In today's article we will talk about such a disease as - tracheitis.
Tracheitis (lat. Tracheitis) is inflammation of the mucous membrane of the trachea.
Despite the fact that the trachea belongs to the lower respiratory tract, the ICD (International Classification of Diseases) classifies tracheitis as a disease of the upper respiratory tract.
ICD-10: J04.0, J42.
ICD-9: 464.1
According to the course of the disease, acute and chronic tracheitis are distinguished. Chronic is a complication of acute.
Tracheitis rarely occurs in isolation, most often it joins rhinitis, pharyngitis, laryngitis, bronchitis, forming rhinopharyngotracheitis, laryngotracheitis, tracheobronchitis.
Symptoms of tracheitis
The first signs of tracheitis and its symptoms depend on the type of infection and health status at the time of infection.
Symptoms of acute tracheitis
Symptoms of acute tracheitis usually appear following the development of acute inflammation of the overlying parts of the respiratory tract.
The most characteristic sign of tracheitis is a dry cough at night and especially in the morning, as well as coughing attacks when taking a deep breath, laughing, crying, or when the air temperature changes. During and after a coughing attack, a raw pain is felt in the throat and behind the sternum, as a result of which patients try to limit breathing movements. In such cases, especially in children, breathing becomes shallow and rapid. Even a small accumulation of sputum in the area of the tracheal bifurcation causes another attack of severe convulsive cough.
With concomitant laryngitis, the voice may be hoarse. Percussion and auscultation of mild deviations from the norm are usually not observed. The patient's general condition usually suffers slightly; body temperature is often slightly elevated, especially in the evenings. In children, the temperature can reach 39°.
The sputum is initially viscous, mucous in nature, and comes out with difficulty in small quantities. Gradually (starting from the 3-4th day) it becomes mucopurulent, more abundant, and comes off more easily: the pain when coughing becomes less intense.
Sometimes, simultaneously with the trachea, the inflammatory process affects the large bronchi and the clinical picture takes on the character of tracheobronchitis, in which the cough is more painful and constant than with tracheitis, and the body temperature is higher.
The most common complication of tracheitis and tracheobronchitis is the spread of the inflammatory process to the mucous membrane of the underlying respiratory tract. The development of bronchopneumonia (pneumonia in combination with bronchitis) in old age and bronchiolitis in children is especially dangerous.
Symptoms of chronic tracheitis
The main symptom of chronic tracheitis is a paroxysmal, painful cough, especially at night and in the morning, accompanied by pain in the chest. The sputum of a patient with chronic tracheitis in some cases may be scanty and viscous, in others – abundant and mucopurulent. However, despite its consistency, it almost always separates very easily.
The course of the disease in most patients is long, with exacerbations.
Other symptoms of tracheitis:
- burning behind the sternum; - general weakness; - headache; - difficulty breathing, worsening over time; - respiratory stridor - noisy breathing; - intercostal retractions (compression of the ribs during breathing); - varying degrees of respiratory failure; - sore throat, difficulty swallowing; - dysphonia (silence of voice).
First signs
Usually tracheitis begins according to a similar scenario with acute respiratory infections. First, the patient has a runny nose and a dry cough. A person may complain of weakness, sore throat, pain in the head. Hyperthermia up to 38-39 degrees can last up to 3 days, but sometimes it may not increase at all or rise to subfebrile levels of 37.5-38.0.
In young children, when tracheitis begins to develop, wheezing that can be heard at a distance may occur in the morning. Such wheezing usually goes away after the patient has cleared his throat. Shortness of breath with tracheitis, as a rule, does not occur.
Causes of tracheitis
The cause of tracheitis is the same infection that causes rhinitis, pharyngitis and laryngitis: staphylococci, streptococci, etc. In case of insufficient treatment (or lack thereof) of these diseases, the inflammatory process can spread to the trachea, causing tracheitis.
Causes of acute tracheitis
The most common cause of acute tracheitis is a viral infection, less often staphylococcus, streptococcus, etc. The development of tracheitis is promoted by inhalation of dry, cold or dusty air, irritating vapors and gases (paints, gasoline, other chemicals). In people prone to allergies, tracheitis can develop in a dusty room.
Causes of chronic tracheitis
Chronic tracheitis mainly develops from acute. It often occurs in people who abuse smoking and alcohol, as well as in cases of congestion in the respiratory tract due to emphysema, heart disease, and kidney disease. Chronic tracheitis is often caused by chronic inflammatory diseases of the nasal cavity and paranasal sinuses (rhinitis, sinusitis).
The main causative agents of tracheitis:
— Streptococcal species of bacteria, especially S pyogenes; - Haemophilus influenzae type B (Hib) (This cause is less common after the introduction of the Hib vaccine); — Representatives of the genus Klebsiella; — Representatives of the genus Pseudomonas; — Representatives of the genus Peptostreptococcus; — Representatives of the genus Prevotella; — Bactericides; — Anaerobes; - Moraxella catarrhalis (Recent research suggests that this is the main cause of bacterial tracheitis).
Bases classification
The classification is based on the etiological factor of the origin of the disease.
Depending on what microflora triggered the biomechanism of the pathological process, the following types of tracheitis are distinguished:
- Viral. A consequence of the penetration of viruses after suffering from influenza, acute respiratory infections or acute respiratory viral infections.
- Bacterial. Caused by the development of staphylococcal, streptococcal or pneumococcal infection.
- Mycotic. Occurs due to the ingress of a fungus of the genus candida.
- Allergic. Develops as a consequence of exposure to an allergen on the body.
- Mixed. The most dangerous, due to the fact that the disease occurs under the influence of several groups of microorganisms.
Taking into account the severity of the inflammatory process, tracheitis in adults can develop:
- Spicy. The disease is severe in both adults and children, with a large number of clinical symptoms.
- The chronic form does not have violent clinical manifestations, but its therapy requires a long time.
In turn, chronic tracheitis has two forms of the disease:
- Hypertrophic. The mucous membrane begins to grow and increase in volume, while the capillary network expands. The patient has a large amount of sputum produced.
- Atrophic. The mucous membrane becomes very thin, and small erosions or ulcers form on its surface. Because of this, this type of process received the second name erosive tracheitis.
Diagnosis of tracheitis
The diagnosis of acute tracheitis is based on the clinical picture, medical history, and the results of examination of the trachea using a laryngoscope.
When auscultating the lungs in the initial stage of tracheobronchitis, dry sounds are heard, later - silent moist small and medium bubble rales scattered throughout both lungs (mainly in the root and lower lobes).
Also, to diagnose the disease, the following may be prescribed:
— X-ray examination — Endoscopic examination
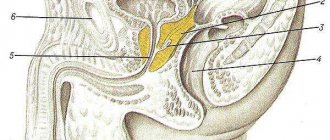
Briefly about the structure of the trachea
This organ is a hollow tube consisting of 16 - 20 cartilages, shaped like open rings. The trachea begins at the level of the sixth-seventh cervical vertebrae and ends with a branching (bifurcation) into the right and left main bronchi in the region of the fourth-fifth thoracic vertebrae. The total length in adults reaches 15 centimeters. The cartilages of the trachea are connected to each other by muscular and ligamentous apparatus. The open sections of the rings are facing backward, this is necessary for the free movement of the food bolus. Anatomically, the organ is divided into cervical and thoracic parts. In front of the trachea are the thyroid gland and the aortic arch, the largest blood vessel, and behind the esophagus, an organ necessary for the passage of food.
The inside of the trachea is lined with mucous membrane, and it is this area that is most often affected by the inflammatory process.
Treatment of tracheitis
Treatment of acute tracheitis
Treatment of acute tracheitis should be aimed, first of all, at eliminating the causative and contributing factors to the occurrence of tracheitis.
Without the use of antiviral drugs, treatment is mainly symptomatic: mustard plasters on the sternum and between the shoulder blades, antipyretic and anti-inflammatory drugs (Aspirin, Paracetamol), hot drinks in small sips, thermal inhalations.
Read also Pleurisy - symptoms, causes, types and treatment of pleurisy
For symptoms of intoxication or spread of the process to the underlying parts of the respiratory tract - sulfonamide drugs and antibiotics, incl. in the form of aerosols.
For a debilitating dry cough, Codeine, Libexin, and Glaucine are prescribed.
If there is difficulty in sputum discharge, use expectorants: thermopsis herb, marshmallow root, licorice, etc., as well as alkaline inhalations.
For purulent sputum, sulfa drugs and antibiotics are prescribed (preferably in aerosols).
If a viral infection is suspected (primarily influenza A and B), Remantadine is prescribed according to the following regimen: on the 1st day - 0.1 g 3 times a day, on the 2nd and 3rd days - 0.1 g 2 times a day, on the 4th day - 0.1 g 1 time a day after meals. Remantadine is more effective in the first days of treatment.
In cases of combination of tracheitis with acute pharyngitis, laryngitis, on the 1st-3rd days of the disease, a mixture of apomorphine hydrochloride, 1 tbsp. l. every 2-3 hours, use an infusion of thermopsis and marshmallow.
For an unspecified viral infection, Interferon is used in the form of repeated irrigations (0.6 mg per procedure) of the mucous membrane of the nasopharynx and trachea.
Inhalations. For inhalation, it is advisable to use a conventional steam or ultrasonic inhaler. At home or in the absence of an inhaler, for inhalation you can use a regular enamel pan in which 4-5 glasses of water are heated with the addition of various medications that cause a mild anti-inflammatory effect. For example: 5-10 drops of 5-10% iodine tincture, 1-2 tbsp. l. crushed eucalyptus leaves, 0.5-1 tsp. eucalyptus, menthol or anise oil.
To carry out inhalation, you can use a cone-shaped funnel rolled up from thick paper, the wide end of which is tightly covered with a pan, while the patient breathes through the narrow end of the funnel, inserted into the mouth. You can also breathe steam over the pan, covering yourself with a wide towel or sheet at a distance of 20-30 cm, keeping in mind that the greater this distance, the lower the temperature of the steam.
These thermal inhalations should be carried out for 5 minutes several times a day for 3-5 days.
In the treatment of acute and exacerbations of chronic tracheitis, propolis inhalations (bee glue) are often used. To prepare this inhalation, you need to place 60 g of propolis and 40 g of wax in an aluminum container with a capacity of 300 ml and place it in another larger container with boiling water. Breathe morning and evening for 10-15 minutes.
For the treatment of acute tracheitis, vitamin therapy is also indicated (vitamins A and 3 mg and 0.1 g, respectively, 3 times a day).
With timely treatment of uncomplicated acute tracheitis, recovery usually occurs within 1-2 weeks.
Treatment of chronic tracheitis
Treatment of chronic tracheitis is based on the same principles as for acute tracheitis. For purulent and mucopurulent sputum, broad-spectrum antibiotics are used:
— “Ampicillin” 2-3 g per day, course of treatment 1.5-3 weeks; - “Doxycycline” 0.2 g on the first day and 0.1 g in subsequent days, course of treatment 7-14 days).
Inhalations of garlic or onion phytoncides are indicated (garlic and onion juice is prepared before inhalation, mixed with a 0.25% solution of novocaine or isotonic sodium chloride solution in a proportion of 1 part juice to 3 parts solvent). Inhalations are carried out 2 times a day (for a course of 20 inhalations). Phytoncides also include “Chlorphyllipt”. A 1% alcohol solution is used internally, 25 drops 3 times a day.
Also, for the treatment of chronic tracheitis, expectorants of reflex action are indicated, which increase the secretion of the bronchial glands and dilute sputum.
Expectorants include copious alkaline drinks, a 3% solution of potassium iodide, infusions and decoctions of marshmallow, thermopsis up to 10 times a day, inhalation with a 2% solution of sodium bicarbonate.
Expectorants are used both during exacerbation of the disease and during remission.
Development of complications and prognosis
If the patient goes to a medical institution on time for medical care, the prognosis will be favorable. A wide selection of medicines allows for the completeness of the treatment process, and the disease does not become chronic.
The lack of proper therapy can be complicated by the development of the following pathologies:
- Bronchitis and pneumonia.
- Development of tracheobronchitis or bronchopneumonia.
- The appearance of symptoms of bronchial asthma with severe shortness of breath.
- In severe cases, tracheal stenosis may develop due to tissue swelling. This can disrupt the natural respiratory process, and surgical intervention will be required to resolve this situation.
The chronic form of tracheitis can cause the development of oncopathology (neoplasms of an endotracheal or endotracheal nature). The development of such a problem does not always have a favorable prognosis.
Folk remedies for treating tracheitis
1. Radish with honey.
When treating tracheitis, black radish juice with honey in a 1:1 ratio is very helpful. Drink it one tablespoon 3 times a day after meals. To prepare, you need to cut out the core of the radish and put honey in it. The radish will release juice, and in a few hours the mixture will be ready. 2. When symptoms of laryngitis and tracheitis appear, it is useful to breathe in onion or garlic pulp wrapped in gauze.
3. It is beneficial to drink ½ glass of freshly prepared carrot juice 2-3 times a day.
4. You can gargle with infusion of onion peels. Pour 2 tablespoons of husks into two glasses of boiling water, leave for 2-4 hours in a thermos and gargle with the infusion several times a day.
5. Rinsing raspberry leaves with tincture is effective (pour 2 tablespoons into 0.5 liters of boiling water in a thermos, leave for 1-2 hours).
6. You can gargle with calendula tincture (1 - 2 teaspoons per glass of warm water).
7. A decoction of eucalyptus leaves is suitable for both inhalation and oral administration (infuse 2 tablespoons of eucalyptus leaves in a thermos in 0.5 liters of boiling water for 1-2 hours). Gargle several times a day, and drink 2 tablespoons 3 times a day after meals, warm.
8. Inhalation of potato steam, inhalation and drinking herbal decoctions have an anti-inflammatory and softening effect: chamomile (2 tablespoons per 0.5 liters of water), plantain (2 tablespoons per 0.5 liters of water), marshmallow root (2 tablespoons per 0.5 liters of water). .5 liters of water). You can breathe these decoctions by covering yourself over a saucepan with the decoction; you can drink ½ cup 3 times a day before meals.
9. Inhalations with propolis. To do this, place 40 g of wax and 60 g of propolis in an aluminum bowl and place it in a water bath. Breathe for 15 minutes twice a day.
Read also Zika virus. Symptoms, causes, infection and prevention
10. Mix eucalyptus leaves, sage, chamomile flowers, mint herb and pine buds. Pour the resulting mass with a glass of boiling water and place in a water bath for 30 minutes, then pour into the inhaler. Inhale the vapors for no more than 15 minutes.
11. The following recipe is effective: crush 5-6 cloves of garlic and boil in a glass of milk, cool and drink 1 teaspoon several times a day.
12. For hoarseness, freshly prepared cabbage juice 30-40 minutes before meals, 3-4 times a day, helps well, start with ½ glass and increase to 1 glass.
13. For tracheitis, expectorant and phlegm-thinning plants are useful: coltsfoot leaves, licorice root, yarrow herbs, elecampane, string, thyme, marshmallow root. To prepare, take 2 tablespoons of any of the indicated medicinal plants, and pour 0.5 liters of boiling water in a thermos, leave for 1-2 hours, filter and drink ½ cup 2-3 times a day 30 minutes before meals (drink licorice root infusion 2 tablespoons 3-4 times a day).
14. It is useful to sew a pillow, stuff it with dried thyme and hang it near the head of the bed. Thyme essential oils soothe coughs and sore throats.
15. At home, to prepare an aqueous infusion, pour 2 tablespoons of crushed dry marshmallow roots into 1 glass of cold boiled water and leave at room temperature for 30 minutes, stirring occasionally. Then the liquid is drained without squeezing out the sediment, filtered through several layers of gauze and cold boiled water is added to 200 ml.
16. People use marshmallow root powder prepared for future use. It is mixed with warm water until it becomes thick sour cream. The resulting suspension is filtered and taken 1 tablespoon 2 times a day.
17. A very effective decoction for the treatment of tracheitis is an infusion of the following mixture: 10 parts of creeping thyme, dill and mint seeds, 15 parts of plantain and licorice root, 5 parts of sweet clover and 20 of coltsfoot. 4 tbsp. pour boiling water (800 ml) over the crushed mixture, leave for 1 hour and strain. Drink warmed to 40°C with 200 ml honey. Drink 2-3 servings per night.
18. In folk medicine in many countries, advice on how to treat tracheitis includes a recipe for a decoction of buds or young shoots of pine. To do this, 15 buds are boiled in 250 ml of water. And take a hot decoction 4 times a day. You can add 10 g of cinnamon, 5 g of cloves and 1 nutmeg here.
19. Egg mixture. You need to boil a glass of milk, add a tablespoon of honey and butter, a well-beaten yolk and ¼ tsp. soda Drink at night.
20. If you have a chronic form of the disease and you are constantly wondering how to cure tracheitis, then try using compresses made from a mixture of honey, sunflower oil, dry mustard and flour. You need to take a tablespoon of each ingredient. And add 1.5 tbsp. vodka. Mix everything and heat in a water bath. Place the mixture in gauze and apply a compress to the area where it hurts the most. Secure with polyethylene and a warm scarf. Repeat the procedure for several days in a row.
21. Tracheitis in children: treatment with potato compresses. Boil two potatoes in their skins, mash them hot, add a tablespoon of vegetable oil, apply to the chest, cover and keep until cool.
22. Traditional medicine recommends treating allergic tracheitis with an infusion of blackberry leaves and fruits. For this, 2 tbsp. Pour half a liter of boiling water over the mixture and let it brew for 1 hour. Drink the strained solution instead of tea.
Sprays
They are especially effective at the initial stage of the disease. The best sprays for irrigation are:
- "Inhalipt." Reduces soreness and burning in the throat.
- "Hexasprey". Has an anti-inflammatory effect, eliminates irritation.
- "Tantum Verde forte." Moisturizes and softens the throat, produces a slight analgesic effect.
- "Kameton." Makes breathing easier and has an antiseptic effect.
Two injections three times a day are enough. The effect of each spray reaches 6 hours.
Tracheitis in a child
The causes and symptoms of tracheitis in children are the same as in adults.
The only difference is the treatment methods for this disease. The fact is that a child’s body, unlike an adult’s, is not yet fully developed and is going through its formation stages, so incorrect diagnosis and subsequently selected medications for the treatment of tracheitis in a child can harm the baby’s health. After all, drugs for adults can be strong for a child and have a negative impact on the further development of the baby.
Therefore, first of all, treatment should be carried out under the supervision of a doctor.
The main task of the doctor and parents when treating tracheitis in children is to increase immunity and replenish the body with vitamins.
You should absolutely not take any medications, especially antibiotics, without a prescription.
To overcome a cough, the baby will be prescribed syrups and decoctions (licorice root syrup, stoptussin, chest tea), gargling, inhalations with herbs and essential oils, and warm, preferably alkaline, drinks. Tea with viburnum, raspberries, linden, hot milk with honey helps well. If the child is very small, gargling will not work. In this case, it is necessary to give the baby warm herbal tea, and the more often the better. It is also recommended to take vitamins A and C daily three times, which help improve immunity.
In addition, when treating tracheitis, antiviral aerosol drugs are prescribed.
For tracheitis, rubbing the baby’s chest with “Zvezdochka” or “Doctor MOM” balms helps. The procedure should be carried out twice a day. One of the rubbings is best done at night.
Rubbing can be done daily, starting from the first days of the disease, and inhalations, which will be discussed later, are used no earlier than the third day from the onset of the disease.
Steam inhalation is a very effective way to combat tracheitis. But, if the baby is very small, then classical inhalation will not be possible. In this case, you can find a way out: put a saucepan with water and other ingredients on the gas, close the door to the kitchen, take the baby in your arms and stand with him for 10 minutes near the boiling broth. If the child is over two years old, you can do classic inhalations.
Read also Warts. Description, causes, prevention and treatment of warts
Here are a few options for what might be included:
1. Honey inhalation is very effective and promotes recovery in the shortest possible time. To prepare it, 10 gr. flower honey, dissolve it in water, add 5 ml. calcium chloride. The mixture must be heated in a water bath. The child must breathe these fumes for at least 7 minutes.
2. Iodine + eucalyptus. For this option, you need five glasses of water, 25 drops of iodine, two tablespoons of eucalyptus leaves or sage herb. You can add one teaspoon of anise oil. The inhalation time, as in the previous case, is about 5-7 minutes.
3. Tea tree inhalation. Take a cup of hot water and add 5 drops of tea tree oil. Ask your baby to breathe in the steam.
To treat tracheitis, warm compresses are successfully used, which should be applied to the sternum and between the shoulder blades, as well as mustard foot baths.
Other activities that are carried out to reduce the disease and speed up recovery include:
— Frequent wet cleaning;
— Air humidification (dry air dries out the mucous membrane and only aggravates the condition). You can use a humidifier for this.
- Ventilation.
In addition, you can use a salt lamp as a night light. In addition to lighting, this device can also have a beneficial effect on the indoor microclimate.
For chronic tracheitis, climatic treatment is often recommended, that is, treatment in sanatoriums, at sea, with maximum exposure to the fresh air.
Comments (7)
Nadia
01/04/2017 at 15:33 |
If you consult a doctor in time, you will recover faster. When I was diagnosed with tracheitis, I was prescribed nebulizer inhalations with Prospan drops. Treatment began immediately. This way the throat softens and the dry cough goes away.Answer
Elena
10/30/2018 at 10:19 |
Three years ago in the fall I got very cold and got sick, and that’s when I started getting tracheitis. At first I treated myself, but then I turned to an ENT specialist and she told me to drink Sumamed and do inhalations.
Answer
Igor
04/20/2019 at 00:29 |
I usually treat such a cold, if there is no fever, with ambroxol and licorice root syrup. I use these two products at the same time. The annoying cough, however, goes away within a week.
Answer
Sonya
07/02/2019 at 11:40 |
Hypothermia of the body during the cold season is not uncommon, as well as a manifestation of pharyngitis, laryngitis and other similar diseases. Traditional medicine cannot cure such a disease, only antibiotics.
Answer
Expert Marina Rusetskaya
07/02/2019 at 13:23 |
Sophia - laryngitis and pharyngitis are treated with antibacterial drugs only when a bacterial infection is associated.
Colored deposits on the mucous membrane of the tonsils or yellow or green sputum help determine the bacterial nature of the disease.
But, if sputum comes out, this indicates that the inflammatory process has descended into the lower respiratory tract.
In other cases, inhalation gargling and sucking medicinal lozenges and lozenges are sufficient.
If you have laryngitis, it is still important not to talk.
In severe cases of laryngitis (loss of voice), patients are prescribed inhaled glucocorticoids.
Important factors in complex treatment are plenty of warm drinks and home regimen.
It happens that laryngitis and pharyngitis are symptoms of a viral infection.
In these cases, the first sign is an increase in body temperature to 38 C˚ or higher; you need to take an antiviral drug, preferably in the first hours after the body temperature rises.
Answer
Galina
04/13/2020 at 06:14 |
Of course, it is imperative to find out the cause of the cough and get treatment.
Answer
Olga
04/13/2020 at 07:49 |
Galina, everything is exactly right. My cough itself was simply terrible (It’s good that the doctor prescribed Fluifort granules for me. I diluted it according to the instructions and took it. Now the cough doesn’t bother me, I cured it.
Answer
Tracheitis during pregnancy
During pregnancy, a woman’s body is weakened and susceptible to infections and viruses, which is why they often experience inflammation of the tracheal mucosa.
Symptoms of tracheitis in pregnant women are the same as in all people, but treatment differs in its duration and complexity due to the limited use of medications. Tracheitis in pregnant women is dangerous because the virus or infection can be transmitted from the expectant mother through the placenta to the baby. Advanced tracheitis can undermine the health of an unborn child and complicate childbirth. The peculiarity of this disease in pregnant women is that it often leads to bronchitis due to the “descent” of the disease from the trachea into the bronchi. To prevent this from happening, tracheitis must be diagnosed and treated in time.
Tracheitis during pregnancy is also dangerous because during a strong cough, the front wall of the abdomen tenses, and this is undesirable for a pregnant woman, so tracheitis must be treated, and the cough must be made less intense and painful.
Treatment of tracheitis during pregnancy
Important! If you have symptoms of tracheitis during pregnancy, be sure to consult a doctor, and do not self-medicate, so as not to harm your health or the health of your unborn child!
If pregnant women become ill with respiratory infections, in particular tracheitis, they need to rest more in the first days. It is advisable to ventilate the room frequently and carry out wet cleaning twice a day. At the onset of the disease, it is allowed to take interferon-based antiviral agents.
In the treatment of tracheitis, drugs that relieve cough are of great importance, because this is one of the main and painful symptoms of tracheitis. To reduce the intensity of cough, steam or ultrasonic inhalations with saline, soda, mineral water, garlic or onions are performed.
As a rule, warm and frequent drinks are prescribed (milk with soda or Borjomi, hot tea with honey or lemon, linden and other teas, fruit drinks, compotes, milk). Dairy and vegetable products should predominate in the diet.
At the same time, there is a need to prescribe expectorant medications that can thin the mucus and facilitate its elimination.
Expectorants used for pregnant women can be divided into two groups:
- reflex-action drugs, so-called secretomotor substances (sodium bicarbonate, ammonium chloride, sodium iodide, thermopsis, ipecac, terpine hydrate). Of these drugs, it is recommended to take thermopsis mixture, since it does not cause any side effects at any stage of pregnancy;
- mucolytics. These products include Ambroxol (Trisolvin, Ambrosan), Bromhexine (Mucodex, Phlegamine, Bisolvon).
High fever in pregnant women is reduced by physical methods (wiping with a damp sponge, cool shower, cold on the area of large vessels); if these are ineffective, the use of paracetamol is allowed.
From traditional medicine, it is recommended to use a decoction of marshmallow root to suppress cough.
Antibacterial drugs in the treatment of this disease are not recommended for pregnant women. However, they can be prescribed if there is purulent sputum. Therefore, in the first trimester, semi-synthetic penicillins, for example, Amoxicillin, are usually prescribed. From the beginning of the second trimester, macrolides (Vilprafen, Azithromycin, Rovamycin) and cephalosporins (Cefuroxime, Kefzol) are prescribed.
The general condition is alleviated mainly with the help of symptomatic means. For nasal congestion, perform a nasal douche using saline or sea salt solution. In case of discomfort in the throat, gargle with herbal decoctions (chamomile, sage, oak bark).
Medicines
Photo: m.mcdn.fr
The choice between antibacterial and antiviral agents depends on the etiology of the disease. This or that group of antibiotics is prescribed depending on the type of harmful bacteria that caused the development of tracheitis. The duration of the course and the frequency of administration are indicated by the doctor. It is important to follow all doctor’s recommendations regarding the use of an antibiotic, since stopping treatment earlier or independently changing the frequency of administration can lead to the development of chronic tracheitis.
Antipyretics help in the fight against fever. The most commonly used is ibuprofen, which is available not only in the form of tablets, but also in the form of a suspension, which is especially important when prescribed to children. In addition to its antipyretic effect, ibuprofen has analgesic and anti-inflammatory effects. The drug is well tolerated and rarely causes side effects. People with peptic ulcers of the stomach and duodenum in the acute phase, severe insufficiency of liver or kidney function, severe heart failure, blood diseases (hemophilia, hemorrhagic diathesis), and women in the 3rd trimester of pregnancy should be treated with caution.
For painful coughs, antitussives are prescribed. There are many names of antitussive drugs that are prescribed in cases where the cough reaction is not due to the need to remove secretions (sputum).
Expectorants are used to improve mucus discharge. Ambroxol is one of the representatives of this group. It should not be taken together with antitussives, as this leads to difficulty in sputum discharge due to a decrease in cough. Rarely, the following side effects occur while taking ambroxol: nausea, vomiting, diarrhea, dyspepsia. Most often, the drug is well tolerated and does not cause any discomfort.
The most commonly used antihistamine is loratadine. The effect of the drug is to reduce capillary permeability, thereby preventing the development of tissue edema. It does not have a central effect, that is, it does not penetrate the blood-brain barrier, due to this there is no risk of developing addiction to taking the drug.
Prevention of tracheitis
Prevention of both acute and chronic tracheitis is aimed at timely elimination of the causes of tracheitis, strengthening the body, especially for persons predisposed to acute diseases of the upper respiratory tract.
Hardening the body, reducing dust and gas pollution in the air (use of air purifiers) are of great importance.
Also try to avoid both active and passive smoking.
In addition, avoid prolonged hypothermia.
Maintain cleanliness and basic hygiene at home.
Try to walk more in the fresh air and spend your free time actively.
Eat foods rich in vitamins and minerals. By the way, you can also cook food in a double boiler. With this method of preparation, products lose the least amount of vitamins.
Self-determination of the disease
Many people wonder: how to determine whether tracheitis is viral or bacterial? It is difficult to do this on your own, since the symptoms are similar, and the patient is in such a state that it is difficult for him to analyze the signs, to put it mildly.
However, a disease of bacterial origin is potentially more dangerous than a viral disease. It is caused by meningococcus, pneumococcus, staphylococcus and other parasitic microbes. And since they, developing and multiplying, release toxic substances, a person develops symptoms of intoxication. In addition to all of the above:
- Problems with stool.
- Stomach ache.
- Decreased appetite.
- Strong increase in temperature up to 40 °C.
- Dehydration.
- Hallucinations and febrile seizures (in children).
Here, however, is how to understand whether viral or bacterial tracheitis has overcome a person. If there is intoxication, then the second option is more likely. And this is dangerous, since bacteria can provoke purulent inflammation of the trachea. This phenomenon is fraught with a retropharyngeal abscess.
It is also useful to know that there is fungal tracheitis (manifested by intoxication and swelling of the trachea) and chronic, in which there is no discomfort in the throat, but there is inflammation. A once untreated disease takes this form.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 521 | 1003 | 2863.4 | 3561 | 3561 | 3561 | 3561 | 521 | 1003 | 2863.4 | 3561 | 3561 | 3561 | 3561 |
Physiotherapy
In order to minimize the risk of complications, and also speed up the recovery process, you will need to undergo procedures. As a rule, doctors recommend the following:
- Electrophoresis.
- Inductothermy.
- Exposure to an electromagnetic field.
- Steam inhalations.
The last procedure listed can be done at home. It is better to use herbal infusions rather than water. The best raw materials for their preparation are eucalyptus, elecampane rhizome, sage, pine buds, thyme, chamomile and mint. Their action for tracheitis is irreplaceable.
By the way, you can also add essential oil to the inhalation composition. The best ones are cajeput, mint, juniper, eucalyptus, clove, cedar, rosemary, pine, ginger, fir, anise or sage.
Compliance with the regime
To recover faster, you need to change your lifestyle at least temporarily. Here are the main recommendations for patients:
- It is necessary to maintain indoor humidity at a minimum of 55%.
- Drink plenty of fluids. These can be teas, juices, compotes, fruit drinks.
- No smoking. This further irritates the already inflamed airways.
- Do not eat pickled, salty or spicy foods.
- Try not to strain your vocal cords.
If you start treatment on time, take medications prescribed by your doctor, and follow the regimen, you will be able to get rid of tracheitis in 7 days.
Pathogenesis
Pathogenic microorganisms and irritants cause catarrhal inflammation of the trachea. Pathogenetic links of the process:
- Destruction of the ciliated epithelium,
- Development of local inflammation,
- Release of biologically active substances into the blood,
- Dilation of blood vessels, increasing their permeability,
- Swelling of the tracheal tissues,
- The release of plasma into the intercellular space and the formation of exudate,
- The appearance of a viscous secretion in the lumen of the organ,
- Irritation of nerve endings
- Dry hacking cough,
- Intense vibration of the esophagus, leading to vomiting,
- Constant irritation of the mucous membrane and worsening inflammation,
- Violation of drainage and ventilation functions,
- Accumulation of viscous sputum,
- Decreased local immunity,
- Addition of severe complications.
Pathological signs of the disease:
- Infiltration of the tracheal mucosa,
- Hyperemia and edema of the ciliated epithelium,
- Accumulation of mucus
- Ecchymoses are small hemorrhages.
Acute tracheitis is characterized by a sudden onset and pronounced symptoms. It lasts 7-10 days and usually ends with recovery. In severe cases, if left untreated, the process becomes chronic. The outcome of the pathology depends on the form and intensity of inflammation, the functional activity of the immune system, the presence of serious underlying diseases in patients, the adequacy, timeliness and effectiveness of therapeutic measures.