Diagnostics
Diagnosis criteria:
- professional route (work experience in harmful and/or dangerous conditions) according to the work book;
- contact with a harmful production factor (HAZF) according to the sanitary and hygienic characteristics of working conditions;
- pathognomonic changes on x-ray/CT.
2.1. Complaints and anamnesis
Analysis of data on sanitary and hygienic characteristics of working conditions - obtaining information about the availability of professional experience.
Duration of professional experience before the appearance of pathological changes:
- in most cases 20 years or more;
- when in contact with low-fiber dust - at least 10 years;
- with rapidly progressing silicosis – less than 10 years.
2.2 Physical examination
In most cases, there are no changes on physical examination.
There are no specific symptoms.
With massive fibrosis, there may be areas of dullness of pulmonary sound above the fields of fibrosis.
With progression, cyanosis, barrel-shaped chest, and weight loss may develop.
Non-respiratory signs - swelling of the joints, their deformation and pain, skin changes can occur when silicosis is combined with systemic diseases - Kaline-Kaplan syndrome.
The coniotic process is often complicated by pulmonary tuberculosis, accompanied by hemoptysis or night sweats.
Wheezing and/or harsh breathing is rare and possible when combined with COPD.
Boxed sound is rare.
Areas of dullness of percussion sound over the lungs are rare, possible with massive fibrosis
Thickening of the fingers in the form of drumsticks only in severe forms with DN, is not specific for pneumoconiosis.
Weight loss is rare.
2.3 Laboratory diagnostics
There is no specific laboratory diagnosis.
Study of blood gas composition for signs of respiratory and/or right ventricular failure.
If a complication of tuberculosis is suspected:
- tuberculin skin tests;
- immunological tests in vitro (PCR, RNGA, RPG, RPK, ELISA, quantiferon test, IGRA);
- bacterioscopy and sputum culture.
2.4 Instrumental diagnostics
General radiography of the chest organs (CH) in two projections .
Indications for CT :
- every 5 years for everyone working with APFD after 10 years of experience;
- assessment of changes in the lungs over time in patients with an established diagnosis;
- primary diagnosis of nodular forms in patients with nodular silicosis;
- all patients of the professional center with a suspected/established diagnosis;
- The severity of dyspnea is not explained by radiographic changes or spirometry results.
Continue the diagnostic search to rule out other interstitial diseases:
- in the absence of typical signs against the background of the pathology identified by radiography of the OGK or high-resolution CT;
- with morphological changes without a typical x-ray picture of pneumoconiosis.
Spirometry:
- identification of disorders of the ventilation capacity of the lungs,
- determining the severity of the disease,
- choice of treatment tactics,
- detection of respiratory failure (RF),
- determining the type of functional disorders (restrictive, obstructive, mixed),
- degree of gas exchange disturbances.
Blood oxygen saturation using pulse oximetry to clarify the degree of DN.
Doppler echocardiography from parasternal access to identify cor pulmonale.
2.5 Other diagnostics
Transbronchial biopsy to exclude granulomatosis (sarcoidosis, berylliosis), lung cancer.
Open lung biopsy if other interstitial lung diseases are suspected.
PET-CT to exclude some granulomatous processes (sarcoidosis, tuberculosis).
Causes of pneumoconiosis
The development of the disease occurs as a result of inhalation of microscopic particles of dust, which spread through the alveoli, penetrating the lung tissue. Dust particles have a toxic effect, which initiates the oxidation of adipose tissue, forming collagen in the structure of the affected lungs.
Industrial dust is especially hazardous to health. There are organic, inorganic and mixed dust. The organic type includes cotton, wool, and protein dust. Pneumoconiosis is most often formed as a result of exposure to dust of inorganic origin, which can be metallic or mineral.
Interesting fact! Hippocrates described the disease by noting that people mining ore would begin to cough violently and then die. In 1866, pathology was identified as a separate group of diseases.
Types of pneumoconiosis
The depth of dust distribution through the respiratory system and the degree of its evacuation from the lungs depends on the size of the aerosol elements - dispersity. The smallest particles, the parameters of which do not exceed 2 microns, penetrate deep into the respiratory tract, settling on the alveolar walls, bronchioles, and respiratory tract. Larger particles are eliminated through the bronchial apparatus.
Due to exposure to the smallest aerosol elements, connective tissue grows in the lungs - diffuse fibrosis and respiratory failure are diagnosed. As a result of such changes in the lungs, the following pathological phenomena develop:
- bronchiolitis;
- emphysema;
- endobronchitis.
Pathologies caused by the influence of aggressive dust particles belong to the group of occupational diseases, the treatment of which is carried out by an occupational pathologist.
Treatment
Key points:
- there are no drugs and methods that cure pulmonary fibrosis and change the dynamics of decreased lung function;
- treatment is aimed at pathogenetic mechanisms and clinical symptoms, prevention of complications;
- To enhance the effect of pharmacotherapy, non-drug methods are recommended.
Treatment objectives:
- Reduce symptoms and increase exercise tolerance.
- Improved overall well-being.
- Prevention and treatment of complications.
- Extending life and active working capacity.
- Minimizing side effects of drug therapy.
Basic treatment strategies:
- To give up smoking.
- Rational employment when indicated.
- Pathogenetic therapy.
- Pulmonary rehabilitation for shortness of breath.
- Oxygen therapy for hypoxia.
Indications for hospitalization:
- Primary diagnosis of pneumoconiosis (differential diagnostics, examination of connections with the profession, prescription of therapy and pulmonary rehabilitation).
- Stable course of pneumoconiosis (monitoring of the condition, correction of therapy and pulmonary rehabilitation, examination of work ability).
- Worsening of the course of pneumoconiosis.
3.1 Non-drug treatment
To give up smoking.
Rational employment of the patient.
3.2 Drug treatment
Total bronchoalveolar lavage in rapidly progressing silicosis.
Acetylcysteine reduces the progression of restrictive syndrome and decreased diffusion capacity of the lungs.
Glutamic acid to increase the resistance of coniophages.
Hyaluronidase + azoximer bromide as an antifibrotic and immunomodulatory agent.
Pulmonary rehabilitation is recommended for all patients with dyspnea on exertion.
Long-term oxygen therapy more than 15 hours per day:
- at PaO2 55 mm. Hg Art. and below or oxygen saturation SpO2 less than 88%;
- at PaO2 55-60 mm. Hg Art. and SpO2=88% for pulmonary hypertension, peripheral edema or polycythemia (hematocrit more than 55%).
Bronchodilation therapy in the presence of COPD: beta-2 agonists, anticholinergics, theophylline and their combination.
Treatment of latent tuberculosis infection with a papule of 10 mm or more, or with a positive immunological test.
3.3 Surgical treatment
Surgical treatment is not recommended as a method of choice.
3.4 Lung transplantation
At the terminal stage of DN with PaO2
Absolute contraindications:
- another incurable disease in a severe stage;
- addictions (including smoking);
- lack of social support;
- uncorrectable mental illness;
- documented non-compliance with drug treatment recommendations.
Relative contraindications:
- over 65 years old;
- pregnancy.
Possible complications
The prognosis for recovery depends on the phase of the disease and the consequences that arise during the course of the pathology. In the case of long-term exposure to harmful factors and the lack of necessary therapy, there is a risk of developing complications that aggravate pneumoconiosis, affecting other structures.
Complications of the pathological process include:
- pneumonia;
- pulmonary heart;
- bronchial asthma;
- tuberculosis;
- heart failure;
- respiratory dysfunction.
Asbestosis, silicosis, and berylliosis are characterized by an unfavorable course. This is explained by the intensive development of pathologies after eliminating contact with aggressive dust. Other forms of the disease are easily treatable.
Lymph nodes affected by tuberculosis
Lymph node tuberculosis is a common complication of silicosis, which affects the intrathoracic lymph nodes. A characteristic sign of silicotuberculosis is the presence of tuberculosis bacteria in the patient’s bronchial mucus. Fistulas may be detected, after treatment of which scars form.
Occasionally, a consequence of pathology is the formation of tumor processes. Neoplasms are characterized by gradual growth, during which the patient’s condition does not worsen, which complicates the early detection of cancer.
Rehabilitation
4.1 Rehabilitation
- medical: inpatient and outpatient treatment, sanitary treatment, dispensaries, rest homes, boarding houses, health groups;
- social: material compensation for damage to health based on disability and percentage of loss of ability to work, benefits, etc.;
- labor: rational employment, free training or retraining for a new profession.
Pneumoconiosis is an absolute contraindication for working with dust; referral to BMSE is required.
4.2 Clinical observation
Annually:
- examination by a therapist;
- examination by a pulmonologist;
- examination by an occupational pathologist;
- OGK radiography and CT;
- FVD study.
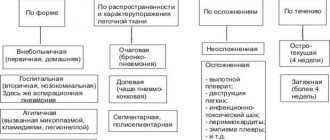
Classification of pneumoconiosis
Factors influencing the progression of pathology include the composition, nature of inhalation and concentration of dust of organic or mineral origin. Based on the contents of inhaled dust, the following groups of occupational lung diseases are distinguished:
- silicosis – inhalation of dust that contains silicon dioxide;
- silicates – inhalation of silicon compounds with metals (talcosis, asbestosis, calinosis);
- carboconioses – dust containing carbon (graphitosis, anthracosis);
- metalloconiosis - the influence of metal dust (siderosis, aluminosis, berylliosis);
- pneumoconiosis resulting from exposure to mixed dust (anthracosilicosis, siderosilicosis).
Silicosis is one of the most serious diseases resulting from exposure to silicon dioxide. This type is diagnosed in people interacting with ore, ceramics, and refractory materials. The severity of silicosis is determined by the duration of exposure to dust.
The factor that causes asbestosis is the inhalation of asbestos dust, the particles of which affect the lungs. This type of pneumoconiosis is detected in workers in the construction, aviation, and shipbuilding industries.
There are pathologies that are caused by regular inhalation of dust from sugar cane, flax, and cotton. This type of pneumoconiosis is similar to bronchial asthma and allergic alveolitis.
Peculiarities
During the diagnosis of pathology, the type of employment of the patient, the level of negative impact and physiological information are determined first of all. Tests such as radiography, spirometry, and blood tests are used as auxiliary tests.
Among occupational diseases, pneumoconiosis is the most common. They are often diagnosed in workers in engineering, coal, asbestos, and glass production, where harmful industrial dust affects the human respiratory system for 5 years or longer.
Prevention measures
In order to prevent pneumoconiosis, it is necessary to improve and modernize working conditions for workers exposed to the negative effects of dust, and reduce the time spent at work. It is necessary to prevent dust from entering the human body using personal protective equipment:
- respirators;
- glasses;
- workwear.
To prevent illness, you need to visit your doctor regularly
Industrial premises should be ventilated by humidifying the air.
To prevent the development of the disease, people at risk are sent to sanatoriums or hospitals. Regular preventive examinations are of paramount importance, allowing pathology to be identified at an early stage.
Pneumoconiosis is an occupational disease caused by exposure to industrial dust. The degree of lung damage depends on the period of work, the type of dust and working conditions. The main requirement for successful therapy is to avoid interaction with a harmful factor.
How to treat?
Treatment of pneumoconiosis includes a mandatory set of measures. First of all, the patient must completely stop staying in the area with gassed/aerosolized harmful impurities in the air. Visiting health camps, dispensaries and sanatoriums is beneficial for relieving symptoms.
Recovery is also facilitated by increasing immune resistance:
eating balanced foods- active spending of the day with sports exercises,
- compliance with the exact schedule of activities carried out during the day: food, sports, walks, rest, sleep.
There are specially designed exercises to restore respiratory function. You can learn about the methods of performing them and the procedure for carrying them out from your attending physician or independently from specialized sources.
Smokers need to temporarily or completely give up the bad habit; all patients are advised to avoid places where the air is filled with smoke, exhaust or other harmful accumulations.
In inpatient treatment, the following are actively used:
- physiotherapy procedures (ultrasound method, heating),
- herbal medicine (inhalation of agents that increase respiratory function, calm and restore proper blood flow),
- ultraviolet irradiation (UVR) courses.
Drug treatment is carried out by using expectorants and cough suppressants; heart complications are suppressed by bronchodilators. For expectoration, herbal remedies are used (pharmaceutical herbs coltsfoot, marshmallow, violet, etc.), compositions based on essential oils (compressive, inhaling), and other medications of a mucolytic/secretolytic or secretomotor nature. The following cough suppressants are used: Doctor Mom, Bromhexine, Herbion.
In case of severe consequences of the disease, the patient is prescribed individual treatment. It consists of anti-inflammatory and antiproliferative (reducing the formation of tissue growths) therapy.
In cases of exacerbation of heart failure, in addition to bronchodilators, the doctor prescribes:
- cardiac glycosides (stimulants of heart muscle contraction),
- anticoagulants (blood thinners),
- diuretics (diuretic drugs).
In this case, the patient is placed under constant observation in hospital, which allows him to constantly monitor his well-being and make therapeutic adjustments if his condition persists or worsens.
Consequences
The pathological process is also accompanied by emphysema, which in some cases develops into an incurable form. Along with transformations of lung tissue, pneumoconiosis is combined with diseases of the mucous membranes, which resemble bronchiolitis or endobronchitis in their manifestations.
As a result of these successive phenomena, large areas of the lung cease to perform their functions in the overall breathing process. In most cases of the disease, using radiography, pathology is detected exclusively at the active stage of pneumoconiosis and its rapid progression.
Mechanism of disease development
An excess of dust in the working environment and poor protection of the breathing apparatus lead to the entry and accumulation of harmful substances in the alveoli. Particles collected in this way can penetrate into the porous tissues of the lungs or be absorbed by macrophages. After this, cytotoxicity often appears, which provokes lipid oxidation.
During this process, lysochondrial and lysosomal enzymes are released, which cause the active proliferation of fibroblastic cells and the formation of collagen in the lung area. In addition, the efficiency of immunopathological mechanisms increases.
The cause of pneumoconiosis is pulmonary fibrosis, which is expressed as nodules that block large areas of organ tissue. This disease manifests itself in the form of sclerotic accumulations consisting of macrophages with a high content of dust and connective tissue particles. If their number is small or completely absent, interstitial pneumoconiosis is diagnosed - this is a disease that is accompanied by thickening of the alveolar septa, as well as perivascular and peribronchial fibrosis. Due to the connection of small nodules, they turn into large clots that fill the lung tissue.
Symptoms
The danger of occupational diseases is that they may not make themselves felt for a long time and may not cause either subjective or objective clinical manifestations. All this occurs against the background of gradually developing fibrosis. 5 years of exposure to high concentrations of dust in the air is enough for pathology to develop even 10-20 years after the end of work.
The nature of the course of pneumoconiosis is usually chronic with gradual development and progression of changes causing increasingly severe disorders and symptoms:
- at the initial stage, a person experiences a lack of air, chest pain and a dry cough (with nephelinosis, viscous sputum is possible), the airiness of the lung tissue increases;
- the subsequent course has manifestations similar to pulmonary failure, then signs of heart failure , a nonproductive cough is annoying, shortness of breath ;
- as a result, emphysema , cirrhosis of the lung and its shrinkage may occur, as well as atrophy or hypertrophy of the mucous membranes of the respiratory tract, metabolic disorders and deterioration of the pancreas and stomach.
The second stage of determining the disease
Then the quality of breathing is determined using several diagnostic methods:
- Spirometry. Allows you to measure the volume of inhaled oxygen, the rate of its entry and exit from the body.
- Plethysmography. Helps determine the characteristics of external respiration.
- Pneumotachography. Allows you to measure arterial rhythm and breathing at rest and after several exercises.
- Gas analytical examination. Allows you to measure the volume of remaining air after a complete exhalation.
At the same time, all kinds of tests are collected to identify foreign impurities in the expectorated secretion. If there are any hiccups or problems with diagnosis using standard methods, the patient may be sent for a biopsy.
Pathogenesis
Occupational diseases associated with work in dusty rooms, workshops and mines are dangerous due to their hidden, almost asymptomatic course against the background of diffuse growth of connective tissue in the lungs, as well as, for example, as in silicosis, the formation of characteristic nodules. Foreign tissue reduces the lungs' ability to process oxygen.
External view of the lung of a healthy 78-year-old man suffering from pneumoconiosis
The pathogenesis is considered not to be thoroughly studied; scientists put forward various theories. The most common is phagocytic: after the penetration of foreign small dust particles into the lungs, they settle in the alveoli, through absorption by macrophages or white blood cells, the body tries to remove them, but macrophages are not able to cope with this task, so they rupture, which leads to the release of particles into the lung tissue. The fibrotic process with scar formation is caused by the accumulation of lactic acid, subsequent activation of the enzyme - ketoglutorate , which directly triggers the process of collagen . As a result, the respiratory surface of the lungs decreases.