes. Differential diagnosis is carried out with:
- interrupted ectopic pregnancy;
- acute adnexitis;
- rupture of an ovarian cyst;
- pyosalpinx and its rupture;
- appendicitis;
- renal colic;
- acute pancreatitis;
- perforation of a stomach ulcer;
- intestinal obstruction.
The patient's complaints are carefully collected and anamnesis is studied, a general and gynecological examination is performed, after which additional research methods are prescribed:
- UAC
A decrease in red blood cells and hemoglobin is determined (the degree of their decrease depends on the volume of blood loss), slight leukocytosis, and an increase in ESR.
- Coagulogram
- Pelvic ultrasound
Examination of the ovaries and determination of their size, taking into account the phase of the menstrual cycle and the condition of the other gland. The damaged ovary is somewhat larger in size; in its stroma, a hypoechoic or heterogeneous formation is detected - the corpus luteum. The diameter of the corpus luteum is not larger than the size of the maturing follicle, and the follicular apparatus of the gonad is normal (fluid inclusions up to 4–8 mm). Free fluid is visualized behind the uterus.
- Culdocentesis
Puncture of the abdominal cavity through the posterior vaginal fornix confirms/refutes the presence of liquid blood in the retrouterine space, which does not clot if the apoplexy is “fresh” or contains small clots – “old” bleeding.
- Laparoscopy
A minimally invasive intervention that allows not only to clarify the diagnosis, but also to carry out surgical treatment. During the inspection the following is revealed:
- blood poured into the abdominal cavity, without or with clots;
- an enlarged, purple ovary with a rupture that is either bleeding or blocked by a blood clot;
- normal sized uterus;
- inflammatory changes in the tubes (tortuosity, hyperemia, thickening, adhesions);
- pelvic adhesions.
In case of severe chronic adhesions or signs of hemorrhagic shock, laparoscopy is contraindicated and immediate therapeutic and diagnostic laparotomy is started.
Planning a pregnancy
Only in rare cases has apoplexy prevented pregnancy in the future. During the operation, only part of the ovary is removed and the organ is restored. After which it produces germ cells suitable for fertilization. If at the time of hospitalization the ovary was so damaged that it had to be removed, there is still a chance of getting pregnant.
At the same time, it is not always necessary to stimulate egg synthesis. Female reproductive cells are produced by a single ovary (preserved, healthy), and their quantity is sufficient for conception to occur.
Treatment
Treatment of the pathology is carried out in a hospital, since all patients are admitted with symptoms of “acute abdomen” and on an emergency basis. “Acute abdomen” requires not only careful diagnosis, but also monitoring of the patient’s condition. There are 2 options for treating the disease.
Conservative therapy
Conservative treatment is allowed for patients with minor blood loss (up to 0.15 liters) who have already achieved their reproductive function (they have children and are no longer planning to have children). The complex of treatment measures includes:
- Strict bed rest
The patient's movements can provoke and intensify subsided bleeding from the ovary, and also intensify the pain attack.
- Cold
All patients, immediately after diagnostic measures, are prescribed cold on the lower abdomen (rubber heating pad with ice), which causes vasospasm, stops bleeding and reduces pain.
- Hemostatic drugs
Also, to stop bleeding, hemostatic agents are administered: etamsylate, ascorbic acid, vikasol, vitamins B1, B6 and B12.
- Analgesics and antispasmodics
Baralgin, drotaverine, no-spa effectively relieve pain.
- Iron supplements
Prescribed for antianemic purposes (tardiferon, sorbifer, fenyuls).
Surgery
Surgery is performed either laparoscopically or laparotomically. Laparoscopic surgery is preferred, especially in the case of women who are planning a pregnancy in the future. Advantages of laparoscopic access:
- psychological comfort (no rough scars in the abdominal area);
- quick recovery from anesthesia;
- early activation of the patient;
- short hospital stay;
- less use of pain medications after surgery for ovarian rupture;
- low risk of adhesions and preservation of reproductive function.
Laparotomy is performed when the patient is in serious condition (hemorrhagic shock) and if it is impossible to perform laparoscopy (lack of equipment, significant adhesions in the abdominal cavity).
Stages of surgery:
- stopping bleeding (hemostasis) from a damaged ovary (coagulation, suturing the rupture or wedge resection of the gland is possible);
- removal of blood and clots from the abdominal cavity;
- sanitation (rinsing) with antiseptic solutions (aqueous solution of chlorhexidine, saline solution).
Very rarely it is necessary to perform an oophorectomy - complete removal of the ovary (in case of massive hemorrhage into the ovarian tissue).
Rehabilitation
After surgery for ovarian apoplexy, the patient undergoes rehabilitation measures:
Prevention of adhesions formation
Physiotherapy procedures are actively prescribed (starting from 3–4 days of the postoperative period):
- low frequency ultrasound;
- SMT;
- low intensity laser therapy;
- electrical stimulation of the fallopian tubes;
- therapeutic electrophoresis (with zinc, lidase, hydrocortisone);
- UHF.
Restoration of hormonal levels
Patients after ovarian rupture are recommended to take low-dose oral contraceptives for 1 to 3 months.
Dispensary registration
All women who have suffered ovarian apoplexy are subject to mandatory dispensary registration at the antenatal clinic for a year. The first examination is scheduled after a month, then after 3 and 6.
Forecasts
After suffering a painful form of ovarian apoplexy, quite good and favorable prognoses were revealed. In patients with hemorrhagic disease, the life prognosis will depend on rapid diagnosis and timing of treatment. Death from ovarian rupture occurs in decompensated irreversible hemorrhagic shock. It occurs with heavy blood loss (more than 50% of the blood volume).
Various measures to prevent the disease of ovarian apoplexy help reduce the frequency of relapses of this pathology.
Consequences
The prognosis in most cases after ovarian rupture (especially in the case of conservative treatment) is favorable. But the consequences cannot be excluded:
Adhesive process
Conservative therapy or delaying the timing of surgery in 85% of cases leads to the formation of adhesions in the pelvis. This is facilitated by the presence of blood and clots in the abdominal cavity, which eventually organize and cause the formation of adhesions. In addition, the occurrence of adhesions is provoked by the duration of the operation, an open wound of the abdomen (during laparotomy), the presence of chronic inflammation of the appendages and a complicated course of the postoperative period.
Infertility
Infertility develops in 42% of patients, which is facilitated by intense adhesions, hormonal imbalance and chronic inflammatory diseases of the ovaries and appendages. But if after apoplexy and surgery one healthy ovary remains, the chances of becoming pregnant in the future are high.
Relapse of the disease
Repeated apoplexy of both damaged and healthy ovaries occurs in 16% (according to some data in 50%) of cases, which is facilitated by background diseases (hormonal imbalance, chronic adnexitis).
Ectopic pregnancy
The risk of ectopic pregnancy increases due to the formation of adhesions in the pelvis, torsion and kinking of the fallopian tubes.
Complications
The consequences of ovarian apoplexy are adhesions, a high risk of developing peritonitis, and in some cases, adnexal cancer is possible.
With timely assistance, the patient’s life is not in danger, but if assistance is not provided on time, then extensive bleeding can lead to death.
In the future, women may lose reproductive function and suffer from an ectopic pregnancy.
Question answer
How long do you stay in the hospital after surgery?
As a rule, after surgery for ovarian apoplexy, patients stay in the hospital for 7–10 days. Early discharge is carried out after laparoscopic access and a smooth course of the postoperative period.
I underwent conservative treatment for 3 days in the hospital for a painful form of ovarian apoplexy. Laparoscopy was not performed, an ultrasound was performed and treated with hemostatic drugs. I was discharged with an improvement, but at home I again felt pain that radiated to the lower back and anus, plus the temperature rose to 37.5. What to do?
You need to urgently contact a gynecologist and possibly undergo laparoscopic surgery. All signs point to continued bleeding from the ovary and accompanying inflammation. In the event of an attack of acute pain, immediately call an ambulance.
When can you start having sex after surgery (ovarian rupture)?
In about a month.
Surgery
Operations for this pathology are the most common practice. Today, when the ovary ruptures, laparotomy and laparoscopy are performed. In the first method, an abdominal incision is made on the abdominal wall to gain maximum access to the organs. Similar operations are performed in any surgical department. The advantage of this type of intervention is a 100% overview of the internal genital organs.
After about a week, the stitches have healed and are removed. After another two to three weeks, if there are no complications, the woman is prepared for discharge. After two months, the patient fully recovers and can lead an active lifestyle.
The most modern method of surgical intervention is laparoscopy. This operation is performed through a small incision. The advantage of this method is quick rehabilitation (from 4 to 10 days). Not all institutions perform such operations. This technique is contraindicated in some forms of apoplexy.
After surgery (if the rupture is detected early), the woman retains reproductive function. Even if one ovary is removed, the second one can perform its function. The doctor will prescribe rehabilitation procedures (a course of hormonal medications, physiotherapy, etc.). At this time, pregnancy planning should be postponed. Doctors also advise abstaining from sexual intercourse for 1-2 months.