Pulmonary embolism (PE) is a blockage of the artery that transports venous blood from the heart to the lungs for oxygenation by a blood clot.
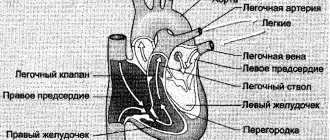
A pathological clot (thrombus) can form in the veins of the legs, arms or pelvis, or in the atria and ventricles of the heart. This clot is carried by the blood into the pulmonary circulation and blocks the pulmonary artery or its branch (thromboembolism of the branches of the pulmonary artery, thromboembolism of the small branches of the pulmonary artery). If a pulmonary artery or a large branch is blocked by a massive thrombus, death can occur instantly. When small branches of the pulmonary artery in part of the lung are blocked by a thrombus, blood circulation and gas exchange (oxygen and carbon dioxide) worsen and a pulmonary infarction occurs.
If the damage is extensive, the human body ceases to receive a sufficient amount of oxygen and hypoxia occurs. With critical hypoxia due to pulmonary embolism, the patient may die.
Unfortunately, the development of pulmonary embolism is often so rapid that it is not possible to establish a diagnosis during life. The chances of recovery are significantly increased by early diagnosis and anticoagulant therapy in the first hours of the disease.
Thromboembolism spares neither adults nor children, but the main risk group is people aged about sixty years.
Embolism can be gas (the lumen of the artery is closed by an air bubble), bacterial (the reason for blocking the blood flow is a clot of microorganisms), mechanical (clogging with fatty deposits, bone marrow particles).
1 Blood test for pulmonary embolism
2 Blood test for pulmonary embolism
3 Blood test for pulmonary embolism
General information
Thrombosis is the formation of a blood clot in a blood vessel that interferes with blood flow.
Its danger lies in the fact that there is a danger of a blood clot or its fragment moving through the bloodstream - an embolism and blockage of another vessel occurs. For example, supplying the brain or heart. Pulmonary embolism often occurs, which leads to severe organ dysfunction or death. What is pulmonary embolism in medicine? Pulmonary embolism is an acute occlusion (blockage) of the pulmonary artery trunk or its branches (main, lobar or segmental). Occlusion occurs more often due to embolization of a thrombus from the right half of the heart or veins of the lower extremities. The incidence of this disease increases with age and the age of such patients is 62 years.
Pulmonary artery thrombosis is an emergency in cardiac resuscitation and is often the cause of patient death. Seriously ill patients with a high risk of pulmonary embolism and death are patients with cardiac arrhythmias, cancer pathology , and thrombosis of the veins of the lower extremities .
Diagnosis is often difficult, so the disease is often not recognized. Early diagnosis and initiation of intensive treatment are important in the prognosis of this disease. The code for pulmonary embolism according to ICD-10 is I 26.
Air bubble blockage
In addition to blood clots, an air bubble may enter the bloodstream. This rarely happens spontaneously. Much more often as a result of medical intervention.
Contrary to popular misconception, a dropper after the medicine has been poured out is not capable of causing air to enter the bloodstream due to a difference in blood pressure and indicator in the system.
That is why special stands are used and glass containers with medicine are placed high.
Moreover, for the development of an embolism, at least 5 cubic meters of gas or more are required. This amount can only penetrate during open surgery or arterial catheterization. This option is much less common.
Then everything develops along an identical path. Blockage, disruption of cellular respiration, possible death of the patient without high-quality and urgent treatment. In some cases, it is impossible to radically influence the situation at all.
Pathogenesis
The main thing in the pathogenesis of pulmonary embolism is occlusion of the pulmonary artery and its branches by embolism, which leads to disruption of hemodynamics and gas exchange. During occlusion, the pressure in the pulmonary artery increases by almost 50% due to vasoconstriction associated with the release of serotonin and thromboxane A2 . A sharp increase in pulmonary resistance causes expansion of the right ventricle, stretching of myocytes and tension of the ventricular walls. Lengthening the time of its contraction towards diastole causes protrusion of the septum into the left ventricle. Therefore, left ventricular filling becomes more difficult, cardiac output decreases, and systemic hypotension .
Massive infiltrates are found in the ventricular myocardium, which further destabilizes hemodynamics. Right ventricular failure due to pressure overload is a leading cause of death. Respiratory failure is also associated with hemodynamic disturbances. A decrease in cardiac output causes desaturation of venous blood. The appearance of zones of reduced blood flow causes a mismatch between perfusion and ventilation. Small emboli in the periphery do not affect hemodynamics, but cause pulmonary hemorrhage with hemoptysis, pleurisy and pleural effusion (“pulmonary infarction”).
Development mechanism
As stated, the immediate cause of pulmonary embolism is blockage of the pulmonary artery by a foreign structure. There are options here. The most common occurrence is thrombi (blood clots).
Similar formations form in the upper, lower extremities, and the heart itself (somewhat less frequently). They are not always rigidly attached to the place of their formation.
When exposed to a negative factor: pressure, impact, the clot can break off and move along the bloodstream. Further, everything depends on its size and the will of chance.
The thrombus will stop in one or another part of the vascular network, it is likely that it will be in the pulmonary artery.
The following is a standard scheme. A mechanical obstacle is formed to the flow of blood in a small circle.
Initially, it is poor in oxygen (venous), and is not sufficiently saturated with O2, which means the same meager amount enters the heart, is released into the aorta and circulates throughout the body.
For obvious reasons, such blood cannot meet the oxygen needs of cells. Therefore, severe starvation occurs against the background of cellular respiration disorder.
In the short term, this leads to cerebral ischemia and multiple organ failure. Death may occur within a matter of days. If a total blockage of the pulmonary artery occurs, death occurs almost instantly.
Classification of pulmonary embolism
The 2008 classification of the European Society of Cardiology identifies:
- Low risk pulmonary embolism.
- Intermediate.
- Tall.
Clinical classification takes into account the caliber of the pulmonary arteries and the percentage of pulmonary involvement:
- Massive (cessation of blood flow in less than 50% of the pulmonary bed). It is of great clinical importance because it is accompanied by shock or decreased pressure, pulmonary hypertension. With occlusion of the trunk, pronounced cardiorespiratory disorders develop. Under such conditions, the right ventricle cannot perform the function of a pump and its cavities quickly expand, and tricuspid valve insufficiency develops. The septum between the ventricles shifts to the left (towards the left ventricle), which is accompanied by poor filling in diastole. Due to the cessation of blood flow, the pulmonary parenchyma is not supplied with blood, but is ventilated. In the affected area, obstruction of the bronchi occurs, the alveoli collapse and surfactant is not formed in them, which contributes to the development of atelectasis (collapse) of the lungs on days 1-2 of embolism. Such hemodynamic disturbances and impaired pulmonary function often lead to the death of the patient.
- PE of small branches of the pulmonary artery (cessation of blood flow is noted in less than 30% of the pulmonary bed). In this case, there is occlusion of lobar and segmental small branches. The disease is not severe without hemodynamic disturbances and patients only need anticoagulant therapy. The pulmonary circulation has compensatory capabilities and there is a possibility of independent dissolution of blood clots when fibrinolysis .
- Submassive—thromboembolism of the branches of the pulmonary artery (cessation of blood flow in less than 30-50% of the bed). It manifests itself as right ventricular failure, and hemorrhagic infarctions form in the lungs.
First aid
Carried out urgently. During the acute period, nothing can be done. Death will come anyway. Within a matter of seconds, a person will die, even if he is in a fully equipped intensive care unit. This is an axiom.
The same applies to the decompensated phase, when there are still chances to “get the person out.” The main action is to call an ambulance. It is impossible to correct the violation on your own.
Before the brigade arrives, the patient must be laid down. The head should be slightly elevated. This can be achieved by placing a pillow or using an improvised cushion.
There should not be a strong anatomical bend, so as not to provoke a stroke. Everything in moderation.
The drugs cannot be used. It is not known how the body will react to oral administration of medications. The condition may worsen.
Complete peace is ensured. Emergency care for pulmonary embolism involves placing the arms and legs below the heart. That is, you should not place cushions under your limbs, and that is why the lying position is the most preferable.
It is recommended to measure blood pressure and heart rate every 10 minutes. Capture the dynamics. Upon arrival of specialists, report on the condition of the victim and talk about objective indicators.
Then you can only accompany the patient to the hospital in order to help with moving, if necessary, and convey the necessary information.
Causes of pulmonary embolism
Considering the causes of pulmonary embolism, it is necessary to highlight a number of diseases and conditions that are accompanied by the formation of blood clots, which are the basis of embolism:
- Varicose veins and phlebothrombosis of the deep veins of the lower extremities. This pathology causes thromboembolism in 90% of cases. The threat is posed by floating blood clots, which are freely located in the lumen of the vessel and are connected to the vein wall in only one part.
- Congestive heart failure , overstretching of the right ventricle, which creates conditions for the formation of blood clots in the cavity of the right ventricle.
- The use of oral contraceptives and pregnancy , which are associated with an increased risk of blood clots.
- Antiphospholipid syndrome (autoimmune thrombotic vasculopathy ), manifested by venous and arterial thrombosis . Vessels of different sizes may be affected - capillaries and large arterial trunks. Deep vein thrombosis of the lower extremities is a typical manifestation of antiphospholipid syndrome. Repeated pulmonary embolisms are typical.
- Central venous catheterization.
- The presence of malignant diseases.
- Carrying out chemotherapy .
- Spinal cord injury.
- Forced immobilization after surgery, during a stroke , fractures of the pelvis and limbs.
- Hip replacement.
- Atrial fibrillation.
- Polytrauma and extensive surgery.
- Hereditary predisposition to thrombosis ( thrombophilia ), which is caused by mutations of certain genes, deficiency of antithrombin III, deficiency of protein C and S.
Considering pulmonary thrombosis , it is necessary to note the risk factors for this condition:
- Damage to the venous endothelium.
- Obesity.
- Age.
- Hypercoagulation.
- Slowing of venous blood flow.
- Infection.
- Blood transfusions.
- Migraine.
- The combination of several factors is accompanied by a high risk of thrombus embolism .
Diagnostics
Diagnosis of PE begins with a clinical assessment by a physician and may then include specialized tests that can confirm or rule out the diagnosis.
Clinical assessment.
The first step in diagnosing PE is for the doctor to assess whether the person is likely to have PE. The doctor makes this assessment by performing a thorough medical history, assessing risk factors for deep vein thrombosis (DVT), performing a physical examination, measuring the oxygen concentration in the blood, and possibly performing an ultrasound to detect DVT.
Non-invasive tests
After a clinical evaluation by a doctor, special tests, such as blood tests or imaging studies, may be needed.
- D-dimer assay . If the likelihood of thromboembolism is considered low, your doctor may order a D-dimer test. A D-dimer test is a blood test that measures the presence of abnormal levels of clotting activity in the blood, which is expected if a person has DVT or PE. If the clinical likelihood of PE is low and the D-dimer test is negative, PE can be ruled out and the doctor will begin to consider other possible causes of the symptoms.
If the likelihood of PE is assessed as high, or if the D-dimer test is positive, then either a V/Q scan (ventilation/perfusion scan) or a computed tomography (CT) scan of the chest is usually performed.
- V/Q scan : A V/Q scan is a scan of the lungs that uses a radioactive dye injected into a vein to evaluate the flow of blood into lung tissue. If a pulmonary artery is partially blocked by an embolus, less radioactive dye will be delivered to the corresponding portion of the lung tissue and will be visible on the screen.
- Computed tomography (CT) : A CT scan is a non-invasive computerized x-ray procedure that allows the doctor to visualize the pulmonary arteries to see if there is obstruction caused by an embolism.
- Pulmonary angiogram : The pulmonary angiogram has long been considered the gold standard for detecting PE. If the diagnosis is unclear after performing the above tests, your doctor may order a pulmonary angiogram.
Treatment of pulmonary embolism
Once the diagnosis of pulmonary embolism is confirmed, therapy begins immediately. If there is a very high probability of pulmonary embolism, medical therapy may be started even before the diagnosis is confirmed.
Blood thinners - anticoagulants .
The main treatment for pulmonary embolism is the use of anticoagulant blood thinners to prevent further clotting.
Symptoms of pulmonary embolism (PE)
Making a diagnosis in the early stages is difficult, only in the acute course the symptoms of pulmonary artery thrombosis appear manifestly and suddenly: shortness of breath , chest pain , tachycardia , decreased blood pressure. In this case, the patient has risk factors for thromboembolism - varicose veins and phlebothrombosis .
Hypotension and shock indicate central thromboembolism . Severe acute shortness of breath also develops with central pulmonary embolism. With the same localization, chest pain is angina-like in nature . Massive thromboembolism is accompanied by signs of right ventricular overload - this is the bulging of the jugular veins in the neck and the right ventricular gallop rhythm.
Signs of PE in subacute cases are not very specific. Respiratory and right ventricular failure progresses, infarction pneumonia and hemoptysis appears. With a recurrent course, repeated attacks of shortness of breath , there are signs of pneumonia and periodic fainting occurs. If the thrombus blocks small arteries in the periphery, shortness of breath is minor and transient. Only in the case of chronic lung pathology or heart failure does shortness of breath worsen. Sometimes PE is asymptomatic.
The clinical picture depends on the caliber of the blocked vessel and, accordingly, the degree of involvement of the pulmonary vascular bed. Massive pulmonary embolism (most often thrombosis of the main branch ) occurs with symptoms of shock or a decrease in pressure by 40 mm Hg. Art. for a short time that is not associated with arrhythmia , sepsis , or decreased blood volume. Characteristic shortness of breath , cyanosis , and sometimes fainting .
Submassive pulmonary embolism (obstruction of lobar or segmental branches) is manifested by right ventricular failure (swelling of the neck veins, pallor, cyanosis), but without arterial hypotension. The patient develops shortness of breath , tachycardia , pulmonary infarction (fever, cough, pulmonary-pleural pain, sputum streaked with blood).
In non-massive cases, there are no signs of right ventricular failure, and the pressure is normal.
Treatment
There are not many techniques. However, those that are available provide good chances of success.
In the early stages, medication is used. Anticoagulants are used. They thin the blood (relatively speaking, in fact, the effect of these medications is indirect, without going into details).
In the first 6 days, intravenous injections of Heparin are performed. This is a dangerous drug with many side effects. Therefore, constant monitoring of the patient’s condition is necessary.
If the dynamics are positive, after leaving the walls of the cardiology department, softer analogs are prescribed in tablet form. For example, Warfarin, Marevan, Warfarex. At the discretion of the specialist.
The duration of therapy after an acute condition is 3-12 months. The timing is determined by the doctor. You cannot adjust the duration on your own.
In a favorable scenario, it is possible to achieve a stable reduction of symptoms in the first days. Total recovery is observed after a few months. The patient is considered conditionally recovered.
Emergency conditions or severe forms of pulmonary embolism require the use of thrombolytics. For example, Urokinase, Streptokinase in shock dosages. They dissolve blood clots and help normalize the flow of fluid connective tissue.
An extreme technique involves performing abdominal surgery to mechanically remove the blood clot (embolectomy). This is a dangerous, difficult way. But there are no options, and besides, the risks are justified. The patient is already in danger of death, it certainly won’t get any worse.
In the future, it is recommended to carefully check for cardiovascular and hormonal pathologies in order to eliminate the root cause of thromboembolism. This will minimize the likelihood of relapse.
Tests and diagnosis of pulmonary embolism
Instrumental diagnostics of this condition includes:
- Chest X-ray . In the lungs, discoid atelectasis , a raised dome of the diaphragm, or pleural effusion . All these signs are nonspecific, but exclude various causes of pain and shortness of breath.
- ECG.
- Echocardiography . It is of key importance in diagnosis, especially in patients with unstable hemodynamics. This test directly detects blood clots in the right side of the heart, and blood clots in the large arteries of the lungs (trunk and main branches). An indirect sign of pulmonary embolism detected by echocardiography is overload of the right chambers. An indirect sign of pulmonary artery thrombosis is identified - overload of the right ventricle: expansion of the ventricular cavity, unusual movement of the septum between the ventricles and a D-shaped left ventricle.
- Ultrasound of the deep veins of the extremities.
- A special research method is ventilation-perfusion scintigraphy . This is a safe study that involves the intravenous administration of albumin microspheres that are labeled with technetium. Albumin microspheres block pulmonary capillaries and lung perfusion is assessed based on this feature. This study is complemented by a ventilation study, which increases the specificity of the examination (in case of thrombosis, ventilation in segments of the lungs in which there is poor blood supply remains normal). That is, a discrepancy between ventilation and perfusion is detected. Radioactive radiation during scintigraphy is lower than during CT angiography. Perfusion scintigraphy alone can be performed in patients with a normal radiograph.
- CT angiography . This study has become the method of choice for diagnosing pulmonary vascular pathology. The pulmonary arteries can be viewed down to the segmental branches. The specificity of the method is 96%. The technique is optimal for diagnosing a patient whose condition is stable. In another case, the patient cannot be transported from intensive care.
- Pulmonary angiography is considered the gold standard for diagnosing PE. However, it is rarely performed since a less invasive test, CT angiography, has become available. Diagnosis is based on identifying a blood clot that causes a defect in the filling of the pulmonary artery branch or is completely absent. The method allows you to obtain images of peripheral pulmonary arteries and detect blood clots of 1-2 mm in the smallest arteries. A contrast agent is injected for the study.
ECG signs of PE and radiographic signs
Blood tests:
- D-dimer is a fibrin degradation product. Its increase in plasma is observed during acute thrombosis - this is explained by the activation of fibrinolysis and coagulation. A normal D-dimer level makes the diagnosis of PE unlikely. Also, this indicator is nonspecific, since fibrin overproduction is observed during inflammation, bleeding, myocardial infarction , aortic aneurysm , oncological processes, trauma, and surgery. The specificity of D-dimer for thrombosis decreases with age. This indicator is paid attention to during treatment, since an increase in its level after the end of anticoagulant treatment indicates a risk of relapse.
- of brain natriuretic peptide increases , which is associated with distension of the right ventricle. The degree of increase is proportional to the severity of the patient. However, an increase in this marker is nonspecific, since it can be observed with myocardial ischemia , left ventricular hypertrophy , sepsis and tachycardia . However, the absence of a significant increase indicates a favorable prognosis for pulmonary embolism.
Diagnosis of thromboembolism
It is often very difficult to diagnose PE due to the fact that its symptoms are similar to many other CVDs. Therefore, for the correct differentiation of the disease, the experience of the doctor and decent technical equipment of the clinic are very important.
After talking with the patient and analyzing his complaints, the doctor conducts a physical examination, measures blood pressure and pulse, and listens to the heart and lungs with a stethoscope. Next, laboratory and instrumental diagnostics are prescribed:
- clinical blood test, biochemical blood test, blood test for D-dimer;
- electrocardiography (ECG);
- echocardiography (ultrasound of the heart);
- chest x-ray;
- duplex/triplex scanning of the veins of the lower extremities;
- MSCT of the chest organs;
- ventilation-perfusion lung scintigraphy.
1 ECG for thromboembolism
2 Diagnosis of pulmonary embolism in MedikCity
3 ECHO-CG for thromboembolism
In children
Thrombosis in children occurs much less frequently. For their occurrence, a combination of acquired and congenital factors is necessary. Of the hereditary ones, it is worth noting the hereditary decrease in the activity of antithrombin III and proteins C, S, which are natural anticoagulants. Acquired factors:
- severe somatic diseases
- infectious diseases;
- systemic connective tissue diseases;
- malignant tumors;
- connective tissue dysplasia ;
- hemolytic anemia;
- antiphospholipid syndrome.
The most important factor in thrombosis is the use of an intravascular catheter. Up to 80% of thromboses are associated with catheterization. In children, pulmonary embolism is often associated with deep vein thrombosis. Venous thrombosis in children is preceded by infection, thrombocytopenic purpura , antiphospholipid syndrome , and in some, excessive insolation. Recurrent pulmonary embolism also occurs, but the source of thrombosis cannot be identified. PE in children is often mistakenly regarded as pneumonia .
X-ray of the lungs with pulmonary embolism
Pathological changes on chest x-rays are detected in most cases of pulmonary embolism, but are not specific. The most commonly detected pathological changes on radiographs include atelectasis (collapse) of part of the lung, pleural effusion, decreased transparency of the lung tissue, and high standing of the right or left dome of the diaphragm. Classic X-ray signs of pulmonary infarction are the presence of a wedge-shaped (triangular) darkening, with a wide base facing the pleura, the apex of which is directed towards the root of the lung (Hampton's tubercle), or a decrease in the severity of the vascular pulmonary pattern in the zone of thromboembolism (Westermarck's sign).
Other changes on radiographs detected with pulmonary embolism are expansion of the central pulmonary artery with its sharp break - “cut off roots”, an increase in the size of the heart (especially its right parts), as well as signs of pulmonary edema. These changes can be combined with acute clinical symptoms of cor pulmonale. The absence of changes on the chest x-ray in a patient with severe respiratory distress and hypoxemia, but without signs of bronchospasm or atypical blood flow in the heart, is highly suspicious for PE. In general, chest radiography cannot be used to confirm or refute the diagnosis of PE; however, radiography and ECG may be helpful in confirming alternative diagnoses.
Prevention of pulmonary embolism
- Primary prevention of embolism after surgery on the pelvic organs and orthopedics.
- If the risk of thromboembolism is low, prevention involves the use of compression stockings or elastic compression with an elastic bandage of the lower extremities.
- enoxaparin or fondaparinux or dabigatran until discharge .
- If the risk is high, these recommendations should be followed for a month.
- New oral anticoagulants are registered for primary prevention after orthopedic surgery.
There are also non-surgical patients (chronic heart failure class III-IV), who are also at risk for pulmonary embolism. Their choice of anticoagulant is the same. The standard of treatment is enoxaparin .
Secondary prevention is the prevention of recurrent thromboembolism. Without prophylaxis, recurrence of pulmonary embolism within the first three months is observed in 20-45% of patients. With prevention, the number of relapses is reduced to 1%. Warfarin is used for prevention , and for the first six months, cancer patients are prescribed low molecular weight heparins ( Fraxiparin , Fraxiparin Forte , Clexane , Enixum , Fragmin , Daltep ), then they are transferred to oral medications ( vitamin K antagonists - Warfarin , Warfarex ).
How long should I take them? To do this, the risk of bleeding is assessed based on risk factors (age 65 years or older, history stroke malignant tumor , renal and liver failure , diabetes mellitus , low platelet levels, anemia and others). The risk of bleeding is high if more than two risk factors combine.
It is also possible to use “new” anticoagulants for secondary prevention, which are included in the American Guidelines for the prevention of pulmonary embolism. Rivaroxaban ( Xarelto ) is superior in long-term treatment and can be prescribed for 6-12 months with a low risk of bleeding, providing protection against relapse.
Prevention
Preventing pulmonary embolism is preventing deep vein thrombosis; The need for it depends on the patient's risks, including:
- type and duration of surgery;
- concomitant diseases, including cancer and hypercoagulability disorders;
- presence of a central venous catheter;
- History of DVT or PE.
Bedridden patients and patients undergoing surgery, especially orthopedic surgery , have an advantage, and most of these patients can be identified before a clot forms. Preventative recommendations include low-dose unfractionated heparin, low-molecular-weight heparins, warfarin, fondaparinux, oral anticoagulants (rivaroxaban, apixaban, dabigatran), and the use of compression devices or elastic compression stockings.
The choice of drug or device depends on various factors, including patient population, perceived risk, contraindications (such as risk of bleeding), relative costs, and ease of use.
Healthy people who simply want to protect themselves from this disease need to undergo constant diagnostics (once every 6 months), exercise, keep their weight under control and be sure not to smoke.
Consequences and complications
- Hemodynamic disturbances (increased vascular resistance in the pulmonary artery system and increased afterload on the right ventricle).
- Respiratory failure.
- Hypoxia.
- Pulmonary-pleural complications ( atelectasis , pleurisy , lung abscess , pulmonary infarction , pneumonia , pyopneumothorax , pleural empyema ).
- Post-embolic pulmonary hypertension .
Consequences of pulmonary embolism
With timely provision of sufficient medical care to patients with mild forms of pulmonary embolism, the prognosis is favorable. In the case of pronounced changes in the organs of the cardiovascular and respiratory systems, mortality exceeds 30%. With massive thromboembolism, the prognosis is the most unfavorable; mortality can reach 100%.
PE is a dangerous condition that ranks third in the list of leading causes of death.
The main factors determining the prognosis for pulmonary embolism:
- timeliness of treatment;
- presence of concomitant cardiovascular diseases;
- presence of risk factors.
The main danger of pulmonary embolism is death, which occurs in severe cases of the disease. However, even in the presence of mild or moderate severity of the disease, immediate initiation of treatment is required.
In the absence of timely assistance, complications may develop:
- pulmonary infarction;
- pleurisy and pneumonia;
- acute renal failure;
- embolism of blood vessels in the systemic circulation;
- chronic pulmonary hypertension.
List of sources
- Vatutin N.T., Sklyannaya E.V., Eshchenko E.V. /Pulmonary embolism. Review of recommendations of the European Society of Cardiology for diagnosis and treatment (2014 // Practical Angiology. - 2015. - No. 1 (68). - P. 5-18.
- Russian clinical recommendations for the diagnosis, treatment and prevention of venous thromboembolic complications // Phlebology. — 2015.— No. 4, issue 2. 46 p.
- Vatutin N.T. Emergency cardiology. - Donetsk, 2011. - 236 p.
- Vatutin N.T., Kalinkina N.V., Perueva I.A. /Pulmonary embolism // Practical angiology. – 2011. – No. 2. – P. 32-40.
- Vatutin N.T., Kalinkina N.V., Eshchenko E.V. and others. Pulmonary embolism (basic information and own observation) // Heart and Vessels. – 2013. – No. 1. – P. 120-123.
Treatment of pulmonary embolism
The main directions of treatment for patients with pulmonary embolism:
- life maintenance;
- elimination of pathological reflex reactions;
- elimination of occlusion;
- relief of collapse;
- decrease in pressure in the small circle;
- oxygen therapy.
To treat pulmonary embolism, a complex of medications is used. Among them are anticoagulants (Heparin, Warfarin) and thrombolytics (Urokinase, Streptokinase).
Venous thromboembolism in most cases (except for absolute contraindications) requires the use of anticoagulants (Heparin, Warfarin), which affect blood coagulation factors and prevent excessive thrombus formation. Heparin has a rapid effect, so its use is indicated in the early stages of pulmonary embolism. The drug is administered intravenously or subcutaneously. Most patients require treatment with Heparin for 5 days, followed by oral Warfarin, an indirect coagulant, which should be taken for at least 3 months.
When starting treatment with Warfarin, it may be necessary to perform tests twice a week to determine the optimal dosage. Next, you should determine the coagulogram once a month, since the drug affects the blood coagulation system. In addition, the drug has side effects such as bleeding, headaches, nausea, vomiting, so you should reconsider your lifestyle: watch your diet, limit alcohol consumption, take the drug at one time of day, eliminate all medications, if you need to use other drugs, consult with doctor.
Thrombolysis is used to treat PE in high-risk patients. The greatest effectiveness is achieved when thrombolytics are used in the first 48 hours after embolism. The “therapeutic window”, which determines the advisability of such treatment, is up to 2 weeks from the onset of the disease.
Thrombolytics are drugs that eliminate a blood clot. Drugs of choice: Alteplase, Streptokinase, Urokinase. These are powerful drugs, so before use you should evaluate the indications and possible risks: the use of such drugs can lead to the development of bleeding, including intracerebral hemorrhages.
Surgical treatment of pulmonary embolism is performed in patients with contraindications to thrombolysis. This is a complex manipulation that can lead to serious consequences, including death, so the doctor, when deciding on an intervention, evaluates the indications and contraindications.
Indications for surgical treatment of pulmonary embolism:
- massive thromboembolism;
- lack of effectiveness of conservative therapy;
- thromboembolism of the pulmonary artery or major branches;
- severe hypotension.
For pulmonary embolism, 2 types of operations are performed:
- embolectomy - removal of thrombotic masses, used in acute form of pulmonary embolism;
- endarterectomy – removal of the inner wall of a vessel in chronic pulmonary embolism.
Installation of a vena cava filter avoids thromboembolism in patients at high risk of relapse. The device is a special mesh that is placed in the lumen of the inferior vena cava. Thrombotic masses cannot pass through it and reach the pulmonary artery. This is an endovascular operation, the doctor performs a puncture and inserts a special catheter into the jugular, subclavian or great saphenous vein, through which the device is delivered to the installation site.
Computed tomography (CT) in the diagnosis of the body
The technical development of the CT method, especially the emergence and introduction of multidetector devices (MSCT), has led to the fact that computed tomography has become an important diagnostic method for suspected pulmonary embolism. Contrast-enhanced CT is increasingly used as the primary method of investigation for pulmonary embolism, especially in those patients in whom pathological changes were detected on chest x-ray and the results of scintigraphic examination are not of diagnostic value.
CT pulmonary angiography can visualize emboli directly and is non-invasive and easy to use. In recent years, computed tomography scanners have been installed in almost all large hospitals, so the method is relatively affordable. Also, CT allows you to obtain additional information regarding an alternative diagnosis, which is a great advantage of this diagnostic method over classical pulmonary angiography and scintigraphy.
Contrast-enhanced spiral CT allows you to contrast the lumen of the pulmonary vessels and see a thrombus in their lumen. After an intercontinental flight, a young man developed acute chest pain and breathing problems. CT scan visualizes thrombus in the anterior segment artery of the left upper lobe ( LA 2) and the anterior segment artery of the right upper lobe ( RA 2).
CT scan for chronic thromboembolism in a 69-year-old patient with pulmonary arterial hypertension. The tomogram visualizes a parietal thrombus with the presence of point calcifications, located parallel to the anterior wall of the right lower interlobar artery.
In most cases where CT is positive for pulmonary emboli, the emboli are multiple and intraluminal filling defects (enhancement defects) are seen in the larger central arteries and in the segmental and subsegmental vessels. Most often, emboli are found on both sides and are localized in the lower lobe arteries. An obvious filling defect in a single segmental or (especially) subsegmental vessel can be difficult to recognize. It must be taken into account that artifacts associated with the partial volume effect may be mistaken for a filling defect in the subsegmental artery.
Since deep vein thrombosis and pulmonary embolism are partial aspects of a single disease, after CT angiopulmonography, CT venography can be performed without additional administration of a contrast agent. In this case, the research time will increase by only a few minutes.