SPECIALISTS Gynecologist Gynecologist-endocrinologist Pediatric gynecologist Mammologist-oncologist Dermatologist Hirudotherapist Intimate surgeon Contour plastic doctor Ultrasound doctor SERVICES AND PRICES Gynecology Mammology Ultrasound diagnostics Paid tests Intimate surgery Contour plastic Treatment for women PROMOTIONS AND DISCOUNTS Students Teams Friends and subscribers Residents m district For pensioners Promotions at the clinic
One of the miracles of the human body is that every cell is renewed over time and replaced with new, healthy cells. This gives us the opportunity to work on changing our fertility issues by nourishing and caring for our bodies now so that these new cells have the best chance to be alive and healthy!
On another page of the site, you learned what the clinic offers that is beneficial for the health and functioning of the ovaries, read about proper nutrition, products and vitamins to support the normal function of the appendages. But did you know that it is also important for a woman to have a healthy uterus in order to receive a fertilized egg? Many patients say that they cannot get pregnant because “the egg just won’t stick.” Or “the doctor says my uterus is not healthy enough for implantation”...
That's why we offer you a guide to action to improve your uterine health. Many of these remedies may be familiar to you in one way or another, but after reading this information you will be able to look at them in a completely new way. This is that they have an amazing ability to prevent and heal various parts of our body, as well as provide a preventive and general healing effect.
Structure and dimensions
The uterus is an unpaired female reproductive organ, predominantly consisting of multidirectional smooth muscle fibers, externally covered with modified peritoneum (perimetry), and internally lined with mucous membrane (endometrium).
The adult uterus of a nulliparous woman is pear-shaped and flattened in the anteroposterior direction. Anatomically there are three parts:
- The fundus is the upper portion located above the line of entry of the fallopian tubes into the uterine cavity.
- The body is triangular in shape. The wide part of the body is directed upward, towards the abdominal cavity.
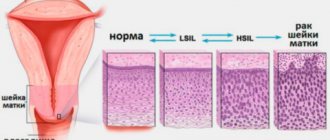
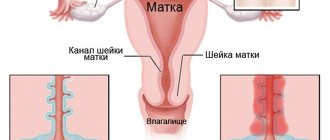
- The cervix is a direct continuation of the body of the uterus. There are two sections in the cervix:
- The vaginal section (exocervix) , lined with stratified squamous non-keratinizing epithelium.
- The supravaginal area (endocervix, cervical canal, cervical canal) , consisting mostly of smooth muscle fibers surrounding the cervix in a circle, with inclusions of collagen and elastin fibers. The endocervix is lined with single-layer columnar epithelium.
This is what a healthy uterus should look like in a non-pregnant woman. When pregnancy occurs, the shape begins to change. In late pregnancy, the uterus looks like a spherical muscular formation with thin walls. In some cases, palpation and ultrasound examination in the early stages of pregnancy reveal its slight asymmetry. This is a variant of the norm and does not entail any consequences.
During pregnancy, the size of the uterus also changes. By the end of the second month of pregnancy, the size doubles, and by the end of the third month it quadruples.
Schematically, a woman’s uterus can be depicted as a triangle, the corners of which are the openings of the fallopian tubes and the cervix.
The shape of the cervix differs between women who have given birth and women who have not given birth. The cervical canal in nulliparous women resembles a spindle (that is, it is narrowed at the ends and widened in the middle), and the uterine os (the border between the cervical canal and the vagina) has a round or oval appearance. In women who have given birth, the cervical canal has a uniform width throughout, and the pharynx is a transverse slit with torn healed edges.
The size of the uterus may vary depending on the period of a woman’s life and the number of pregnancies and births she has had. According to ultrasound data, three sizes of the body and cervix are determined.
| Women category | Dimensions of the uterine body, mm | Cervical dimensions, mm | ||||
| Length | Width | Thickness | Length | Width | Thickness | |
| "Virgin Womb" | 37 – 49 | 26 – 38 | 40 – 50 | 25 – 35 | 23 – 30 | 25 – 35 |
| After one birth | 45 – 58 | 35 – 45 | 46 – 56 | 28 – 39 | 25 – 32 | 28 – 37 |
| After the second and subsequent births | 50 – 65 | 40 – 50 | 50 – 60 | 30 – 44 | 26 – 36 | 30 – 40 |
| Early postmenopause (up to 5 years) | 33 – 45 | 27 – 35 | 31 – 41 | 25 – 34 | 20 – 30 | 23 – 33 |
| Late postmenopause (more than 5 years) | 28 – 38 | 20 – 31 | 27 – 37 | 20 – 30 | 16 – 26 | 20 – 29 |
Diagnostics
The doctor clarifies the patient’s complaints, studies the medical history, asks questions about the menstrual cycle, and conducts an examination in a gynecological chair.
If a bicornuate uterus is suspected, the following diagnostic measures are carried out:
- examination of the uterus with probing through the cervical canal;
- ultrasound sonography of the pelvic organs;
- hysteroscopy – examination using an optical device;
- ultrasound-guided hysterosalpingoscopy;
- diagnostic laparoscopy.
The bicornuate uterus is differentiated from the intrauterine septum. If necessary, magnetic resonance imaging is performed.
Location
The location of the uterus is the small pelvis, where its anterior wall is adjacent to the bladder, and its posterior surface is in contact with the rectum.
The uterus has a certain degree of mobility, and its position depends on the level of fluid in the bladder. If it is empty, then the fundus of the uterus is directed towards the abdomen, and the anterior surface is directed forward and slightly downwards. In this case, the uterus forms an acute angle with the cervix, open anteriorly. This condition is called anteversion. As the bladder fills, the uterus begins to tilt posteriorly, forming an angle with the cervix that is close to the unfolded one. This position of the uterus is called retroversion.
Treatment
Bicornuate uterus can only be eliminated surgically. Indications for radical treatment are infertility and recurrent miscarriage (read more about the treatment of infertility in this material - note altravita-ivf.ru). During the operation, a rudimentary horn or septum is removed, which allows the uterine cavity to be restored.
The intervention is performed by laparotomy or hysteroscopy. During laparotomy, the fundus of the uterus is incised, the septum is removed, and the membranes of the organ are sutured. Postoperative rehabilitation consists of observing contraception for a 6-9 month period so that reproductive function can be fully restored. For this purpose, a special intrauterine contraceptive is used.
Anatomy
The wall of the uterus has a three-layer structure:
- The inner mucous membrane is the endometrium. Lining the inside of the uterus, the endometrium has no folds, is lined with ciliated epithelium and is rich in glands. The epithelium is also well supplied with blood, which explains its sensitivity to injury and inflammatory processes. In photos and videos taken during hysteroscopy, the inside of the uterus is a flat, smooth space of various colors - from pink to grayish, depending on the phase of the female cycle and the woman’s age.
- The middle muscular layer is the myometrium. This layer consists of smooth muscle cells intertwined in all directions. Because the muscle cells are smooth, the woman is unable to regulate uterine contractions. The consistency of contraction of various sections of the myometrium at different periods of the cycle and during childbirth is subject to the autonomic nervous system.
- The outer layer is the perimeter, which is the peritoneum . This serous membrane covers the entire anterior wall of the body, and at the border with the neck it bends and passes onto the bladder. Here the vesico-uterine space is formed. The cervix in front is not covered by the peritoneum and is delimited from the bladder by a layer of fatty tissue. In addition to the entire posterior surface of the body, the peritoneum covers a small area of the posterior vaginal vault. After this, the membrane bends and spreads over the rectum, forming a rectal-uterine pouch. Fluid can accumulate in this space due to ascites. Purulent inflammation, endometriosis or malignant tumors can spread here. Through the posterior wall of the vagina, access is made to this space during a diagnostic procedure - culdoscopy.
Purpose of ligaments
The uterus is an organ for which a clear, relatively constant position is of fundamental importance. This is achieved through the ligaments of the uterus.
The ligamentous apparatus performs three main functions:
- Suspension – attachment of an organ to the pelvic bones in order to fix the uterus in a stable position.
- Fixing – holding the uterus in a physiological position during gestation due to tensile ligaments.
- Supportive – forming support for internal organs.
Characteristics of the hanging apparatus
The suspension function of the uterus is carried out thanks to four pairs of ligaments:
- Round uterine ligaments containing smooth myocytes and connective tissue fibers. In appearance, they resemble cords 100–120 mm long, running from the corners of the uterus to the inguinal canal. Thanks to this direction, the round ligaments tilt the fundus of the uterus anteriorly.
- Broad uterine ligaments , which are derivatives of the peritoneum. They look like a “sail” stretched from the side surfaces of the uterus to the walls of the pelvis. At the top of these ligaments lie the tubes, and on the posterior surface are the ovaries. The space between the two leaves is filled with fiber in which neurovascular bundles are located.
- Suspensory ligaments of the ovaries , which are part of the broad uterine ligaments. They originate from the uterine tubes and are fixed to the walls of the pelvis.
- Proper ovarian ligaments , which fix the ovary to the lateral surface of the uterus.
Structure and location of fixing ligaments
The fixing ligaments of the uterus are:
- Cardinal (transverse) uterine ligaments, which are powerful bundles rich in vessels and nerves, consisting of smooth muscles and connective tissue fibers. These ligaments are modified, strengthened broad ligaments for which the transverse ligaments serve as support.
- The uterovesical (cervicovesical) ligaments are muscle-connective tissue fibers originating from the cervix and encircling the bladder. Due to this direction, the ligaments prevent the uterus from moving in the posterior direction.
- The uterosacral ligaments are composed of smooth muscle and connective tissue fibers starting from the posterior wall of the uterus, wrapping around the rectum and attaching to the sacrum. These fibers prevent the cervix from moving towards the pubis.
Supporting apparatus: muscles and fascia
The supporting apparatus of the uterus is represented by the perineum - the muscular-fascial plate. The perineum includes the genitourinary and pelvic diaphragms, consisting of two layers of muscles, as well as the perineal fascia.
Structure of the ovaries
The ovaries are paired glandular organs located in the female body on both sides of the uterus and connected to it by the fallopian tubes.
The shape of the ovaries resembles an egg flattened in front. The mass of this organ is approximately 7 - 10 g, length - 25 - 45 mm, and width - about 20 - 30 mm. The color of a healthy ovary can range from pinkish-blue to blue-purple.
On the outside, the ovary is covered with coelomic (germinal) epithelium. Beneath it lies the fibrous tunica albuginea, which forms the framework of the ovary. The functionally active substance of the organ, the parenchyma, is located even deeper. It consists of two layers. On the outside there is a cortical layer in which the follicles are located. The inner layer - granular (medullary substance) contains the egg.
In addition to the maturation of eggs, the ovaries perform a hormonal function, synthesizing estrogens (estradiol, estriol), gestagens (progesterone) and testosterone.
The fallopian tubes
The uterine (fallopian) tube is a paired hollow muscular organ that connects the uterine cavity with the ovary.
The fallopian tubes range in length from 100 to 120 mm. The diameter of the pipe is different along its entire length and varies from 2 – 5 to 8 – 10 mm.
The fallopian tube contains the uterine part, which communicates with the uterine cavity, as well as the isthmus, ampulla and infundibulum.
The funnel contains fimbriae. The longest of them, the ovarian one, approaches the tubal end of the ovary. This fimbria guides the egg into the tube.
The wall of the fallopian tube is represented mostly by smooth myocytes, located in two levels. The cells of the layer located more superficially are arranged longitudinally. Myocytes of the deeper layer wrap around the wall of the fallopian tube in a circle.
Due to this structure, the walls of the fallopian tubes have the ability to contract (peristalsis). This is necessary to move the egg into the uterine cavity.
But when exposed to certain unfavorable factors, the fertilized female reproductive cell is not evacuated into the uterus, but is attached to the wall of the tube. An ectopic (tubal, ectopic) pregnancy develops. An increase in the size of the embryo (embryo) causes a rupture of the wall of the fallopian tube. This leads to the development of massive internal bleeding.
How to find out?
The main method for diagnosing fibroids is ultrasound; the study is safe and painless. Although the doctor can detect large nodes with his hands. An ultrasound will help determine the cause of the bleeding: is it actually caused by fibroids or is it in the endometrium - the lining of the uterus. An ultrasound will show the nature of the location of the nodes - they are located outside the uterus, in its walls or inside the reproductive organ.
Nodules can be of different sizes - from a few millimeters in diameter to giant tumors weighing several kilograms. Our expert Larisa Nikolaevna Ulyatovskaya had to remove fibroids weighing up to 8 kg! Usually, the less often a woman goes to the gynecologist, the larger the size of her fibroid is found.
Structure of the circulatory system
The uterus and appendages are organs with a large circulatory network. In this regard, the pathology of the female reproductive system is often accompanied by heavy bleeding, which poses a danger to the patient’s life.
The main arteries are:
- The uterine artery, which is a branch of the internal iliac artery. This vessel supplies blood not only to the uterus itself, but also gives off branches that supply the tube, the broad uterine ligament, part of the vagina and the ovary. In the wall of the uterus, the artery forms an abundant network connected with the uterine artery of the opposite side.
- The ovarian artery on the left arises from the aorta. The right ovarian artery is most often a branch of the renal artery. This vessel supplies blood mainly to the ovaries, but also takes part in the nutrition of the uterus due to anastomoses with the uterine artery.
The vagina receives blood from three sources:
- The branches of the uterine arteries supply the portion of the vagina adjacent to the cervix;
- The inferior vesical and middle rectal arteries supply blood to the central part;
- The middle rectal and internal pudendal arteries deliver blood to the lower parts of the vagina.
From the upper parts of the uterus, tubes and ovaries on the right, venous outflow occurs into the inferior vena cava, and on the left into the left renal vein. Blood from the lower parts of the uterus, cervix and vagina flows into the internal iliac vein.
Outflow of lymph from the internal genital organs
The main collectors for the body of the uterus, tubes and ovaries are the lumbar lymph nodes. The iliac and sacral lymph nodes drain lymph from the cervix and lower body of the uterus. A small part of the lymph from the uterus may collect in the inguinal lymph nodes.
Next, all the lymph from the internal reproductive organs enters the lumbar lymphatic trunks and the lacteal cistern, from where it enters the internal jugular and left subclavian veins through the thoracic duct.
Innervation of the uterus and other female reproductive organs
Sensitive innervation of the external genitalia and the skin of the perineum is provided by the pudendal (genital) nerve, which is a branch of the sacral plexus. The same nerve gives off motor branches to the muscles that form the perineum.
The internal reproductive organs have only autonomic innervation. This means that the movements of the uterus are not subject to volitional efforts, but are carried out under the influence of neuro-vegetative changes. The body of the uterus has mainly sympathetic innervation, and the cervix has predominantly parasympathetic innervation.
The peculiarity of the autonomic innervation of the internal genital organs is that it occurs through the plexuses. The uterus receives innervation from the uterovaginal plexus, the ovary from the ovarian plexus, and the fallopian tubes from the ovarian and uterovaginal plexuses.
Functional changes during the monthly cycle
The monthly (menstrual) cycle is a complex of periodic changes in the endocrine system, ovaries and endometrium, aimed at conception. Cycle length may vary and range from 3 to 5 weeks (or 28 ± 7 days).
Functional changes in a woman’s body occur in three stages.
| Cycle phase | Changes in the ovaries | Changes in the endometrium |
| I Lasts from 7 to 22 days | Follicular phase | Menstrual phase |
| In the pituitary gland, under the influence of gonadoliberin, the synthesis and release of FSH1 and LH2 into the blood begins. Under the influence of FSH, several follicles mature in the ovaries, one of which becomes the main (dominant). This follicle begins to synthesize estradiol in large volumes, which, in turn, causes an increase in the synthesis of gonadotropins. The concentration of GnRH increases in proportion to the growth of the dominant follicle until a sharp release of LH from the adenohypophysis occurs. | If the egg has not been fertilized, epithelial detachment occurs. This is manifested by menstrual bleeding. | |
| II Duration – about 3 days | The dominant follicle continues to grow and secrete estradiol. A follicle that has reached maturity and is ready for ovulation is called Graafian vesicle (GV). The LH surge is the final stage of HP development. There is a release of dissolving enzymes that destroy the follicle wall. A mature egg, ready for fertilization, emerges from the GP cavity. | |
| III Lasts 13 – 14 days | Luteal phase | Secretory phase |
| After rupture, the walls of the GP collapse, and a new endocrine organ is formed - the corpus luteum (CL). VT releases estradiol, progesterone and androgens. If the egg has been fertilized and successfully attached to the uterine wall, the VT secretes progesterone until the placenta has formed and begins to secrete estrogen and progesterone. If pregnancy does not occur, the VT is destroyed, which causes a decrease in progesterone and estrogen levels. | Estrogen and progesterone cause the endometrial glands to mature. These glands begin to actively secrete, preparing the endometrium for attachment (implantation) of a fertilized egg. If pregnancy does not occur, in the absence of the influence of estrogen and progesterone of the corpus luteum, the endometrium begins to swell and necrotize. Eventually it is rejected and the cycle starts again. | |
FSH – Follicle stimulating hormone.
LH – Luteinizing hormone.
Change your lifestyle
What is the cause of the disease? The longer doctors search for an answer to this question, the more difficult it is for them to answer it. It is assumed that fibroids react to an excess amount of female sex hormones - estrogens, relative to another sex hormone - progesterone. It appears only during the reproductive period, when the ovaries produce estrogens. While the ovaries are functioning, the fibroid does nothing other than grow. At best, it is in a stable state. In postmenopause, fibroids no longer appear, and those small nodes that a woman has at this point begin to decrease in size.
But why did fibroids begin to appear more often? Obviously, this is due to our lifestyle - high pace, heavy loads. The body, as it were, warns that it can’t cope, and that’s why it gets sick. Proof of the correctness of this view are examples when women had their uterus removed due to large nodes, they did not change their lifestyle after the operation, and fibroids subsequently appeared in their mammary glands.
Fibroids can occur after stress. Doctors say that if you have had unpleasant changes in your life - you divorced your husband, lost your job, are quarreling with a child who has entered a difficult age - go to the gynecologist in a month or two. Alas, at this time something will definitely worsen or appear for you.
The heat and smog this summer also brought us unpleasant surprises. Gynecologists have recorded cases of ultra-fast growth of fibroids in one month.
There is also a theory that fibroids are the consequences of dissatisfaction with personal life. They occur in unhappy women.
Pathologies and anomalies
As a result of various adverse effects, the structure of the uterus or its position in the pelvic cavity may be disrupted.
Among the anomalies of the structure of the uterus, the following forms are distinguished:
- Organ doubling .
At the same time, there is always a doubling of the vagina. Most often, one of the uteruses is better developed than the other. In this case, a normal monthly cycle occurs in both uteruses, and pregnancy can develop in each of them. - Bicornuate uterus .
With this anomaly in the fundus, the organ is divided into two horns that connect at the cervix. Clinically, this deviation is manifested by menstrual irregularities, miscarriages and infertility. One of the horns may be underdeveloped (in this case, it looks like a cord or cavity formation communicating with the uterus). - Saddle-shaped (arched) uterus .
It is a variant of a bicornuate uterus, in which the separation of the fundus is minimally expressed. Most often, this anomaly is asymptomatic and is an incidental finding. - Intrauterine septum .
This is a malformation of the organ in which the uterus is divided into two cavities, which are either completely isolated from each other (complete septum) or communicate with each other in the cervical area (incomplete septum). Clinically, a uterine septum is manifested by habitual miscarriages, and less commonly by the inability to become pregnant.
The most common forms of abnormal location of the uterus are the following:
- Uterine prolapse .
In this case, the vaginal part of the cervix will not stand beyond the border of the genital slit. Otherwise, they talk about uterine prolapse. - Elevation of the uterus .
In this case, the fundus of the uterus is located above the upper plane of the pelvis. Elevation of the organ can be due to adhesions, accumulation of menstrual blood with atresia of the hymen, or with tumors of the rectum. - Rotation of the uterus. With this anomaly, the cervix and body of the uterus rotate in one direction. Unlike rotation, when the uterus is twisted, the cervix remains in place, and only the body turns.
- Displacement of the entire uterus .
This anomaly can manifest itself in various forms: displacement forward (anteposition), backward (retroposition), left or right (synistroposition or dextroposition).
Diseases
Pathological neoplasms are the first type of uterine diseases.
Uterine fibroids.
This is a benign tumor originating from the muscle layer. There are several types of myomatous nodes:
- Submucosal. Occurs most often in women of fertile age;
- Intramural nodes are located deep in the myometrium;
- Subserous nodes are localized outside the uterus, adjacent to the perimeter.
The main symptoms of uterine fibroids are heavy menstruation, miscarriages, and infertility.
Uterine fibroids.
If uterine fibroids contain mainly myocytes in their structure, then fibroma is a benign tumor consisting of connective tissue cells. The same forms of fibroma are distinguished as in the classification of fibroids. Separately, uterine fibroids are distinguished - a tumor containing muscle cells, but with the obligatory inclusion of fibrous tissue. The clinical manifestations of fibroids are identical to those of uterine fibroids.
Endometrial polyps are benign growths of blood vessels covered with epithelium. There are several types of polyps:
- fibrous - pale, round or oval, dense, smooth formations on a stalk, up to 15 mm in size;
- glandular-cystic - large (up to 60 mm), oblong, smooth, pale pink, gray-pink or yellowish;
- adenomatous - dull gray formations up to 15 mm in size.
Polyps may be asymptomatic or cause bleeding, pain and infertility.
Prolapse of the reproductive organ
Prolapse (loss) of the female reproductive organs is the movement of the vagina, cervix or uterine body beyond the genital opening.
There are three degrees of genital prolapse:
- I degree (not true prolapse): the cervix prolapses, but it does not extend beyond the entrance to the vagina;
- II degree: incomplete prolapse - movement of the cervix beyond the border of the genital fissure, but the uterus is in the pelvic cavity;
- III degree: complete prolapse - the entire uterus falls out.
The main cause of uterine prolapse is dysfunction of the ligamentous apparatus. This can be caused by connective tissue dysplasia, inflammatory and adhesive processes in the pelvis, impaired innervation and blood supply to the genital organs.
At the first stage of prolapse, there may be no complaints. Sometimes women note a feeling of heaviness in the perineum, discomfort when walking, pain in the lower back and sacrum.
The most characteristic symptom of the second and third stages is a formation that has fallen outside the genital slit.
Upon examination, the prolapsed parts of the cervix and body of the uterus have a bluish tint. The reason for this is poor circulation in the prolapsed areas of the organ.
Conservative management of prolapse of the female reproductive organs is impossible! The only way to treat this pathology is surgery.
The operation is aimed at returning organs to their physiological location, restoring and strengthening the supporting structures of the uterus and treating associated pathologies.
"Uterine rabies"
This term hides two diseases that belong more to the field of pathological psychology than gynecology.
Nymphomania (“disease of forest nymphs”) is female hypersexuality, excessive attraction to a man. This disorder is manifested by constant sexual dissatisfaction and the desire to constantly change sexual partners.
Hysteria (“the monkey of all diseases”) is a disorder characterized by a pathological need to attract attention to oneself. Although this condition also occurs in men, it is most pronounced in women. Hysteria can manifest itself with almost any known symptoms - uncontrollable laughter and/or crying, convulsive seizures, fainting, blindness, deafness, muteness, loss of sensitivity. It is not difficult to distinguish hysteria from a true disorder. It is enough to remember that hysteria manifests itself only in the presence of people whose attention the patient is trying to achieve.
Both nymphomania and hysteria require treatment from a psychiatrist and psychotherapist. But sometimes these disorders reach such severity that they require differential diagnosis with diseases of the nervous system (epilepsy, damage to the frontal lobes of the brain, stroke).
"Dense uterus"
A dense uterus is not an independent disease, but a symptom that accompanies the development of many pathological conditions. Uterine thickening means focal or total thickening of its walls, identified during a gynecological examination. The most common causes of the development of a dense uterus are myomatous nodes and foci of adenomyosis.
Adenomyosis (internal endometriosis) is a benign disease, which is based on the growth of the endometrium into the muscular layer of the uterus. The main symptoms to suspect adenomyosis are menstrual irregularities, intense dull pain in the lower abdomen, pain during sexual intercourse, and “chocolate”-colored discharge in the middle of the cycle.
If during the examination the gynecologist reveals a hardening of the uterus, an ultrasound should be performed to identify the cause.
Disease prevention
There are no specific prophylactic treatments for diseases of the reproductive organ, but gynecologists advise women:
- live a full and regular sex life;
- try to avoid abortions and gross surgical interventions;
- do not lift heavy objects;
- use barrier methods of protection during questionable sexual contacts
- carefully monitor your health and regularly undergo scheduled medical and gynecological examinations.
Women who have recently given birth to a child or are on the verge of menopause need to be especially attentive, since it is they who, due to unstable hormonal levels, are most susceptible to the development of endocrinological dysfunctions that provoke pathological processes in the reproductive organ.
The uterus is the basis of the female reproductive system, whose main task is the reproductive function of the female body. Created for the bearing and development of a child, the organ, which in photographs has the shape of an inverted triangle, is responsible for the normal functioning of the hormonal system and the stable course of the menstrual cycle.
Diseases of the uterus that develop under the influence of infectious, endocrine or medical pathologies can cause severe pain and bleeding, and are also the main cause of female infertility.
Removal of the uterus and postoperative period
Indications for removal (amputation, extirpation) of the uterus (hysterectomy) are large myomatous nodes, malignant tumors of the uterus, widespread adenomyosis, heavy uterine bleeding, and severe inflammation of the endometrium.
With a favorable outcome, it is possible to save the ovaries and cervix. This gives the woman the opportunity to have a normal sex life and avoid the use of hormone replacement therapy. In addition, eggs stored in the ovaries can be used for surrogacy.
During the postoperative period of a hysterectomy, pain and bleeding always occur.
The pain bothers the woman for about a week and is nagging in nature. If the pain intensifies and becomes sharp and cramping, this indicates the development of complications.
Bloody discharge occurs due to the existence of a wound surface. By the end of the second week they gradually stop.
Long-term consequences are associated with a violation of the location of organs in the pelvis. The bladder moves backward, which can manifest itself in various urinary disorders. The intestines shift downward, which can ultimately cause prolapse of hemorrhoids.
If regional lymph nodes were removed along with the uterus, the outflow of lymph from the lower extremities is disrupted, which leads to the development of lymphostasis. This is manifested by swelling, heaviness, pain, and tissue malnutrition.