Rosa Ismailovna Yagudina, Doctor of Pharm. Sc., prof., head. Department of Organization of Drug Supply and Pharmacoeconomics and Head. laboratory of pharmacoeconomic research of the First Moscow State Medical University named after. I. M. Sechenov. Evgenia Evgenievna Arinina , Ph.D., leading researcher at the laboratory of pharmacoeconomic studies of the First Moscow State Medical University named after. I. M. Sechenov.
With the coming summer, the topic of our article has acquired particular relevance. Intestinal infections are a whole group of infectious diseases that mainly affect the gastrointestinal tract. Acute intestinal infections are second only to acute respiratory diseases in their prevalence. The peak incidence usually occurs in the summer, but intestinal infections caused mainly by viruses are also common in the cold season. However, the most common cause of these diseases is the entry of infectious agents into the gastrointestinal tract with contaminated food and water.
In total, about 30 infectious intestinal diseases are currently known. The most common ones include:
- food toxic infection (mainly of staphylococcal etiology)
- salmonellosis
- dysentery
- enterovirus and rotavirus infection
- cholera
According to the degree of danger, they can be divided into non-hazardous, dangerous and especially dangerous. Thus, food poisoning infections (PTIs) are considered non-hazardous, and cholera, typhoid fever, etc. are considered especially dangerous. But this does not mean that the so-called “non-dangerous” PTI does not cause serious damage to the body and does not lead to complications.
Complications of intestinal infections:
- bacterial infections of the respiratory system and middle ear
- intestinal dysbiosis
- intestinal bleeding
- perforation of the intestinal wall
- intussusception
- bacterial toxic shock
Classification of infections depending on the pathogen
Gastrointestinal infection is one of the most common infectious pathologies in the world. There are more than 30 types of this significant group of diseases that affect more than a billion people every year. According to medical statistics, they rank third among all infectious diseases. Depending on the type of pathogen that caused the disease, there are the following types of intestinal infections:
- Bacterial - they are caused by pathogenic bacteria: E. coli, Shigella, Salmonella. They are transmitted through water, food, dirty hands and objects.
- Viral – the culprits of the disease are rotaviruses, adenoviruses, enteroviruses. Infection occurs by airborne droplets, through food, dirty hands and objects.
- Fungal – when immunity decreases, Candida fungi often multiply in the intestines.
- Protozoans – provoke protozoan pathogens. Spread by insects, sometimes sexually transmitted.
Who's at risk
The immune system of a healthy person is able to independently fight viruses immediately after they enter the body, preventing the disease from reaching an acute stage. If the immune system is compromised, it is unlikely that it will be possible to avoid infection when exposed to rotavirus.
The most vulnerable categories among the adult population are:
- pregnant women;
- people who have had colds or other infectious diseases;
- patients after surgery;
- patients taking antibiotics (especially potent ones);
- socially disadvantaged residents;
- people who find themselves in difficult life situations and forced to give up quality food.
These categories of people automatically fall into the risk group for possible infection with intestinal flu, since their immunity is not able to independently cope with the causative agent of the disease due to their lifestyle, health status or other reasons.
Where do pathogens of infectious diseases come from?
The source of intestinal infections is a person or animal whose body contains pathogenic bacteria. They are released from the infected body with feces, vomit, exhaled air when sneezing and coughing. Outside the human and animal body, pathogenic organisms rarely reproduce. Most often, when exposed to unfavorable environmental conditions, they die. However, anthrax pathogens persist in the soil for many years. The danger of sources of intestinal infections depends on:
- duration and massiveness of discharge;
- professions of the infected person (teacher, educator, cook, food seller).
In addition, the danger of patients to others depends on:
- features of the course of the disease - severe, mild, asymptomatic, carrier;
- period of illness - latent, the height of illness or recovery.
Patients with a severe course during the height of the disease are very dangerous, but they can be isolated as they are easily identified. Patients with a mild and asymptomatic course of the disease, as well as carriers, are difficult to identify, so they are considered more dangerous.
Infected animals are more dangerous for humans the more they come into contact with them. This could be large and small cattle with anthrax and brucellosis, cats with toxoplasmosis, dogs with rabies. They become infected from wild animals during hunting when cutting up carcasses and processing skins. Epidemiological surveys help prevent infection.
Routes of transmission of infectious diseases
The following transmission routes are typical for gastrointestinal infections (GIDs):
- Nutritional – eating poor quality food, poorly washed vegetables and fruits.
- Water – using water for drinking and cooking from questionable sources.
- Contact and household - through household items, poor hand washing, lack of personal hygiene.
- Airborne - pathological microorganisms that the patient excretes with sputum when talking, sneezing and coughing enter the body of a healthy person with the air.
It should be noted that aerosol transmission of LCDs is rare. Most often, people become infected due to poor personal hygiene.
Routes of infection
Cells affected by the virus die within 18-22 hours after the pathogen enters the human body. After this period, they descend into the lower parts of the gastrointestinal tract, after which they move into the intestines, causing stool disorder in the form of persistent diarrhea. Infected cells come out along with the stool.
Rotavirus has excellent “survivability”: it can withstand extremes and strong temperature fluctuations, and is able to remain outside the human body for 6 hours, maintaining the ability to reproduce.
You can become infected with rotavirus infection in any public place and even at home if someone in your household is a carrier of the disease. Most often this occurs when coming into contact with personal belongings or being in a closed room with a sick person for a long period of time.
The main ways of contracting intestinal flu in adults:
- through water (for example, when swimming, visiting a pool or drinking raw water);
- when consuming low-quality food;
- through personal hygiene items belonging to a sick person (toothbrush, towel, etc.);
- during personal contact (kisses, hugs, handshakes, etc.);
- with poor hygiene (dirty hands).
The incubation period for intestinal flu is 5 days. During this time, the person is a carrier of the disease, although he himself does not even know about it.
Clinical picture
Regardless of the cause of the disease and the type of intestinal infection, patients experience general symptoms that manifest themselves:
- Pain syndrome – painful sensations occur in the upper or lower abdomen.
- Diarrhea – many intestinal infections are characterized by frequent bowel movements with false urges.
- Constipation – occurs in severe cases and persists for several days.
- Changes in stool - its structure becomes liquid, watery, and a change in color occurs. Blood, mucus and undigested food debris appear in the stool.
- Nausea and vomiting - these signs depend on the severity of the disease. Vomiting appears once or several times, after which the patient feels better or, conversely, the condition worsens.
- General intoxication of the body - the condition worsens: fever occurs, headaches appear, appetite decreases and severe weakness occurs.
If symptoms of intestinal infections are detected, treatment must be carried out under the supervision of a doctor to avoid serious complications.
Consequences
With untimely or inadequate medical care, an infectious intestinal disease can cause:
- Dehydration is the loss of large amounts of fluid due to diarrhea and vomiting. Water-salt metabolism is disrupted, blood pressure decreases, and heart rate increases.
- Dehydration shock is rapid dehydration with the threat of death.
- Toxic shock is the rapid onset of intoxication with a drop in blood pressure.
- Acute renal failure.
- An inflammatory process in the lungs – pneumonia.
Diagnostics
If an intestinal infection is suspected, the patient should consult a physician. It is impossible to make a specific diagnosis after a conversation and examination of the patient. Therefore, the following tests are required to determine the type of intestinal infection:
- Coprogram - physical, chemical and microscopic characteristics of feces are revealed.
- Bacteriological - the causative agent of the disease is determined by inoculating the biomaterial on a nutrient medium and its sensitivity to antibiotics.
- Serological – the patient’s blood is checked for antibodies. The analysis is taken on the fifth day of the disease and allows you to accurately identify the type of microorganism.
After receiving the results of the studies, an accurate diagnosis is established and appropriate therapy is prescribed.
Treatment options
As soon as the first symptoms of the disease appear, you should eat as little food as possible and drink plenty of fluids to prevent dehydration. It is better to drink regular non-carbonated mineral water, compotes, and unsweetened tea. The liquid should not be cold or very hot.
Rehydration products
Helps with frequent vomiting and diarrhea. It is worth giving preference to pharmaceutical drugs.
Enterofuril has proven itself well, capable of fighting any intestinal infections.
Antibiotics
Prescribed to treat many bacterial infections. They can only be used for medical purposes. This or that drug is able to fight a specific type of bacteria. It is important to correctly identify the causative agent of infection. Proper use of antibiotics will allow you to experience a noticeable improvement within a day after starting treatment. They should be taken throughout the entire treatment course, the duration of which is determined by the doctor.
If treatment is interrupted, the remaining microorganisms will become resistant to antibiotics and become insensitive to their action. As a result, over time the disease will manifest itself with even greater force and it will be more difficult to overcome it. Effective agents include: Levomycetin, Ampicillin, Rifaximin.
Antiprotozoal agents
Effective against protozoal infectious lesions. Like antibiotics, they can only be prescribed by a doctor; you should never self-medicate, otherwise there is a risk of worsening the condition. First you need to do an examination. The results of the analysis will allow you to establish an accurate diagnosis and select appropriate medications. Usually prescribed: Ornidazole, Clarithromycin, Spiramycin.
Viral infections
What are the types of viral intestinal infections? Let's look at the specific symptoms of the main ones:
- Rotavirus - increased body temperature, possible runny nose, sore throat, nausea and vomiting, followed by relief, diarrhea - foamy watery stools of a yellowish tint, loss of appetite, deterioration in general condition.
- Adenoviral - high temperature, severe intoxication, frequent heavy stools, vomiting, enlarged lymph nodes, inflammation of the oral mucosa, possible conjunctivitis.
- Enteroviral - the temperature can rise to 40 degrees, pain in muscles and joints appears, convulsions are possible, the nasopharynx becomes inflamed, pain in the heart area, diarrhea and vomiting are possible.
Viral intestinal infections are transmitted through dirty hands, poorly washed vegetables and fruits, poor-quality water, as well as through airborne droplets when a sick person talks, sneezes and coughs. Illnesses most often begin with an acute course. They are often difficult to diagnose because the symptoms vary greatly depending on the virus.
Therapy
Treatment for symptoms of intestinal infection is as follows:
- Fighting dehydration – diseases are accompanied by vomiting and diarrhea, so there is a large loss of fluid. To restore it, as well as normalize the salt balance, you need to drink a lot and take Regidron.
- Removing intoxication - sorbents are used for this purpose: “Polyphepan”, “White Coal”, “Smecta”. These drugs help remove harmful substances from the body.
- Restoration of enzyme metabolism - “Festal”, “Mezim”, “Creon” will help to resurrect the damaged intestinal mucosa.
In addition to medications, which must be taken under the supervision of a doctor, you must follow a diet.
Treatment of rotavirus infection in adults
For a favorable outcome of the disease, the patient is prescribed symptomatic treatment, that is, aimed at combating the clinical signs of rotavirus and eliminating its consequences. The standard treatment regimen includes:
- oral rehydration;
- enterosorbents;
- diet.
In severe cases and when signs of dehydration appear, the patient is given IV drips, which help replenish fluid in the body and restore the balance of mineral salts in the blood.
Oral rehydration therapy
Since rotavirus infection is accompanied by profuse diarrhea and vomiting, in order to avoid complications such as dehydration and in order to replenish the volume of lost fluid, the patient should immediately begin taking oral rehydration solutions. They can be purchased at the pharmacy and prepared according to the instructions. The optimal content of electrolytes and microelements in the following products:
- Regidron;
- Humana electrolyte;
- Trihydron;
- Hydrovit.
You can also prepare a saline solution for oral use yourself: to do this, you need to take a liter of boiled cooled water, 6 teaspoons of sugar, half a teaspoon of salt and a pinch of baking soda. Mix everything thoroughly and drink a small sip every 5 minutes.
Important! To avoid a repeated attack of vomiting, it is not recommended to drink a lot of liquid at once - it is best to take a saline solution in small sips at regular intervals.
Oral rehydration for an adult with rotavirus infection is continued until there is a stable improvement in the condition - cessation of vomiting and diarrhea.
If the patient vomits even after a small sip of the solution and it is impossible to replenish the volume of lost fluid through the mouth, then they must be connected to a system through which solutions of sodium chloride, glucose and vitamins will be infused directly into a vein, drop by drop.
Enterosorbents for rotavirus infection
To reduce the amount of toxic substances in the body and remove them from the intestines as quickly as possible during rotavirus infection, the patient is prescribed enterosorbents:
These drugs bind toxic substances in the intestines, prevent their further absorption into the blood and remove them from the body with feces.
Bacterial intestinal infections
These diseases often arise due to poor personal hygiene, improper heat treatment of foods, and consumption of food that has expired or is stored in improper conditions. Various bacteria cause the disease:
- coli;
- staphylococci;
- salmonella;
- shigella
Signs of intestinal infections caused by viruses and bacteria are similar. But it should be noted that bacterial intestinal infection is more severe. The incubation period has a wide range and ranges from several hours to several days. Children suffering from a viral infection often experience a sharp deterioration in their condition after feeling better. This indicates a bacterial complication. It is characterized by a rise in high temperature, nausea, vomiting, white coating on the tongue and tonsils, as well as severe intoxication. The most common names for intestinal infections caused by bacteria are:
- dysentery;
- salmonellosis;
- botulism;
- typhoid fever.
An accurate diagnosis can only be made in the infectious diseases department of the hospital after examining stool and blood. In severe cases, the patient is prescribed antibiotics. Otherwise, therapy is carried out in the same way as for a viral infection. The doctor prescribes saline solutions, sorbents, and enzymes to restore the intestinal mucosa. If severe dehydration occurs, saline solution is administered intravenously using a drip. Antipyretics are used to reduce fever. All treatment is carried out strictly under the supervision of a doctor.
Treatment
Treatment of an intestinal infection depends on what pathogen is causing it, however, a number of general rules can be identified that apply to all lesions of the digestive system.
Diet
In mild cases of pathology, the patient is prescribed a gentle diet. The total volume of food is reduced, foods harmful to the intestines are excluded, and the most gentle nutrition is prescribed. In moderate to severe cases of the disease, the total daily caloric intake is reduced by approximately 40-50%. It is recommended to increase the frequency of meals to 6-8 times a day. During the recovery period, when diarrhea syndrome disappears, it is recommended to prescribe prebiotics to the patient, both in the form of food products and separately, in tablets.
| Recommended Products | Not Recommended Products |
|
|
Drugs
Antibiotics are used to treat severe bacterial infections. The means are selected depending on the pathogen.
The determination of the treatment regimen and dosage of the medication is carried out only by the patient’s attending physician.
For milder forms of the disease, antibacterial drugs are usually not prescribed; symptomatic therapy is carried out. It includes:
- Administration of saline solutions (Trisol, Regidron). In mild forms of the disease, the liquid is prescribed orally, in severe forms it is administered parenterally.
- Antipyretics. To reduce temperature and intoxication, non-steroidal anti-inflammatory drugs (Ibuprofen, Nimesulide), as well as Paracetamol, are prescribed.
- Sorbents (Enterosgel, Polysorb, Smecta). Drugs from this group neutralize toxic substances contained in the affected intestine and remove them from the body. Thanks to this, the severity of intoxication in the body is reduced.
- Probiotics and prebiotics. Intestinal infections are usually accompanied by symptoms of dysbiosis, so patients are prescribed medications to restore the normal microflora of the digestive system. Medicines are used exclusively during the rehabilitation period, when diarrhea syndrome disappears, since before this their use is practically ineffective.
If an intestinal infection is suspected, the patient must assess his condition and decide on treatment tactics. If this is mild food poisoning, which is not accompanied by a pronounced rise in temperature and extraintestinal symptoms, then the disease can be treated at home. For this, hunger and rest, plenty of drinking, and the use of sorbents are recommended. If the patient’s condition is serious, severe fever, or extraintestinal manifestations occur, it is imperative to consult a doctor. The patient may need to be hospitalized in a gastroenterology department or an infectious diseases hospital.
The prognosis for the patient will depend on the causative agent of the intestinal infection. In most cases, the disease is easily eliminated, but in some specific diseases the disease is accompanied by complications and can even lead to death. The key to a favorable resolution of the disease is early consultation with a doctor and compliance with his instructions.
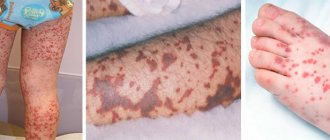
Dysentery
One of the main intestinal infections of bacterial origin is dysentery. Its causative agent is the Shigella bacterium, which actively multiplies in a favorable nutrient medium and dies instantly when boiled. You can become infected from a carrier of the disease or a sick person. Particularly dangerous are people who suffer from mild forms of this disease and work in the catering industry. The latent period of the disease lasts on average 2–3 days. The main symptoms of dysentery (intestinal infection) include:
- general weakness, fatigue;
- loss of appetite;
- headache;
- increased body temperature;
- diarrhea containing mucus and blood;
- nausea and vomiting;
- false urge to defecate.
The onset of the disease is acute. The patient develops chills, loss of appetite, dull pain in the abdomen, and vomiting. The disease can manifest itself in a mild form with the occurrence of minor seizures or cause a severe condition accompanied by neurological disorders. Dehydration often occurs. Diet has a special place in the treatment of dysentery. Food is prepared pureed, completely eliminating plant fiber. Immediately after the onset of the disease, they begin to put the water-salt balance in order. For moderate and severe forms, antibiotics are used. Restore intestinal microflora and support immunity. All prescriptions are made only by a doctor.
Salmonellosis
What are intestinal infections? One of the acute infections caused by bacteria is salmonellosis. The main source of infection are animals that carry salmonella. The main route of transmission occurs through food - animal and poultry meat, fish, milk and eggs. It is possible to get an infection after drinking low-quality water from open reservoirs. Salmonella are very resistant to environmental conditions: they tolerate drying and freezing well, are resistant to smoking, are preserved in pickles, but die when boiled. Getting from the stomach into the mucous membranes of the intestines, bacteria begin to secrete toxins that contribute to the development of the disease. The incubation period for salmonellosis (intestinal infection) averages from 12 hours to a day. The disease often begins acutely, and the following symptoms are noted:
- elevated temperature up to 39 degrees;
- state of chills;
- headache;
- malaise and weakness;
- cramping attacks of abdominal pain;
- nausea and vomiting;
- loose stools with an unpleasant odor, foamy up to 10 times a day, possibly containing mucus, sometimes blood.
For treatment, they use drugs that restore the water-salt balance, neutralize and remove toxins, use antibiotics to destroy salmonella, support the body with vitamin complexes, and restore beneficial bacteria with biological products. All treatment is carried out strictly under the supervision of a doctor. In moderate and severe cases - in hospital departments.
Bacteria that cause inflammation
Diarrhea in these cases can be either watery or bloody. Although watery diarrhea most often occurs with infections caused by viruses, protozoa and bacteria that produce toxins, it can also occur with invasion of the intestinal mucosa by microorganisms. The daily volume of feces is usually more than a liter. General symptoms are not typical.
Bloody diarrhea (for example, with dysentery) is usually accompanied by abdominal pain, tenesmus, nausea, vomiting and general symptoms - fever and malaise.
The infections they cause are difficult to distinguish from each other by clinical presentation, so diagnosis must be based on culture results.
Campylobacteriosis
Epidemiology . Campylobacter jejuni is the most common bacterial cause of bloody diarrhea in the United States. It also causes intestinal infections in developing countries. Campylobacter jejuni is a microaerophilic, gram-negative, curved rod that enters the human body through meat (pork, lamb, beef), milk and dairy products, water, and also through contact with infected domestic animals. Campylobacter jejuni is killed by cooking food, pasteurization, and water purification.
Symptoms and signs
- Enterocolitis. Infections caused by Campylobacter jejuni or (rarely) Campylobacter fetus cause diarrhea, reminiscent of salmonellosis and dysentery. Sometimes there is a prodromal period with headache, myalgia and malaise, lasting 12-24 hours.
- Disseminated infection. It can be caused by Campylobacter fetus (and occasionally by Campylobacter jejuni), more often in elderly weakened patients, as well as in alcoholism, diabetes mellitus and malignant neoplasms. Bacteremia may be transient or may lead to secondary infection (including endocarditis, meningitis, cholecystitis, thrombophlebitis). There may not be any symptoms of enterocolitis.
Complications . Campylobacteriosis can be complicated by Reiter's syndrome, mesadenitis, terminal ileitis (reminiscent of Crohn's disease) and, in rare cases, present with symptoms resembling typhoid fever.
Diagnosis is based on stool and blood culture. Microscopy of a Gram-stained stool smear reveals characteristically curved rods resembling “gull wings.”
Treatment . In mild cases it is symptomatic.
Salmonellosis
Epidemiology . Three main species of Salmonella are pathogenic to humans: Salmonella typhi, Salmonella choleraesuis and Salmonella enteritidis. The latter type often causes an intestinal infection accompanied by diarrhea. The genus Salmcmdla has 1,700 serotypes, grouped into 40 serogroups. About 90% of Salmonella pathogenic to humans belong to serogroups B, C and D. The main reservoir of infection is poultry. Infection requires a large number of microorganisms (more than 105), so the incidence is relatively low, despite the frequent contamination of food products.
Pathogenesis . Salmonella produces an enterotoxin that causes watery diarrhea. In addition, bacteria attach to the mucosa and penetrate the epithelial cells, which leads to inflammation and bloody diarrhea.
Symptoms and signs . Salmonella invades the intestinal mucosa and produces an enterotoxin that causes secretory diarrhea. Diarrhea is often watery, but can also be bloody. The disease usually goes away on its own within a week. Fever and bacteremia occur in less than 10% of patients. However, against the background of immunodeficiencies, malignant neoplasms, hemolytic anemia, liver diseases, with achlorhydria, chronic granulomatous disease in children, salmonellosis can progress: bacteremia develops, secondary foci of infection arise in the joints, bones, meninges and other organs and tissues. In 5% of cases, Salmonella affects the reticuloendothelial system and can cause typhoid fever (Salmonella typhi). Sometimes carriage of salmonella is observed, which are localized in the gallbladder or urinary tract.
Diagnosis is based on medical history and stool and blood cultures. The diagnosis is confirmed by an increase in the titer of agglutinating antibodies to O- and H-antigens at 3-4 weeks of the disease.
Treatment is usually symptomatic. Antimicrobial therapy is contraindicated in most cases, as it can prolong carriage of the pathogen. However, young children, as well as those at high risk of bacteremia and a protracted course of the disease, are still prescribed antimicrobial drugs (ampicillin, chloramphenicol, TMP/SMC, ciprofloxacin, third-generation cephalosporins). Antimicrobial therapy is indicated for bacteremia, typhoid fever and secondary foci of infection. In addition, antimicrobial drugs are prescribed for AIDS, hemolytic anemia, lymphomas, leukemia, as well as newborns, elderly patients and long-term carriage of salmonella. For Salmonella infections, M-anticholinergics and opioids should not be prescribed, as they prolong the period of release of bacteria into the environment.
Dysentery
Epidemiology . The genus Shigella includes 4 main groups: Shigella dysenteriae, Shigella flexneri, Shigella boydii and Shigella sonnei. The most severe form of dysentery is caused by Shigella dysenteriae. In the United States, 60-80% of dysentery cases are caused by Shigella sonnei, with incidence higher in winter. In tropical countries, the causative agent of dysentery is often Shigella flexneri, especially at the end of summer. The transmission mechanism is fecal-oral. Humans are the only source of infection. Dysentery is very contagious; a very small amount of the pathogen is enough for infection - less than 200 bacteria. Microorganisms in food, milk or water can cause outbreaks. With overcrowding and unsanitary conditions, the incidence of disease increases.
Pathogenesis . Shigella produces an enterotoxin that causes watery diarrhea. In addition, they attach to the intestinal mucosa and invade epithelial cells, causing colitis and bloody diarrhea.
Symptoms and signs . As a rule, the disease begins with pain in the lower abdomen and diarrhea. The temperature rises in less than half of patients. Dysentery often occurs in two stages: first, the temperature rises, abdominal pain and watery diarrhea develop, and after 3-5 days a burning sensation in the anus, tenesmus and scanty frequent stools mixed with blood, characteristic of severe colitis, appear. Extraintestinal complications of dysentery include conjunctivitis, epileptic seizures, meningismus, Reiter's syndrome, thrombocytopenia, hemolytic-uremic syndrome.
Dysentery can occur in different ways. In children it usually goes away in 1-3 days, and in most adults in 1-7 days. In severe cases, the disease can last more than 3-4 weeks with periodic relapses. In these cases, dysentery may be mistaken for ulcerative colitis.
Treatment is symptomatic and includes rehydration and antipyretics. Antidiarrheals that weaken peristalsis (diphenoxylate/atropine, loperamide) are not prescribed. Antibacterial therapy reduces the duration of fever, diarrhea, and the release of bacteria in feces. TMP/SMC, tetracycline and ampicillin (but not amoxicillin) are effective, but cases of microorganism resistance to these drugs have been described. Ciprofloxacin and norfloxacin are also effective.
Infections caused by pathogenic strains of Escherichia coli
In addition to enterotoxigenic diarrhea, other strains of Escherichia coli also cause diarrhea. These include enteroinvasive, enteropathogenic, enterohemorrhagic, enteroadhesive and enteroaggregating strains. All of them contain plasmids encoding virulence factors. All pathogenic strains of Escherichia coli specifically interact with the intestinal mucosa, either attaching to the surface of enterocytes or penetrating into them. Some strains produce cytotoxins and enterotoxins.
Enteroinvasive strains of Escherichia coli
Epidemiology . Enteroinvasive strains often cause intestinal infections in travelers. Outbreaks have been described that have occurred when consuming imported cheese. Enteroinvasive strains also cause outbreaks of intestinal infection in children 1-4 years old.
Symptoms and signs . Like Shigella, enteroinvasive strains of Escherichia coli invade and destroy enterocytes, causing watery and then bloody diarrhea.
Diagnostics . Leukocytes are found in the stool. Serotyping and ELISA are carried out for research purposes only.
Treatment is symptomatic. Bismuth subsalicylate reduces diarrhea by suppressing secretion in the intestines and is effective against infections caused by all pathogenic strains of Escherichia coli. Antibiotics used for dysentery and rifaximin are also effective.
Enteropathogenic strains of Escherichia coli
Epidemiology . Enteropathogenic strains of Escherichia coli are one of the main causative agents of diarrhea in both developing and developed countries. They often cause outbreaks of intestinal infections in nurseries in children under one year of age. Sporadic cases of diarrhea have also been described in adults. Due to adhesins, bacteria are tightly attached to the enterocytes, thereby destroying the brush border.
Symptoms and signs . The disease can last more than 2 weeks and subsequently cause relapses.
Diagnosis is carried out by serotyping.
Treatment . Non-absorbable antibiotics are prescribed: neomycin, colistin, polymyxin. Ciprofloxacin, norfloxacin and aztreonam are also effective and are preferred.
Enterohemorrhagic strains of Escherichia coli
Epidemiology . Enterohemorrhagic Escherichia coli strains have been isolated from hamburger mince. They cause outbreaks in nursing homes, day care centers and schools.
Pathogenesis and symptoms . Enterohemorrhagic strains produce two types of verotoxins, similar to the neuroenterotoxin of Shigella dysenteriae, and an adhesion factor encoded by a plasmid gene. The transmission mechanism is fecal-oral. Children are more likely to get sick, but several outbreaks have been reported among adults who ate beef contaminated with bacteria. Bloody diarrhea may be profuse, but white blood cells are not always found in the stool.
Diagnosis is based on isolation of the pathogen from stool and serotyping of Escherichia coli colonies that do not grow on sorbitol.
Treatment is symptomatic. In severe cases, ciprofloxacin or norfloxacin is prescribed.
Prevention
The summer period is favorable for the spread of intestinal infections. At this time, people go out into nature en masse, swim in open reservoirs, eat fresh fruits and vegetables, and cook meat products on the street. Therefore, in order to prevent acute intestinal infections, it is necessary:
- strictly observe hygiene - wash your hands often and thoroughly;
- drink only bottled water and pasteurized milk or boil them;
- wash fruits, berries and vegetables thoroughly with running water;
- observe the thermal regime when cooking meat and fish;
- do not store raw and prepared foods together;
- Use a refrigerator to store perishable foods and observe shelf life;
- Maintain cleanliness in food preparation areas and remove trash promptly.
By following these simple rules, you can avoid contracting intestinal infections and maintain your health. But if you notice symptoms of the disease, you cannot treat yourself, consult a doctor.
Diet and regimen
For patients diagnosed with intestinal flu, it is important to observe bed rest during the acute stage of the disease, as well as other recommendations to speed up recovery. These include:
- regular ventilation of the room in which the patient is located;
- daily wet cleaning using disinfectants;
- limiting contact with other family members;
- using boiling water to wash items worn by an infected person;
- separate storage of personal hygiene items for the patient.
An equally important component of successful treatment is a special diet. Fasting is allowed only on the first day - at this time the patient should be given as much liquid as possible, mostly salty.
Starting from the second day, you should add vegetable purees and porridges prepared without milk to your diet. On the third day, the menu should include the following products:
- fermented milk products (yogurt, kefir, fermented baked milk);
- boiled vegetables;
- boiled chicken (breast) or fish - no more than 50 g per day;
- decoction of rice or oats.
All dishes should be prepared only using dietary methods (boiling, baking, stewing).
What is strictly prohibited for intestinal flu:
- fried foods;
- smoked meats, marinades;
- sauces, spices, herbs;
- confectionery, sugar;
- bread, buns, pastries;
- pork;
- milk;
- fruits.
The therapeutic diet for intestinal flu should last until complete recovery, as well as for two weeks after - this is necessary to normalize the functioning of the digestive organs and reduce the load on the stomach and intestines.
Stomach flu is a common illness that can occur at any age. With proper and timely treatment, the disease does not pose a danger, but it is better to prevent its occurrence. For prevention, it is important to strengthen the immune system, eat a healthy and varied diet, monitor body hygiene and not use other people’s hygiene products.
For more information about the causes, symptoms and treatment of intestinal flu, watch the video:
Rate how helpful this article was
5 Voted by 1 person, average rating 5
Did you like the article? Save it to your wall so you don’t lose it!