Gonorrhea is an infectious disease caused by gonococci. It can be successfully treated with antibiotics if diagnosed early. Without adequate therapy, it threatens the development of complications, including death. It is one of the most common sexually transmitted infections. Every year, about 60 million new cases of this dangerous disease are recorded worldwide.
Gonorrhea is one of the most common STIs
How is gonorrhea diagnosed in women?
When a case of gonorrhea is identified, it is necessary to examine people who had sexual contact with the patient within a month before the patient developed symptoms of infection. If there is an asymptomatic course of the disease, it is necessary to examine those who had sexual intercourse with the patient in the last two months before diagnosis. Also, everyone who was in everyday contact with the patient should be involved in the examination. In addition, it is necessary to pay special attention to the health status of children of sick women. Sick personnel are not allowed to work.
Frequently asked questions to the doctor
The selection of drugs should be carried out individually
How much more?
Hello. A few days ago I began to experience unpleasant symptoms, which prompted me to visit a dermatovenerologist. The doctor diagnosed me with acute gonorrhea and prescribed treatment. I take all medications as recommended, but the symptoms do not go away. What could this mean?
Hello. Treatment of gonorrhea is a rather labor-intensive process, but if no positive results are observed after 5-7 days of therapy, several options can be suspected: either the pathogen is highly resistant to the antibiotic prescribed to you (in this case, you need to take an antibiotic sensitivity test and choose another drug), or you forgot that your sexual partner also needs to be diagnosed with gonorrhea, and possibly treated, as a result of which there is likely to be constant contact with the pathogen and re-infection.
The causative agent of gonorrhea
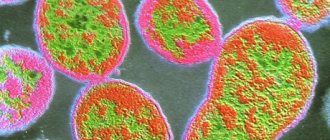
The causative agent of gonorrhea is the gram-negative bacterium Neisseria gonorrhoeae, which belongs to paired cocci and has a bean-shaped shape. Gonococci are located inside cells, within the cytoplasm of leukocytes. These organisms are characterized by increased sensitivity to various external factors. They die when the temperature rises to just 55 degrees. Also harmful to them is exposure to sunlight and drying out. Treatment with antiseptic solutions gives a good effect. The bacterium remains viable in fresh pus. After it dries, the gonococcus dies.
The causative agents of gonorrhea are not able to move, they do not form spores. These organisms have very thin threads, thanks to which they can be held on the surface of epithelial cells, red blood cells, and male germ cells - sperm.
On top, each bacterium is covered with a layer of a special substance and is, as it were, located in a capsule. Therefore, the destruction of such organisms is difficult. Treatment is complicated by the fact that the pathogen can be located inside epithelial cells, Trichomonas and leukocytes.
If the course of treatment was prescribed incorrectly, special forms of the pathogen may appear - L-forms. They differ from typical organisms in a number of biological and morphological characteristics. L-shapes have the appearance of a ball, their color and size can vary. Such gonococci do not show sensitivity to the antibacterial drug that provoked their formation. This is due to the fact that they have partially lost their antigenic properties. The presence of such forms interferes with correct diagnosis and greatly complicates antibacterial therapy. The infection remains in the body due to its transformation into vegetative forms. After many years of using antibiotics to treat gonorrhea, many strains have emerged that are capable of producing lactamase. They have become resistant to drugs that contain a lactam ring.
The first signal of a sexually transmitted disease
Gonorrhea begins to appear a week after infection. The first signs can be confused with minor illnesses.
- Discharge, itching. They are confused with thrush, so treatment is often carried out at home without a doctor’s advice. The result is complications of gonorrhea.
- Spasms in the lower abdomen and pain when urinating. These manifestations are similar to those of cystitis.
Inattention to health can play a cruel joke. The peculiarity of gonorrhea is the erased symptoms. The first signs of gonorrhea in a female should be noticed by her herself, otherwise, if the pathological process is ignored, her health may significantly deteriorate.
After infection, discharge appears. This is the first call of the disease. They will be yellow or light colored with a foul odor. Due to the similarity of symptoms with thrush, women are in no hurry to receive treatment, aggravating the picture.
If there is cervical erosion, the incubation period of the disease will be shortened. This is also facilitated by rectal cracks, candidiasis, and mucosal damage.
Gonorrhea in girls is always acute. The symptoms are pronounced - there is swelling of the vagina, mucous membranes, itching, burning. There is purulent discharge and pain when emptying the bladder.
Ways of transmission of gonorrhea
Most often, infection with gonorrhea occurs through sexual contact. Moreover, for men the contagiousness is 25-50%, and for women this figure is higher (up to 50-70%). Cases of household transmission of infection are not recorded very often. In everyday life, rare causes of infection are usually towels, linen, washcloths, etc. Girls are at greater risk of household infection than boys. Facts of intrauterine infection have not been confirmed. During natural childbirth, the child may become infected from a mother infected with gonococcus.
Timing of the onset of the first symptoms after infection
The incubation period of infection lasts from 3 – 7 days to 2 – 3 weeks. Accordingly, the first signs of the disease, as a rule, appear after 5 days. The shortening or lengthening of the incubation period depends on the body’s defenses.
If the immune system is very weakened, then the first symptoms of the disease will appear within 24-48 hours (recently suffered a severe infectious disease, treatment with steroids, chemotherapy, etc.).
Late manifestation of gonorrhea is associated either with good immunity, or with taking antibiotics for other infections after infection, or with an attempt at self-medication. This, and not only, is due to the fact that the first symptoms of gonorrhea are almost invisible.
Pathogenesis of gonorrhea
Most often, the infection develops in the mucosa of the cervical canal, fallopian tubes, urethra, large vestibular and paraurethral glands. That is, areas that are lined by columnar epithelium are susceptible to damage.
After oral-genital sexual intercourse, the development of gonorrheal stomatitis, tonsillitis or pharyngitis is possible. As a result of anal contact, gonorrheal proctitis cannot be ruled out. If the infection gets into the eyes (for example, during childbirth, when the baby passes through the birth canal of a sick mother), gonorrheal conjunctivitis is possible.
The walls of the vagina are less susceptible to the development of an infectious process, since they are covered with stratified epithelium. However, in children, mature women and pregnant women, the epithelium may thin out or become loose. In such cases, there is a risk of gonorrheal vaginitis.
Thanks to the presence of threads (piles), pathogens that enter the body attach to epithelial cells. Then the bacteria penetrate into the cells, intercellular gaps and the space under the epithelium. Because of this, the epithelium begins to collapse and an inflammatory process occurs.
In the genitourinary tract, the spread of infection goes from the lower to the upper sections. When gonococci are fixed on sperm and with enterobiasis inside Trichomonas, progress occurs more quickly.
There are cases when gonococcus penetrates the bloodstream. But this happens infrequently, since the serum has a bactericidal effect. If this happens, then the infectious process generalizes and foci of the disease arise in other parts of the body. The joints are usually affected. Complications in the form of gonorrheal meningitis or gonorrheal endocarditis are also possible.
When a gonorrheal infection enters the human body, antibodies begin to be produced. But immunity is not lifelong and is not very effective. You can become infected and get sick again. This is most likely due to the fact that gonococcus is characterized by antigenic variability.
Myths about gonorrhea infection
And a little about the myths that men come up with for their wives or girlfriends to justify themselves when they are diagnosed with a gonococcal infection.
Myth 1 – I used a friend’s washcloth in the bathhouse
This is impossible. Gonorrhea in most cases is transmitted from a sick person to a healthy person through sexual contact, regardless of the nature of sexual contact (genital-anal, traditional, petting).
Myth 2 – I got infected in a public toilet by sitting on the toilet
Also impossible, for the same reason. There are descriptions of cases of “household infection”, but the reliability is highly doubtful; it is almost impossible to “pick up” live gonococcus in the toilet. Another possible route of infection with gonorrhea other than sexual contact (this applies only to women) is transmission of the infection from a sick woman to a child at birth.
Myth 3 – Bitten by a street stray dog
Infection from animals is impossible. Neisseria canis can be found in dogs; this pathogen is the closest relative of the human gonorrhea pathogen Neisseria gonorrhoeae, but dogs do not get real gonorrhea.
Myth 4 – I donated blood from a vein at the clinic and became infected
Impossible. The causative agent of gonorrhea quickly dies outside the human body, it is extremely unstable in the external environment, dies when exposed to direct sunlight and heated to 56C. When blood is drawn in medical institutions, disinfectants are used, which has a detrimental effect on the gonorrhea pathogen. Gonococcus does not tolerate temperatures below 36C (human body temperature), and dies at 18C.
Myth 5 – I drank a drink, beer, coffee from someone else’s mug
This is impossible; you cannot become infected with gonorrhea either through drinking, eating or sharing utensils.
Myth 6 - I ride the subway every day, dirty handrails mean a lot of infections
This is impossible. The causative agent of gonorrhea is capable of life only in a humid environment; if the external environment is dry, it dies. This instability of the bacterium in the external environment explains that the likelihood of infection through any objects is very unlikely; for further life it requires only a human body, so its transmission is possible only through close direct contact with the source of infection - a carrier of gonorrhea, a sick person.
Myth 7 - I had a girlfriend before you and I “got” gonorrhea from her
This explanation is possible if the man recently had a “ex-beloved girlfriend”. The first symptoms of gonorrhea appear during the first 1-2 weeks after infection and it is impossible not to notice them. Chronic gonorrhea is considered to be a sluggish inflammatory process that lasts over 2 months. In addition, with provoking factors (hypothermia, lack of hygiene), a relapse (exacerbation) occurs with all the characteristic symptoms that are impossible not to feel - purulent discharge from the penis, itching, pain, burning sensation when urinating.
Author:
Nikita Aleksandrovich Korobov, anesthesiologist
Diagnosis of gonorrhea in women
Diagnosis begins with a history and physical examination of the patient. Then laboratory tests are ordered. The causative agent of infection is detected using bacterioscopic and bacteriological methods. Gonococcus is identified by the following basic criteria: it is gram-negative, diplococcus, and is located inside the cells.
This organism is capable of mutating under the influence of external factors, so bacterioscopy does not always identify it. The sensitivity of the method is 45–80%, and the specificity is 38%. To promptly identify asymptomatic forms, it is better to use the bacterioscopy method. This method is also recommended for examining children and pregnant women. Sowing is carried out in a special nutrient medium. Since the material is contaminated with foreign forms of flora, identifying the causative agent of gonorrhea can be difficult. To make it easier to detect, a selective medium with antibiotics is used. If the analysis cannot be carried out immediately, the material is left in a special transport medium. When the cultures grow, microscopy is performed to determine the sensitivity of the organisms to antibiotics. The bacteriological method has high sensitivity and specificity (90-100% and 98%, respectively). Biological material is collected for research using a bacteriological loop or a Volkmann spoon from the urethra, vagina, cervical canal, rectum or other place where an infectious process may develop. To collect material from the rectum, scraping or rinsing is performed using an isotonic sodium chloride solution.
Other laboratory methods include:
DNA research, enzyme immunoassay, immunofluorescence. But they are rarely used.
The order of diagnostic procedures
1. Bacterioscopic examination
colored material, which was taken from three points - U, V, C. In the case of chronic gonorrhea, gonococcus is usually found extracellularly. In acute infection, the pathogen is located inside the cells.
2. Bacteriological analysis
, in which the sensitivity of the pathogen to antibiotics is assessed. Indications for such a study are repeated negative bacterioscopic results, detection of questionable organisms in smears, suspicion of gonorrhea.
3. RIF (immunofluorescence reaction).
4. ELISA (immunofluorescence analysis).
5. PCR and LCR methods.
6. Provocative tests.
If smears and cultures do not reveal the pathogen, they resort to provocative tests using thermal, chemical immunological techniques. During such studies, care must be taken and all possible complications must be taken into account.
- Chemical.
It involves treating the urethra with a solution of silver nitrate to a depth of up to 2 cm, the cervical canal - up to 1.5 cm, the rectum - up to 4 cm with Lugol's solution in glycerin.
- Biological.
Gonovaccine (500 million microbial bodies) is administered intramuscularly. It is also possible to administer gonovaccine and pyrogenal together (dosage – 200 MTD).
— Thermal
. Diathermy is performed for three days in a row. The first day is half an hour, the second day is 40 minutes, and the last day is 50 minutes. Another option is a three-day course of inductothermy once a day for 15 minutes. After each physiotherapy session, the discharge is taken for analysis.
— Physiological.
A smear is taken during menstruation.
— Combined test.
Thermal, chemical and biological tests are carried out within one day. Material for analysis is taken every other day, two and three days. Crops are performed after three days.
Inflammatory processes of other localizations in gonorrhea
Let's briefly consider other foci of inflammation that can appear with gonorrhea in men, but are less common or have minimal clinical significance.
Morgagniitis is an inflammation of Morgagni lacunae.
They are depressions inside the urethra, reaching a length of 1 cm.
Additional symptoms of gonorrhea in men do not appear with inflammation of the lacunae.
Signs of inflammation are detected during urethroscopy.
Periurethritis is an inflammation of the tissue located near the urethra.
Cavernitis is inflammation of the corpora cavernosa of the penis.
It manifests itself as painful erections and can lead to deformation of the penis.
Occasionally, a penile abscess forms.
It can open both into the urethra and into the external environment.
In the latter case, a fistula tract is formed.
Tyzonitis is a lesion of the tyzonium glands.
They are located on the head of the penis.
In case of inflammation, the doctor may palpate dense nodules.
When squeezed, pus comes out of them.
The pathology may be complicated by an abscess.
Treatment of gonorrhea in women
There are several main ways to treat gonorrhea. It is important to follow this rule: the sexual partner of the sick person is also subject to treatment. Non-acute forms of gonorrhea are treated on an outpatient basis, but the presence of an acute course requires hospitalization. In the hospital, bed rest should be observed, injection antibacterial drugs, cold applied to the lower abdomen, infusion therapy (reopolyglucin, reogluman, reamberin, isotonic solutions of glucose or sodium chloride, glucose-procaine mixture, Trisol) and antihistamines (suprastin, tavegil) are prescribed.
Treatment of gonorrhea in women with antibiotics
Antibiotics are used to combat the pathogen. But positive results are not always achieved. There are strains that are resistant to antibiotics. The appearance of L-forms of gonococci is also possible. When prescribing treatment, you need to take into account the form of the disease, the prevalence of inflammation, its localization, and the presence of concomitant infectious processes. In addition, the possibility of complications and side effects must be taken into account.
Drugs for the treatment of gonorrhea in women
Penicillin antibiotics
- benzyl penicillin - from 4 to 8 million units (course 10-15 days);
- ampicillin - tablets 2-3 g per day at equal intervals for 4-6 doses (course from 7 to 20 days);
- oxacillin - tablets 3 g per day at equal intervals for 4-6 doses, course from 10-14 days;
- ampiox - tablets of 0.5-1 g every 4-6 times a day (course 5-7 days);
- carbenicillin disodium salt 4-8 g per day for 4-6 doses intramuscularly;
- unasin (sulacillin) 1.5-12 g per day for 3-4 doses intramuscularly or intravenously;
- amoxicillin with clavulanic acid (Augmentin) 1.2 g 3 times a day intravenously for 3 days, and then 625 mg 3 times a day orally for 5 days.
Tetracyclines
- tetracycline tablets 250 mg 4 times a day, course 14-21 days;
- doxycycline (Unidox, Vibramycin) 1 capsule (0.1 g) 2 times a day, course 10 days.
Macrolides and azalides
- azithromycin (sumamed) 0.5 g, two tablets once, then for 4 days, 1 tablet (0.5 g) once a day.
— midecamycin (macropen) 400 mg 3 times a day, course 6 days;
— spiramycin (rovamycin) 3 million units 3 times a day, course 10 days;
— josamycin (vilprafen) 500 mg 2 times a day, course 10-14 days;
- Rondomycin 0.2 g once, then 0.1 g once a day, course 14 days;
- clarithromycin (clacid, fromilid) - 300-500 mg tablets 2 times a day, course 10-14 days;
- roxithromycin (rulid, roxide, roxibid) 300 mg 2 times a day, course 10-14 days;
- erythromycin - 500 mg 4 times a day before meals orally, course 10-14 days;
- erythromycin ethyl succinate 800 mg 2 times a day, course one week;
- clindamycin (Dalacin C) 300 mg 4 times a day after meals, course 7-10 days or intramuscularly 300 mg 3 times a day, course 7 days.
Aminoglycosides
- kanamycin 1 g 2 times a day intramuscularly, the course will require 6 g. Oto is also nephrotoxic and cannot be prescribed with antibiotics with similar complications.
Cephalosporins
- cefazolin 0.5 g 4 times a day intramuscularly or intravenously, course 5-7 days;
- ceftriaxone 1.0-2.0 g 2 times a day, diluted in 2 ml of lidocaine, injected intramuscularly, course 3 days;
- cefatoxime (claforan) 1.0 g 2 times a day, course 5 days;
— cefaclor capsules 0.25 g 3 times a day, course 7 days;
- cephalexin 0.5 g 4 times a day, course 7-14 days.
Fluoroquinolones
— ofloxacin (Zanocin, Tarivid, Ofloxin) 200 mg 2 times a day after meals, course 7 days;
— ciprofloxacin (Tsifran, Tsiprinol, Tsiprobay, Tsipro-Bid) 500 mg 2 times a day, course 7 days;
— pefloxacin (abactal) 600 mg once a day after meals, course 7 days;
- levofloxacin 400 mg 2 times a day, course 7-10 days;
- lomefloxacin (Maxaquin) 400 mg once a day, course 7-10 days;
- gatifloxacin (Tebris) 400 mg once a day for 7-10 days.
Treatment regimens for gonorrhea in women
| Features of the course of the disease | Drugs and treatment regimen | Note |
| Fresh gonorrhea of the lower genitourinary system without complications | • ceftriaxone 250 mg intramuscularly once; • azithromycin 2 g orally once; • ciprofloxacin 500 mg orally once; • cefixime 400 mg orally once; • spectinomycin 2 g intramuscularly once. Alternative treatment regimens for gonorrhea: • ofloxacin 400 mg orally once; • cefodisime 500 mg intramuscularly once; • kanamycin 2.0 g intramuscularly once; • trimethoprim + sulfamethoxazole (80 mg + 400 mg) 10 tablets orally once a day for three days. | Contraindications for the use of fluoroquinolones are age under 14 years, pregnancy, and lactation. If an alternative regimen is used, then constant monitoring for changes in the sensitivity of the gonococcus is necessary. |
| Gonorrhea of the lower genitourinary system with complications or gonorrhea of the upper and pelvic organs | • tceftriaxone 1 g intramuscularly or intravenously every 24 hours for one week; • spectinomycin 2.0 g intramuscularly every 12 hours for 7 days. Alternative treatment regimens for complicated gonorrhea: • cefotaxime 1 g intravenously every 8 hours; • kanamycin 1 million units intramuscularly every 12 hours; • ciprofloxacin 500 mg intravenously every 12 hours. The course lasts 48 hours, when the symptoms of acute gonorrhea disappear, you can switch to oral administration of drugs: • ciprofloxacin 500 mg every 12 hours; • ofloxacin 400 mg every 12 hours. | During treatment, you should abstain from sexual intercourse and do not drink alcohol. If there is no effect of therapy, you need to use another antibiotic taking into account sensitivity. |
| Combination of chlamydial infection and gonorrhea | • azithromycin 1.0 g orally once; • doxycycline 100 mg 2 times a day orally, course 7 days; • josamycin 200 mg orally, course 7–10 days. | In addition to antibiotics for gonorrhea, drugs for the treatment of chlamydia are added. |
| Combination of trichomoniasis and gonorrhea | • metronidazole 250 mg orally 2 times a day, course 10 days; • secnidazole 2 g orally once; • ornidazole 500 mg morning and evening with an interval of 12 hours, course 10 days. | If there is a suspicion of trichomoniasis in women, then antibiotics that kill Trichomonas are added to the usual treatment regimen. |
Vaginal eubiotics are prescribed together with or after a course of antibiotics to restore normal vaginal microflora. These are drugs that contain lactobacilli, bifidumbacteria bifidum or lactobacilli acidophilus.
Local treatment of gonorrhea in women
Local therapy for gonorrhea in women consists of restoring damaged mucous membranes of the vagina and urethra; for this purpose, a 1–2% solution of silver proteinate, a 0.5% solution of silver nitrate, as well as microenemas with chamomile infusion are used (for 1 tablespoon of chamomile flowers, 1 glass of boiled water).
Immunotherapy for gonorrhea in women
Immunomodulatory drugs for gonorrhea are used quite rarely, since their prescription must be realistically justified. Immunotherapy for gonorrhea should be carried out after the disappearance of symptoms during antibiotic treatment or before antibiotic therapy, when the disease is subacute, torpid or chronic. Immunotherapy is allowed for children only after 3 years of age.
Immunotherapy can be:
- specific (use of gonococcal vaccine)
- nonspecific (pyrogenal, prodigiosan, autohemotherapy).
Physiotherapeutic treatment of gonorrhea in women
Sick women undergo physiotherapeutic sessions (inductothermy, magnetic therapy, laser therapy, ultraviolet light, electrophoresis and phonophoresis of medications).
Surgery for gonorrhea
For salpingitis and pelvioperitonitis, patients are treated with conservative methods. If therapy does not produce the desired effect within a day or two, a laparoscopic procedure is necessary. It makes it possible to carry out an accurate diagnosis, as well as to open and sanitize the focus of purulent inflammation. Patients with diffuse or diffuse peritonitis undergo laparatomy. The scope of such intervention is determined based on age, the degree of pathological changes in the pelvis, and reproductive history is also taken into account.
Possible complications
Over several weeks, inflammation can spread along the walls of the urethra to the bladder, prostate and seminiferous tubules. This causes complications of gonorrhea in the form of cystitis and prostatitis. Symptoms include frequent painful urination, nagging pain in the perineum during sexual arousal and ejaculation, and discomfort in the testicles. Prostatitis can lead to impotence and a decrease in the fertilizing ability of sperm.
Gonorrheal epididymitis appears when the epididymis is involved in a specific inflammatory process. It is usually acute and proceeds violently. This causes fever, redness and swelling of the scrotum, and sharp pain on the affected side. Epididymitis can be unilateral or affect both testicles to varying degrees. The development of epididymitis threatens subsequent cicatricial narrowing of the lumen of the vas deferens with the development of infertility.
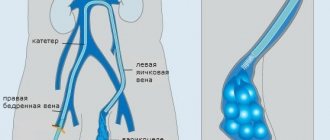
Long-term urethritis, leading to deep lesions of the wall of the urethra, can be complicated by urethral stricture. Difficulty in the outflow of urine contributes to congestion in the bladder, reflux of urine into the ureters and ascending infection of the excretory system.
Massive penetration of the pathogen into the bloodstream leads to the generalization of gonorrhea. In this case, sepsis develops, foci of inflammation appear in other organs, and the heart valves are often affected.
Factors contributing to the development of complicated gonorrhea in men:
- the presence of concomitant acute or chronic diseases of the genitourinary system (cystitis, urolithiasis, prostatitis, prostate adenoma);
- infection with other STDs;
- weakened local immunity, repeated infection with gonorrhea (reinfection);
- eating spicy food;
- frequent sexual arousal;
- use of coitus interruptus as a method of contraception;
- excessive physical activity;
- alcoholism.
Often, a man suffering from gonorrhea consults a doctor not with the initial symptoms of anterior gonorrheal urethritis, but after the development of complications. In this case, even after intensive complex therapy, the consequences of gonorrhea often develop in the form of narrowing of the urethra, infertility and chronic prostatitis.
Treatment of gonorrhea in pregnant women
Treatment of gonorrhea during pregnancy can be carried out at any stage. Drugs allowed during pregnancy include:
• ceftriaxone 250 mg intramuscularly once; • spectinomycin 2 g intramuscularly once.
Pregnant women should not use tetracyclines, fluoroquinolones, or aminoglycosides to treat gonorrhea, as they negatively affect fetal development.
If a complication of gonorrheal choriamnionitis develops, the pregnant woman should be hospitalized and treated according to the following regimen: ampicillin 0.5 g 4 times a day for 7 days or benzylpenicillin 20 million units per day until symptoms disappear. Local therapy, physiotherapy and immunotherapy should be added to antibacterial therapy, especially for chronic gonorrhea.
To prevent the development of gonorrhea in newborns, infants are instilled with 1-2 drops of sulfacetamide solution (30%) into the conjunctival sac.
Treatment methods
Antibiotics are the basis of therapy for gonorrhea. After a course of antibacterial therapy, it is possible to completely get rid of pathogenic bacteria and prevent the development of complications. For this purpose, cephalosporins (for example, Ceftriaxone intravenously, intramuscularly or Cefepime orally) are prescribed once. This is enough to get rid of gonococcus. When treating an extragenital infection, the course of antibiotics can be extended to 3 days.
In case of intolerance to cephalosporins or development of resistance to them, aminoglycosides (Spectinomycin) are prescribed once.
The course of treatment is prescribed to both sexual partners
Important aspects:
- The sexual partner must be treated, otherwise re-infection is inevitable.
- 14 days after completing the course of antibiotics, a repeat test is taken to identify gonococci - monitoring the effectiveness of therapy.
If the result is negative, the patient is removed from the register. If gonococci are detected again, a repeat course of other antibacterial drugs is indicated.
Rehabilitation after treatment of gonorrhea in women
At this stage, it is necessary to evaluate the effectiveness of the therapy (7-10 days after its completion). The treatment criteria are:
- absence of symptoms,
- disappearance of gonococcus in smears during bacterioscopic examination. For diagnostic purposes, it is possible to perform provocative tests, including combined ones. The second control is carried out during the next menstruation. Material for bacterioscopy is taken from the urethra, cervical canal, and rectum (three times at intervals of a day).
The third control involves a combined provocative test after menstruation with bacterioscopic and bacteriological analysis. If the pathogen is not detected, the patient can be removed from the register.
In addition, screening for HIV, syphilis, and hepatitis viruses is recommended. (If the source of infection has not been identified).
Today, many doctors question the need for multiple provocative tests. They suggest shortening the duration of observation after adequate therapy. According to these experts, modern methods are highly effective, and ongoing control measures have become impractical.
The European guidelines note the need for at least one follow-up examination to assess the correctness of treatment. And control laboratory tests are indicated only in case of protracted course of the disease, the likelihood of re-infection, or suspicion of resistance of the pathogenic organism.
How to recover
Treatment for gonorrhea has changed greatly today. This is mainly due to the development of resistance of gonococci to penicillin antibiotics, which in the past formed the basis of therapy. Antibiotics that have a bactericidal and bacteriostatic effect on gonococci are of primary importance. Enzyme and immunotherapy (injections of specific and nonspecific drugs), local remedies (rectal suppositories, microenemas, douching) are also necessary. During pregnancy, the dosage of antibiotics depends on the duration of pregnancy, the nature of the procedures also changes (for example, drugs are not injected directly into the cervical canal).
Self-treatment of gonorrhea at home is unacceptable. This can lead to its transition to a chronic form and the occurrence of irreversible processes. Some girls believe that it is enough to find an article on this topic on the Internet or on a medical forum - and you don’t have to bother with a visit to the doctor, get tested, or “don’t waste your money.” But such people can pay with their health for such views. In the meager texts of published, even very correct standards for the treatment of gonorrhea, many of the nuances on which its result depends are often missed.
Treatment for gonorrhea should be strictly under the supervision of a doctor. Proof of successful therapy is the disappearance of signs of the disease and the absence of gonococci in tests performed 1-2 weeks after the end of taking antibiotics. In women, in addition, 2 additional studies of the same are carried out: during the next menstruation and immediately after it.
Immunity to this disease is not developed. If it is not treated correctly, gonorrhea takes a chronic, protracted course and is aggravated under the influence of alcohol, spicy food, sexual arousal, intimate intercourse, etc.
International standards in treatment
Currently, according to the recommendations of the World Health Organization (WHO) and the US Center for Disease Control (CDC), the antibiotics of choice in the treatment regimen for gonorrhea are: ceftriaxone, cefixime, ciprofloxacin, ofloxacin, levofloxacin, spectinomycin and azithromycin. The uncomplicated form can be cured fairly quickly with the help of these antibiotics.
Since it is combined with chlamydia in approximately 30% of cases, the CDC recommends that after taking a single dose of an antigonorrhea drug, a course against it should be taken. If a microbe is detected in one of the partners, the other one must also be treated, even if he has not been diagnosed with gonorrhea. Treatment of chronic and complicated forms is carried out with higher doses of the same antibiotics. Patients should always remember that only a qualified specialist can take into account all the features and determine the most effective drug, its dose and duration of treatment (taking into account these tests).
Do you suspect you have gonorrhea? Tests, anonymous examination and treatment as soon as possible in our clinic - make an appointment with a gynecologist right now!
Prevention of gonorrhea in women
To reduce the incidence rate, it is very important to detect cases of infection in a timely manner and provide such patients with adequate therapy. Of particular importance are regular medical examinations of employees of child care institutions and catering workers.
Testing for gonococcal infection is mandatory for all pregnant women, as well as for women who go to the gynecological department for termination of pregnancy.
In addition, there are personal prevention methods that every person must follow to prevent infection. First of all, you need to carefully adhere to the rules of personal hygiene and try to avoid casual sexual contacts. When having sexual intercourse, it is recommended to use reliable means of protection. These include condoms or vaginal use of chemicals (chlorhexidine, miramistin). If suspicious symptoms appear (pathological discharge, discomfort), you should immediately consult a doctor.
Publication date 12/10/2016
Symptoms
The main difference between female and male gonorrhea is that in almost half of the patients, the signs of the disease are mild or go completely unnoticed. The diagnosis is determined when you consult a doctor with complaints characteristic of other inflammatory pathologies of the genitourinary system.
Patients' complaints are mainly related to painful urination, green or yellow discharge, discomfort during intimacy, pain in the lower abdomen, and menstrual irregularities.
Incubation period
The first signs of infection in women appear 3-5 days after the bacteria enter the body, but the duration of the incubation period is influenced by a number of factors.
For example, if, simultaneously with gonococci, infection with another pathogenic microflora also occurs, the first symptoms may appear only after two weeks, and sometimes after a month. During the incubation period, the pathogen penetrates from the mucous layer to the submucosal layer and then into the lymphatic system.
The incubation period increases if the woman was currently taking antibacterial drugs. In this case, the activity of the gonorrhea pathogen can be suppressed, and the disease will be asymptomatic.
Clinical manifestations
The symptoms of gonorrhea vary depending on the location of the inflammation and the form of the disease.
If the disease manifested itself immediately after the end of the incubation period, then the most common symptoms of gonococcal lesions include:
- copious purulent or purulent mucous discharge from the vagina;
- discomfort, itching in the area of the external genitalia and vagina;
- painful urination;
- hyperemia and swelling in the labia area.
These symptoms are typical when an infection enters the vagina.
When the oral cavity becomes infected, gonococcal tonsillitis develops, the symptoms of which are fever, sore throat and purulent plaque on the tonsils.
If gonococci have penetrated the rectum, then patients complain of acute pain during bowel movements and purulent discharge from the anus.
When the disease becomes chronic, its symptoms persist, but become less noticeable, appearing only during an exacerbation. The process can be activated:
- sexual contact;
- menstruation;
- consumption of hot spices and alcoholic beverages;
- hypothermia.
During the period of remission, the symptoms of the pathology are practically invisible, the woman considers herself healthy. Since there are no external manifestations of the disease, she can easily agree to unprotected sex, infecting an unsuspecting partner.
Risk group
The risk group for developing the disease includes:
- Sexually active people, whose average age in most cases is 20-35 years.
- Also, who does not use a condom during casual sexual intercourse, as well as when in contact with an unreliable sexual partner.
- Commercial sex workers.
- People who have several sexual partners at once, or those who have a large number of them over a certain period of life.
- Women and men with a history of inflammatory disease from a sexually transmitted infection, in particular gonorrhea.
Incubation period
In the case of gonorrhea, it has certain characteristics. This is primarily due to the gender of the sick person.
In women, gonorrhea occurs differently from the male body, and this is due to the fact that the incubation period can be significantly prolonged and in some cases is more than a month, while in men it is about a week.
In addition, the part of the body where infection and penetration of the pathogen occurs is of particular importance. This is especially true for the genitals, for which this period is valid.
The longest period from the moment of infection to the onset of symptoms is associated with the fact that the pathogen enters the mucous membrane of the anus.
Almost the same period is observed upon contact with the mucous membranes of the oral cavity.
In such cases, the time until the development of the clinic reaches several months. The following factors can increase the incubation period:
- Treatment with various medications, especially antibacterial ones. In this case, great importance is given to the incorrect timing of antibiotics that are sensitive to this pathogen.
- In the event that gonorrhea is transmitted through household contact.
At the same time, the incubation period may be reduced:
- When a woman’s immunity is reduced due to serious diseases, such as tuberculosis, endocrine pathologies.
- Against the background of a combination of gonorrhea with venereological pathology, such as chlamydia, mycoplasma, bacterial vaginosis.
- Combination with bad habits such as smoking, drinking alcohol and drugs.
How to prepare correctly: testing for gonorrhoea
When a gynecologist prescribes a test for gonorrhea to a woman, it is important to follow some rules to ensure that the results obtained are not unreliable.
Preparatory steps before taking the test for gonococci:
- Stop taking antibiotics and get tested no earlier than 3-4 weeks after the course;
- A couple of days before collecting biomaterial, avoid sexual contact;
- Do not douche with antiseptic solutions;
- Wash off with water, without hygiene products;
- Avoid urination 1.5 - 2 hours before taking a smear.
Proper preparation is recommended to obtain the correct test.