What causes orchitis?
Inflammation occurs under the influence of viruses: gonococci, trichomonas, chlamydia, mycoplasmas, ureaplasmas, mumps.
Risk factors
Mature men and boys at an early age are most susceptible to the disease.
The causes of orchitis and factors that provoke its development include:
- infection due to the entry of viruses from the urinary tract and urethra into the testicle;
- inflammation of the testicle as a complication after pneumonia, bronchitis, tonsillitis, sinusitis;
- sexually transmitted and infectious diseases;
- irregular or very frequent sexual intercourse;
- testicular injury;
- alcoholism;
- sedentary work;
- hypothermia;
- regular physical and mental fatigue;
- diseases: pyelonephritis, measles, diabetes, influenza, prostate adenoma.
Causes
Doctors identify many causes of orchitis. The most common of them are:
- Infections that are specific and nonspecific. They can enter the testicle not only from organs located in the immediate vicinity, but also from distant ones. Often the disease occurs due to sexually transmitted infections entering the body. Specific infections include: syphilis, gonorrhea, typhus, tuberculosis, etc. Among nonspecific infections, one can distinguish: bacteria (staphylococcus, E. coli, etc.), viruses (influenza, measles, mumps, herpes, etc.) , fungi (candida, etc.) and urogenital infection (Trichomonas, chlamydia, etc.).
- Injury or other mechanical impact on the organ (impact, consequences of surgery, medical procedures).
- Stagnant processes in the pelvic area associated with poor circulation, prolonged sexual abstinence, the practice of coitus interruptus, etc.
More information about how thrush manifests itself in men?
Immunologist Ermakov Georgy Aleksandrovich will tell you about the causes of development, signs and consequences of the disease:
Risk factors for the development of pathology are:
- Sedentary lifestyle and frequent sitting.
- Too active or, conversely, irregular sex life.
- Decreased body defenses or chronic fatigue syndrome.
- Hypothermia or significant overheating of the genital area.
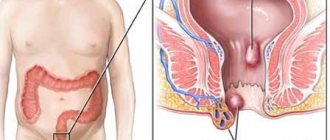
Normal and inflamed prostate with prostatitis
- Impaired urine outflow (with adenoma, prostatitis, etc.).
- The presence of chronic foci of infection in a man’s body (chronic bronchitis, sinusitis, etc.).
- The presence of concomitant pathologies of the genitourinary system (cystitis, pyelonephritis, etc.).
Symptoms and clinical picture of orchitis
Each type of orchitis has its own manifestations. The acute form is characterized by high temperature, an increase in the size of the testicle and the occurrence of sharp pain in it, redness of the scrotum. Symptoms of chronic orchitis (lasting more than 1 month) include hardening and enlargement of the testicle, intermittent aching pain when touching it, a slight increase in temperature, and intoxication. General signs of orchitis (as an inflammatory process): weakness, headache, nausea, dizziness, chills and pain in the testicles.
Consequences and complications
Even with timely treatment of orchitis, the prognosis is not always favorable, especially after mumps. Its virus has an extremely negative effect on the tissue of the seminiferous tubules. Possible consequences:
- Impaired spermatogenesis: a decrease in the number of sperm, their complete absence, a large percentage of immobile and ugly ones;
- In 15-20% of men, infertility develops after bilateral mumps orchitis;
- In 50-75%, the testicles atrophy, and not immediately: in 30% of patients this occurs within the first 2 months, in 40% the process takes from 3 months to a year, in 35% atrophy occurs after 2-4 years.
The result of treatment depends on how quickly and acutely the orchitis developed, what pathogen caused it and how deeply the tissues were affected.
Diagnosis of orchitis
Diagnosis of orchitis is based on examining the patient and conducting a comprehensive examination.
Diagnostic methods
Instrumental studies include biopsy, ultrasound, MRI, and diagnostic puncture.
The tests prescribed for orchitis will help complement the clinical picture and choose the right treatment tactics:
- blood (for the concentration of lymphocytes, leukocytes, ESR level);
- urine (for viruses);
- sperm (for detection and identification of pathogenic microflora);
- smear from the urethra (to identify the causative agent of the disease).
Reviews about the treatment
Uncomplicated mild acute orchitis can be successfully treated with antibiotics and compresses. Reviews below.
A detailed review of the treatment of orchitis complicated by epididymitis from the forum https://hron-prostatit.ru/forum/viewtopic.php?t=15361:
Many men are prescribed compresses with Vishnevsky ointment as part of the treatment for orchitis, but not all specialists approve of this. Below are doctors' answers to the question of how to apply it correctly.
The main condition for successful treatment is a correct diagnosis. Otherwise there will be complications.
Treatment regimen for orchitis
The doctor decides how to treat orchitis after reviewing the examination results.
The main goals of treating orchitis are to eliminate the infection and eliminate the symptoms of the disease. Their implementation is facilitated by drug therapy using:
- antimicrobials (Erythromycin);
- painkillers (Analgin, Ketoprofen);
- cephalosporins (Cefepime);
- anti-inflammatory drugs (Ibuprofen);
- antibiotics (if the disease is protracted and there is purulent inflammation of the testicle);
- probiotics (to normalize microflora).
Treatment with physiotherapeutic methods involves sessions of paraffin and laser therapy, UV irradiation. For chronic orchitis, UHF therapy, magnetic therapy, acupuncture, mineral and mud baths, electrotherapy and physical therapy exercises are prescribed.
Surgical treatment is used in the presence of tumors in the testicle and the appearance of pus in it. Types of operations performed: partial or complete removal of the testicle, puncture of the scrotum. In case of an abscess, the testicle is opened and the abscess is drained.
How to treat orchitis in men
Drug treatment of mild acute orchitis includes oral and intravenous administration of antibacterial and anti-inflammatory drugs. Antibiotic therapy is supplemented with immunomodulatory drugs (Panavir, Immunomax, Interferon), as well as probiotics and hepatoprotectors. The effect of non-steroidal anti-inflammatory drugs is enhanced by absorbable and enzymatic agents.
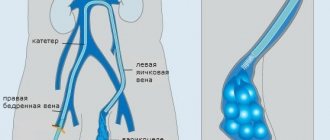
With orchitis, it is necessary to improve blood flow in the scrotum in order to reduce the pressure of biological fluids on the tissue, for which it is raised using a special bandage - a suspensor. Cold compresses are applied to relieve inflammation and swelling. For severe pain, a novocaine blockade of the spermatic cord is performed. After the inflammation has been relieved, treatment is supplemented with physiotherapy: electrophoresis, mud applications.
The scrotal bandage-suspensor helps to reduce the tension of the spermatic cord and improve the outflow of blood from the scrotal organs, provides rest for the operated organs, and can also be used to fix therapeutic bandages
As a result of treatment, acute symptoms disappear by the end of the first week. In some patients, after orchitis, a dense, painless fibrous formation remains on the testicle, fused with the skin of the scrotum.
Surgical intervention is used in cases where, despite drug therapy, an abscess still forms. Then it is opened, washed and drained under local anesthesia.
Urologist, dermatovenerologist Lenkin Sergey Gennadievich on methods of treating orchitis
For moderate to severe orchitis, most doctors are inclined to require active surgical intervention. Removing inflammatory foci and relieving pressure from tissues using puncture helps preserve the functionality of the testicle. In 88% of such patients, long-term results are favorable.
For granulomatous orchitis, drug treatment is useless. The only option is orchiectomy - removal of the testicle. An implant can be inserted instead.
At home
Without preliminary diagnosis at home, testicular inflammation is absolutely impossible to treat. The doctor prescribes the regimen. All folk remedies for topical use should be previously agreed with him. Warming compresses, popular among the people, can provoke an increase in the inflammatory process and an abscess.
Options for lotions for orchitis:
- Grind the dry beans in a coffee grinder, mix the resulting flour with natural apple cider vinegar to a mushy consistency.
- Fresh chopped horsetail.
Horsetail
- A mixture of equal parts honey, aloe pulp, red wine.
- Propolis and cocoa butter.
The mixture is applied for 10 minutes, 2 times a day.
In case of acute orchitis, it is necessary to exclude spicy foods and alcohol, and maintain bed rest. You can take a tincture of dead bees or propolis internally (sold in pharmacies).
Prevention
To avoid such a dangerous pathology as orchitis, men should avoid hypothermia, physical fatigue, casual sex without a condom, scrotal injuries, and bad habits.
It is necessary to promptly identify and treat diseases of the reproductive and excretory systems, sanitize existing foci of infection in the body, have regular sex life, exercise, eat right, do not abuse alcohol, protect the genitals during sports, use a condom, maintain genital hygiene, and get vaccinated against mumps.
Surgical intervention
If conservative treatment of orchitis does not bring the required results, then the question of surgical intervention is raised.
Indications for its implementation are:
- tuberculous nature of the disease;
- frequent exacerbations in chronic orchitis;
- tissue suppuration;
- acute form, developed as a result of injury;
- severe course of the disease, etc.
Depending on the complexity of the case, surgical intervention can be performed using several methods. With the least consequences for functioning, resection is performed - removal of the inflamed part of the testicle. If the operation is insufficiently thorough and in the case of a number of other factors, complications and relapses are possible.
In case of severe purulent lesions - orchiectomy - removal of the testicle and epididymis. If the operation affects both organs, this leads to a significant decrease in the level of male sex hormones and infertility. The attending physician may also suggest other surgical techniques.
What will happen if left untreated?
Untreated or poorly treated acute orchitis becomes chronic.
Possible complications of orchitis:
- Reactive hydrocele is an accumulation of fluid between the membranes of the testicle. This process usually resolves after the underlying disease is eliminated.
- Suppuration of testicular tissue. It is possible to develop one purulent localized focus (testicular abscess) or many small purulent foci (microabscesses) in the testicular tissue. As the process progresses, complete diffuse suppuration of the testicle is possible.
- Inflammation of the appendages (epididymitis). In most cases, the inflammatory process also extends to the epididymis.
- Spread of the inflammatory process to the other testicle.
- Reduction in size, drying of the testicle (testicular atrophy), a frequent complication of acute orchitis.
- Development of infertility. About 50% of cases of acute bilateral orchitis can lead to the development of male infertility.
Course of the disease
The inflammatory processes that occur with orchitis increase rapidly, causing damage to the structure of the testicles.
As mentioned above, orchitis can occur in two forms.
The acute form occurs suddenly and is very painful.
Intense pain is associated with a large number of nerve endings located on the stretching tunica albuginea of the testicle . As a result, the sick person may lose the ability to move independently . There is often a need for hospitalization.
In the chronic form , despite a significant impairment of the secretory function of the testicle, symptoms are not expressed, sexual function is not impaired .
Rehabilitation after illness
If we talk about rehabilitation as such, then only patients who have undergone surgery on the scrotum need it. Typically, two types of operations are performed on this area of the body. This is the evacuation of a purulent source of inflammation and removal of the testicle. As for the second point, such patients, especially if they are young people, need quite serious psychological support, which can only be fully provided by a qualified psychologist.
In addition, the absence of a testicle in itself is a negative emotional factor, which is why today silicone prostheses of this organ are very often used. They come in different sizes, and if a man suffers amputation as a child, then the prostheses require regular replacement. It must be remembered that such an artificial organ serves only an aesthetic function, while the reproductive function can be preserved by the use of a second testicle.