Peritonsillar abscess is an inflammatory disease in which the pathological process is localized in the peritonsillar tissue. Most often, the disease is diagnosed in children, as well as in adolescents and young adults.
Peritonsillar abscess is a complication of inflammation in the oropharynx
Causes of paratonsillar abscess
Peritonsillar abscesses are usually caused by Streptococcus pyogenes,
the same bacteria that cause strep throat and tonsillitis. If the infection spreads beyond the tonsil, it can create an abscess around the tonsil. Peritonsillar abscesses are usually observed in young people in winter and spring, when pharyngitis and tonsillitis are most common. Rarely, people may develop peritonsillar abscesses without tonsillitis. Tonsillitis is most common in children, and peritonsillar abscesses are most common in young adults. In rare cases, these abscesses may occur after tonsil removal.
Pathophysiology
Purulent tonsillitis, as a rule, begins with the onset of acute follicular tonsillitis, progresses to paratonsillitis and leads to the formation of a paratonsillar abscess.
An alternative theory involves the Weber's glands, which are a group of salivary glands located directly above the tonsillar region in the soft palate. These glands are thought to play a minor role in clearing the tonsil area of any “garbage” that has accumulated there. Tissue necrosis and pus formation lead to the formation of an abscess between the tonsil capsule, the lateral wall of the pharynx and the peritonsillar space. As a result of scarring and obstruction of the excretory ducts, pus accumulates in the tissues and the formation of a purulent abscess progresses.
Symptoms of paratonsillar abscess
Symptoms of a peritonsillar abscess can be similar to those of tonsillitis and pharyngitis, but they are often more severe. A person may sometimes see an abscess in the back of the throat, and it may look like a blister or swelling.
Symptoms:
- painful swallowing called odynophagia;
- inability to swallow saliva;
- fever and chills;
- pain causing trismus, difficulty or inability to open the mouth;
- muffled voice;
- headache;
- swelling of the neck and face;
Clinical picture
There is pain in the throat, which increases with swallowing, turning the head and coughing.
The patient experiences difficulty opening his mouth, which is accompanied by severe pain. Trismus (inability to fully open the mouth) of the masticatory muscles is noted. The patient is forced to refuse to eat and drink, the pain interferes with his normal sleep. Body temperature is elevated, patients complain of weakness and malaise. When performing pharyngoscopy, hyperemia (pronounced redness) of the mucous membrane and infiltration of one half of the soft palate and palatine arches on the affected side are determined.
The palatine tonsil is slightly shifted to the healthy side and is tense. The lymph nodes located under the jaw and on the neck become somewhat swollen. Due to the fact that the soft palate is almost motionless, the voice becomes nasal. The most common are peri-almond abscesses with anterior and upper anterior localization.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Peritonsillar abscess - treatment
You should not treat a peritonsillar abscess at home. Consult your doctor to discuss appropriate treatment options. Treatment will depend on how severe the abscess is and how well the person responds to antibiotics. Your doctor may try to treat a peritonsillar abscess with antibiotics first. If they have no effect, the doctor may remove the pus from the abscess.
Medical treatments to treat peritonsillar abscess include:
- removing pus with a needle and syringe;
- puncture the abscess with a scalpel to release and empty the pus;
- surgically removing the tonsils in a procedure called tonsillectomy, which a doctor may recommend if a person has recurring peritonsillar abscesses;
Pathogenesis
The causative agents of the disease are streptococci, staphylococci, pneumococci, Echshieria and Klebsiella, a fungus of the genus Candida. In chronic tonsillitis, the recesses of the tonsils (crypts) are filled with purulent discharge. They are deepest in the upper part of the tonsils - in the place of the most pronounced inflammation.
After several cases of acute inflammation, the tonsil tissue is replaced by scar tissue. Due to scars, the outflow of pus from deep crypts is disrupted; they are not completely cleansed. The infection, concentrated in the tonsils, penetrates deep into the tonsils, into the paratonsillar space around the tonsils.
The frequent localization of an abscess in the upper part of the tonsils is facilitated by the looseness of its fiber. With reduced local immunity, the infection easily penetrates into the deep layers of tissue.
Peritonsillar abscess - complications
Once a person receives treatment, the peritonsillar abscess usually goes away without causing further problems. However, if left untreated, an abscess can cause serious problems.
Complications of a peritonsillar abscess include:
- obstruction (blocking) of the airways;
- dehydration;
- infection of the jaw, neck, or chest;
- a bacterial infection in the bloodstream known as sepsis;
- pneumonia;
- meningitis;
- endocarditis, an infection of the inner lining of the heart.
When to lower the temperature
This disease, against the background of tonsillitis, first manifests itself with a sharp increase in temperature above 38°C. After it, other symptoms begin to appear. Like any purulent inflammation, it puts a huge burden on the body. Therefore, it is imperative to reduce the temperature with antipyretic drugs. For these purposes, otolaryngologists recommend using:
- Ibuprofen, for example, in the form of Nurofen or children's Nurofen;
- Paracetamol.
Unlike other diseases of the ENT organs, peritonsillar abscess requires a decrease in temperature even when it rises to 38°C.
Peritonsillar abscess - diagnosis
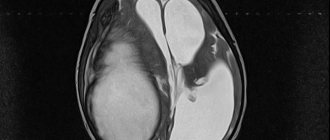
The doctor will examine your mouth and throat to diagnose a peritonsillar abscess. A doctor can usually detect this condition through a visual examination. Swelling and redness in one tonsil may indicate an abscess. The doctor may move the swollen area to determine if there is pus inside. If pus is present, the doctor may collect a sample to send to a laboratory for further testing. In some cases, the doctor may request X-rays or an ultrasound of the neck to rule out other conditions such as peritonsillar cellulitis, epiglottitis, or other upper respiratory tract infections.
Conservative treatment methods
Drug treatment of paratonsillitis should begin in the early stages of development. Key principles of conservative treatment:
- A large volume of liquid (fruit drinks are especially useful), liquid food and bed rest. If the patient has severe pain, medications and nutritional mixtures are administered through a tube. Sometimes intravenous drips of sodium chloride and glucose solutions are prescribed.
- Taking antibacterial agents orally and intramuscularly. For this purpose, penicillin antibiotics (Ampicillin, Flemoxin, Amoxicillin, Unasin, Flemoclav, Panclave, Oxacillin), macrolides (Azotrimycin, Azitral, Josamycin, Sumamed, Hemomycin), aminoglycosides (Amikacin), fluoroquinolones (Levofloxacin, Norfloxacin, Sparfloxacin) and cephalosporins (Cefixime, Cefuroxime, Ceftriaxone, Cefepime, Cefazolin).
- For the purpose of detoxification, Hemodez, Neocompensan, Reamberin, Reosorbilact are administered intravenously.
- To sanitize the oral cavity, solutions of Chlorophyllipt and Furacilin are used. In addition, you can use Chlorhexidine, Givalex, Miramistin, Eludril and Lugol's solution.
- If the disease is complicated by a fungal infection, Intraconazole is prescribed.
- Paracetamol, Analgin, Phenacetin, Diclofenac, Nurofen, Indomethacin, Voltaren, Meloxicam are prescribed as analgesics and anti-inflammatory drugs.
- To prevent allergization of the body, antihistamines are used (Lomilan, Claritin, Kestin, Zyrtec, Loratidine, Telfast).
- After antibiotic therapy, pre- and probiotics (Linex, Acipol, Enterol, Lactobacterin, Probifor, Biosporin, Hilak, Lysozyme) are prescribed to restore the saprophytic intestinal microflora.
We invite you to familiarize yourself. Today I discovered something black under the gum.
In acute disease and severe pain, drugs are prescribed parenterally - intravenously, intramuscularly or rectally. Oral medications cannot be used, because they can only aggravate the patient’s condition by injuring the area of the abscess.
conclusions
Peritonsillar abscess
c is a painful, pus-filled pocket of tissue that forms at the back of the throat, near the tonsil. This is usually a complication of pharyngitis or tonsillitis. The best treatment for a peritonsillar abscess depends on how severe the abscess is and how well it responds to antibiotics. Some procedures include draining the abscess or performing a tonsillectomy.
The authors of another study claim that tonsillectomy increases the risk of developing respiratory diseases.
Classification
Forms of abscess depending on the stage of development:
- Edema stage - the tissues around the tonsils swell, there is no inflammation, as well as clinical symptoms of the disease.
- Infiltration stage - the affected tonsil is hyperemic, pain and fever are noted.
- Abscess stage - 4-7 days after the formation of the infiltrate, a large fluctuating protrusion forms.
Classification by location:
- Anterior or anterior superior abscess - diagnosed in 75% of cases, formed above the tonsil;
- Posterior abscess - diagnosed in 10-15% of cases in the posterior arch or between the edge of the tonsil and the edge of the arch.
- Lower abscess - diagnosed in 5% of cases between the lower edge of the tonsil and the lateral wall of the pharynx.
symptoms
- Lateral or external abscess - diagnosed in 5% of cases between the wall of the pharynx and the lateral edge of the tonsil, it is very difficult.
Symptoms and signs
There are quite a few symptoms indicating the development of an abscess. Signs of the pathological process appear literally from the first hours from the beginning of its development. It can be:
The child exhibits general weakness, lethargy, and may experience insomnia. In adults, it can also occur with less severe symptoms. The patient's condition improves slightly when spontaneous autopsy occurs. The pain decreases and the feeling of fullness disappears.
Upon examination, the doctor notes an enlargement of the tonsils, severe tissue hyperemia and swelling of the paratonsillar region. If the abscess is extensive, the mobility of the palatine arches and uvula may be impaired.
Physiotherapy
When abscessing paratonsillitis, you cannot use physiotherapy procedures that have a warming effect, as this will increase the production of pus. Physiotherapeutic treatment should be aimed at relieving inflammation. The following methods have this effect:
- magnetic therapy;
- exposure to ultra-high frequency currents;
- microwave treatment.
However, all methods of physiotherapy tend to dilate blood vessels at least a little. This may worsen the situation during the acute period. Therefore, they can only be used for rehabilitation after opening a purulent focus of infection.
Treatment at home
Of course, purulent tonsillitis cannot be cured with home remedies alone. They are used only if the pathology develops at the initial stage, and folk remedies act as additional methods of therapy.
Fir cones
Finely chop a handful of raw materials, add 2 cups of boiling water. Place on the stove to let the water boil. Then cover with a lid and wait 30 minutes. After time, add a couple of drops of pine ether to the infusion. If this is not available, then it is allowed to use any coniferous oil.
Place back on the stove to simmer. Now you can carry out inhalation, which lasts 15 minutes. Perform similar activities 2-3 times a day. The resulting solution can be used to rinse the throat. Do this 5-6 times a day. Treatment is continued until the entire clinical picture is overcome.
Honey onion
Grind the onion and combine with 40 ml of honey. Heat in the microwave. Take the mixture 5 g every 2 hours. You don’t need to swallow it right away, keep it in your mouth until the mixture dissolves on its own. But how to use onion cough syrup and how effective it is is described in detail in this article.
Mumiyo
Shilajit helps a lot in the fight against pus. It can be bought at the pharmacy in tablet form. The tablets must be dissolved every day, 2 times a day. Thanks to this drug, it is possible to quickly cope with the infection.
This information will help you understand why tonsils appear in holes after a sore throat and how you can cope with this problem.
It will also be interesting to learn about how to treat loose tonsils in a child.
But how stomatitis on the tonsils in a child is treated and what remedies should be used is described in this article.
Propolis tincture
This remedy has unique properties, because by gargling with propolis tincture you can relieve inflammation, fungal and bacterial infections, and also increase the body's defenses. There are several methods of application, including:
- Combine 200 ml of warm water and 20 ml of propolis tincture. The resulting solution should be used to gargle. Carry out such events several times a day.
- In addition, you can simply drink 20 drops of the tincture. Take it 2 times a day.
- Combine the tincture and vegetable oil in equal quantities. Soak a cotton swab in the solution and treat the area where the abscess is observed. Similar actions should be performed as often as possible until recovery occurs.
But how to treat a sore throat with propolis and how effective this procedure is is described in great detail in this article.
Prevention
With a peritonsillar abscess, the outcome for the patient is most unpredictable, and in most clinical pictures serious complications are observed. It is important to prevent the disease, and for this it is necessary to promptly treat sore throat and prevent the development of chronic tonsillitis. If such an ENT disease has been noticeably prolonged, it is possible that ulcers appear on the tonsils and are prone to rapid growth. They already have to be removed along with the tonsils; this is a complicated course of the disease, which can lead to serious consequences.
If a patient is at risk, his main task is to strengthen the immune system, prevent infection by harmful microorganisms, and promptly treat inflammatory processes in the larynx. Especially for these purposes, the following preventive measures are provided that can be implemented at home against peritonsillar abscess:
- timely treatment of dental diseases;
- correction of immunodeficiency conditions and diabetes mellitus;
- final abandonment of bad habits;
- adequate treatment of diseases of the nose and oral cavity;
- exclusion of alcoholic beverages from the daily diet;
- strengthening of immunodeficiency states;
- preventing prolonged hypothermia of the body.
Development mechanism and reasons
The origin of the abscess process is based on two groups of factors.
- Infectious lesion of the pharyngeal area. Typically, the disorder develops gradually. It all starts with acute inflammation. Exactly what origin depends on the case. But most often it is of bacterial origin.
The causative agents are staphylococci and streptococci, both representatives of pyogenic or pyogenic flora.
Over time, the formation of the abscess itself, an abscess, is possible. Usually against the background of weakening local and general immunity.
- Stagnant process. This mechanism is approximately the same, but goes through more stages in its development. Even before the development of an infectious disorder, a violation of local immunity is observed.
The body is not able to resist negative influences. Then, as soon as a venous-lymphatic disorder develops, the likelihood of tonsillitis and acute tonsillitis increases.
If the condition continues long enough, chronic pathology cannot be avoided. And this is a direct path to the development of complications.
Peritonsillitis develops in 7 stages. The process goes like this:
- A local circulatory disorder appears.
- Because of this, the intensity of local immunity decreases. The body is unable to resist the influence of bacteria, viruses and fungi.
- An inflammatory process develops. Mostly infectious.
- Hence the swelling, an even greater weakening of the body's defenses.
- If treatment is insufficient or absent altogether, tonsillitis becomes chronic. Becomes a person's constant companion.
- Latent forms of the inflammatory process with frequent relapses increase the likelihood of complications.
- At some point, a peritonsillar abscess may develop. This is not necessary, but it is quite possible. How likely such a scenario is depends on the individual characteristics of the organism.
As a rule, purulent lesions of the pharynx develop in the first few years from diagnosis. If the correction is sufficient, this is the only episode at all.
When treatment is ineffective or started late, there is a high probability of a repetition of events and the next formation of a peritonsillar abscess.
A peri-almond abscess develops as an outcome of an inflammatory condition, tonsillitis. But the list of reasons does not end there.
Factors in the development of the disease can be divided into two groups.
Actually, dangerous infectious agents enter the body and affect the pharynx. Which ones exactly depends on the nature of the inflammation.
As a rule, we are talking about the following infections:
- Influenza and parainfluenza viruses. Classic pathogens of ARVI.
- Herpetic structures. Strains of the first and second types. Less often - others. Children may be affected by the third form of herpes (Varicella-Zoster virus), which usually provokes chickenpox.
- Staphylococci. The basis of the pathological condition. They most often cause an inflammatory disorder, a peritonsillar abscess.
In terms of prevalence and breadth of influence, only the following representatives of the pyogenic flora can compete with them.
- Streptococci. They cause dangerous and complex forms of abscesses. Without sufficient treatment, the disorder very quickly becomes chronic with regular exacerbations in the future.
- Fungal flora. An uncommon variant of the pathogen. They belong to opportunistic microorganisms. That is, as long as the body actively holds back the onslaught, the immune system works, everything is fine. But as soon as the protective forces fail, the pathological process becomes relevant.
Caution:
Interestingly, fungi cause some of the most dangerous and aggressive forms of peritonsillar abscess.
- There are also other pathogens. Including pneumococci, Haemophilus influenzae, chlamydia, mycoplasma. But they are not that common.
The second group of factors are those that increase the likelihood of developing a peritonsillar abscess.
Among them:
- Hypothermia. Both general and local. For example, when drinking cold drinks during the hot season.
- Smoking. Because hot tobacco smoke irritates the mucous membranes of the pharynx and oral cavity.
- The same goes for drinking alcohol. Ethanol burns delicate tissues and has a negative effect.
- The presence of a focus of chronic infection in the body. The classic option is carious teeth, gingivitis and other gum problems.
Risk factors increase the likelihood of a problem. But it’s impossible to say exactly how much. The causes of tonsil abscess are always infectious, also associated with a decrease in the patient’s local and general immunity.